Breast Concerns and Disorders in Adolescent Females
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Breast-Reconstruction-For-Deformities
ASPS Recommended Insurance Coverage Criteria for Third-Party Payers Breast Reconstruction for Deformities Unrelated to AMERICAN SOCIETY OF PLASTIC SURGEONS Cancer Treatment BACKGROUND Burn of breast: For women, the function of the breast, aside from the brief periods when it ■ Late effect of burns of other specified sites 906.8 serves for lactation, is an organ of female sexual identity. The female ■ Acquired absence of breast V45.71 breast is a major component of a woman’s self image and is important to her psychological sense of femininity and sexuality. Both men and women TREATMENT with abnormal breast structure(s) often suffer from a severe negative A variety of reconstruction techniques are available to accommodate a impact on their self esteem, which may adversely affect his or her well- wide range of breast defects. The technique(s) selected are dependent on being. the nature of the defect, the patient’s individual circumstances and the surgeon’s judgment. When developing the surgical plan, the surgeon must Breast deformities unrelated to cancer treatment occur in both men and correct underlying deficiencies as well as take into consideration the goal women and may present either bilaterally or unilaterally. These of achieving bilateral symmetry. Depending on the individual patient deformities result from congenital anomalies, trauma, disease, or mal- circumstances, surgery on the contralateral breast may be necessary to development. Because breast deformities often result in abnormally achieve symmetry. Surgical procedures on the opposite breast may asymmetrical breasts, surgery of the contralateral breast, as well as the include reduction mammaplasty and mastopexy with or without affected breast, may be required to achieve symmetry. -

Spectrum of Benign Breast Diseases in Females- a 10 Years Study
Original Article Spectrum of Benign Breast Diseases in Females- a 10 years study Ahmed S1, Awal A2 Abstract their life time would have had the sign or symptom of benign breast disease2. Both the physical and specially the The study was conducted to determine the frequency of psychological sufferings of those females should not be various benign breast diseases in female patients, to underestimated and must be taken care of. In fact some analyze the percentage of incidence of benign breast benign breast lesions can be a predisposing risk factor for diseases, the age distribution and their different mode of developing malignancy in later part of life2,3. So it is presentation. This is a prospective cohort study of all female patients visiting a female surgeon with benign essential to recognize and study these lesions in detail to breast problems. The study was conducted at Chittagong identify the high risk group of patients and providing regular Metropolitn Hospital and CSCR hospital in Chittagong surveillance can lead to early detection and management. As over a period of 10 years starting from July 2007 to June the study includes a great number of patients, this may 2017. All female patients visiting with breast problems reflect the spectrum of breast diseases among females in were included in the study. Patients with obvious clinical Bangladesh. features of malignancy or those who on work up were Aims and Objectives diagnosed as carcinoma were excluded from the study. The findings were tabulated in excel sheet and analyzed The objective of the study was to determine the frequency of for the frequency of each lesion, their distribution in various breast diseases in female patients and to analyze the various age group. -

Unresolved, Atraumatic Breast Hematoma: Post-Irradiation Or Secondary Breast Angiosarcoma
Breast Disease 33 (2011/2012) 139142 139 DOI 10.3233/BD-2012-0331 IOS Press Case Report Unresolved, atraumatic breast hematoma: Post-irradiation or secondary breast angiosarcoma Glenn Hanna, Samuel J. Lin, Michael D. Wertheimer and Ranjna Sharma Department of Surgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA Department of Plastic and Reconstructive Surgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA Abstract. Post-irradiation or secondary angiosarcoma of the breast was rst described in the 1980s in patients treated with breast conserving therapy for cancer. The primary management of radiation-induced breast angiosarcoma has focused on surgical resection with an emphasis on achieving negative tumor margins. While surgery remains a key component of treatment, novel therapeutic approaches have surfaced. Despite such advances in treatment, prognosis remains poor. Keywords: Breast cancer, breast conservation therapy, secondary angiosarcoma 1. Clinical scenario amination showed the left breast to be larger than the right, with a 10 15cm areaofa clinicalhematomalo- A 64-year-old post-menopausal Caucasian female cated in the superior and inferior outer quadrants. The presented to our institution with a seven month history overlying skin was hemorrhagic, necrotic and had in- of an unresolved left breast hematoma. Of note, she durated features with areas of active bleeding. Initially, had a history of left breast inltrating ductal carcinoma no discrete underlying mass was identied on physical that was Her-2/Neu negative with estrogen and proges- examination. Areas of peau de orange surrounded the terone receptor positivity seven years prior. She had lesion. She had no palpable lymphadenopathy. -

How to Manage 'Breast' Pain
How to Manage ‘Breast’ Pain. Breast pain is the commonest presenting breast complaint to GPs and the commonest reason for referral to the Breast Unit. Nearly 70% of women develop breast pain at some point in their lives but in only 1% of patients with true breast pain is it related to breast cancer. It is however a major source of worry and anxiety for patients, with many convinced they have breast cancer. The anxiety caused can perpetuate the symptoms and for some lead to psychological morbidity such as loss of self‐esteem and depression. Breast pain can be divided into cyclical and non‐cyclical breast pain with non‐cyclical being divided into true breast pain and referred pain. Cyclical breast pain Younger women often present because of an increase or change in the pain they normally experience before or during a period. Seventy‐five per cent of women with breast pain have cyclical breast pain worse around the time of menstruation. This is linked to changes in hormone levels and mainly affects premenopausal women. It may be associated with heaviness, tenderness, pricking or stabbing pains and can affect one or both breasts or the axillae. This type of pain is common and often self‐limiting. It usually stops after the menopause unless HRT is taken. Non‐cyclical breast pain Non‐cyclical breast pain is continuous pain not related to the menstrual cycle. It is either true breast pain or extra mammary pain that feels as if it is coming from the breast. The majority of non‐cyclical pain seen in clinic is non‐breast and originates from the chest wall e.g. -

Breastfeeding and Women's Mental Health
BREASTFEEDING AND WOMEN’S MENTAL HEALTH Julie Demetree, MD University of Arizona Department of Psychiatry Disclosures ◦ Nothing to disclose, currently paid by Banner University Medical Center, and on faculty at University of Arizona. Goals and Objectives ◦ Review the basic physiology involved in breastfeeding ◦ Learn about literature available regarding mood, sleep and breastfeeding ◦ Know the resources available to refer to regarding pharmacology and breast feeding ◦ Understand principles of psychopharmacology involved in breastfeeding, including learning about some specific medications, to be able to counsel a woman and obtain informed consent ◦ Be aware of syndrome described as Dysphoric Milk Ejection Reflex Lactation Physiology https://courses.lumenlearning.com/boundless-ap/chapter/lactation/ AAP Material on Breastfeeding AAP: Breastfeeding Your Baby 2015 AAP Material on Breastfeeding AAP: Breastfeeding Your Baby 2015 A Few Numbers ◦ About 80% of US women breastfeed ◦ 10-15% of women suffer from post partum depression or anxiety ◦ 1-2/1000 suffer from post partum psychosis Depression and Infant Care ◦ Depressed mothers are: ◦ More likely to misread infant cues 64 ◦ Less likely to read to infant ◦ Less likely to follow proper safety measures ◦ Less likely to follow preventative care advice 65 Depression is Associated with Decreased Chance of Breastfeeding ◦ A review of 75 articles found “women with depressive symptomatology in the early postpartum period may be at increased risk for negative infant-feeding outcomes including decreased breastfeeding duration, increased breastfeeding difficulties, and decreased levels of breastfeeding self-efficacy.” 1 Depressive Symptoms and Risk of Formula Feeding ◦ An Italian study with 592 mothers participating by completing the Edinburgh Postnatal Depression Scale immediately after delivery and then feeding was assessed at 12-14 weeks where asked if breast, formula or combo feeding. -

Congenital Problems in the Pediatric Breast Disclosure
3/20/2019 Congenital Problems in the Pediatric Breast Alison Kaye, MD, FACS, FAAP Associate Professor Pediatric Plastic Surgery Children’s Mercy Kansas City © The Children's Mercy Hospital 2017 1 Disclosure • I have no relevant financial relationships with the manufacturers(s) of any commercial products(s) and/or provider of commercial services discussed in this CME activity • I do not intend to discuss an unapproved/investigative use of a commercial product/device in my presentation 1 3/20/2019 Pediatric Breast • Embryology • Post-natal development • Hyperplasia • Hypoplasia • Deformation Embryology 4th week of gestation: 2 ridges of thickened ectoderm appear on the ventral surface of the embryo between the limb buds 2 3/20/2019 Embryology By the 6th week ridges disappear except at the level of the 4th intercostal space Breast Embryology In other species multiple paired mammary glands develop along the ridges – Varies greatly among mammalian species – Related to the number of offspring in each litter 3 3/20/2019 Neonatal Breast • Unilateral or bilateral breast enlargement seen in up to 70% of neonates – Temporary hypertrophy of ductal system • Circulating maternal hormones • Spontaneous regression within several weeks Neonatal Breast • Secretion of “witches’ milk” – Cloudy fluid similar to colostrum – Water, fat, and cellular debris • Massaging breast can exacerbate problem – Persistent breast enlargement – Mastitis – Abscess 4 3/20/2019 Thelarche • First stage of normal secondary breast development – Average age of 11 years (range 8-15 years) • Estradiol causes ductal and stromal tissue growth • Progesterone causes alveolar budding and lobular growth Pediatric Breast Anomalies Hyperplastic Deformational Hypoplastic 5 3/20/2019 Pediatric Breast Anomalies Hyperplastic Deformational Hypoplastic Polythelia Thoracostomy Athelia Polymastia Thoracotomy Amazia Hyperplasia Tumor Amastia Excision Thermal Tumors Poland Injury Syndrome Tuberous Gynecomastia Penetrating Injury Deformity Adapted from Sadove and van Aalst. -

Lupus Mastitis
Published online: 2021-07-31 SPECIAL SYMPOSIUM - BREAST Lupus mastitis - peculiar radiological and pathological features Abdul Majid Wani, Waleed Mohd Hussain, Mohamed I Fatani, Bothaina Abdul Shakour Department of Radiology, Hera General Hospital, Makkah-10513, Saudi Arabia Correspondence: Dr Abdul Majid Wani, Hera General Hospital, Makkah-105 13, Saudi Arabia, E-mail: [email protected] Abstract Lupus mastitis is a form of lupus profundus that is seen in patients with systemic lupus erythematosus. It usually presents as a swelling (or swellings) in the breasts, with or without pain. The condition is recurrent and progresses along with the underlying disease, with fat necrosis, calcification, fibrosis, scarring, and breast atrophy. Lupus mastitis is often confused with malignancy and lymphoma and, in our part of the world, with tuberculosis. Confusion is especially likely when it occurs in an unusual clinical setting. In this article, we present a case that presented with unique radiological, pathological, and clinical features. Awareness of the various manifestations of lupus mastitis is essential if unnecessary interventions such as biopsies and surgeries, and their consequences, are to be avoided. Key words: Biopsy; lupus mastitis; lupus profundus; mammography; fine needle aspiration cytology; systemic lupus erythematosus Introduction hospital) was present and the patient reported that she had received antituberculous medication for 1 month at that Systemic lupus erythematosus (SLE) is a multisystem, time. Two 1 × 1.5 cm lymph nodes were present in the left autoimmune disorder. Involvement of the subcutaneous axillary region. The left breast revealed multiple lumps, the fat was termed as lupus profundus by Iregang.[1] Lupus biggest being 4 × 3 cm in size. -

Vasospasm of the Nipple
Vasospasm of the Nipple A spasm of blood vessels (vasospasm) in the nipple can result in nipple and/or breast pain, particularly within 30 minutes after a breastfeeding or a pumping session. It usually happens after nipple trauma and/or an infection. Vasospasms can cause repeated disruption of blood flow to the nipple. Within seconds or minutes after milk removal, the nipple may turn white, red, or purple, and a burning or Community stabbing pain is felt. Occasionally women feel a tingling sensation or itching. As the Breastfeeding nipple returns to its normal color, a throbbing pain may result. Color change is not Center always visible. 5930 S. 58th Street If there is a reason for nipple damage (poor latch or a yeast overgrowth), the cause (in the Trade Center) Lincoln, NE 68516 needs to be addressed. This can be enough to stop the pain. Sometimes the (402) 423-6402 vasospasm continues in a “vicious” cycle, as depicted below. While the blood 10818 Elm Street vessels are constricted, the nipple tissue does not receive enough oxygen. This Rockbrook Village causes more tissue damage, which can lead to recurrent vasospasm, even if the Omaha, NE 68144 (402) 502-0617 original cause of damage is “fixed.” For additional information: (Poor Latch or Inflammation) www ↓ Tissue Damage ↙ ↖ Spasm of blood vessels → Lack of oxygen to tissues To promote improved blood flow and healing of the nipple tissue: • See a lactation consultant (IBCLC) or a breastfeeding medicine specialist for help with latch and/or pumping to reduce future nipple damage. • When your baby comes off your nipple, or you finish a pumping session, immediately cover your nipple with a breast pad or a towel to keep it warm and dry. -

Massachusetts Breastfeeding Resource Guide
Massachusetts Breastfeeding Resource Guide 2008 Edition © 254 Conant Road Weston, MA 02493 781 893-3553 Fax 781 893-8608 www.massbfc.org Massachusetts Breastfeeding Coalition Leadership Chair Board Member Melissa Bartick, MD, MS Lauren Hanley, MD Treasurer Board Member Gwen MacCaughey Marsha Walker, RN, IBCLC NABA, Lactation Associates Clerk Xena Grossman, RD, MPH Board Member Anne Merewood, MPH, IBCLC Board Member Lucia Jenkins, RN, IBCLC La Leche League of MA RI VT 10th edition (2008) Compiled and edited by Rachel Colchamiro, MPH, RD, LDN, CLC and Jan Peabody Cover artwork courtesy of Peter Kuper Funding for the printing and distribution of the Massachusetts Breastfeeding Resource Guide is provided by the Massachusetts Department of Public Health-Bureau of Family and Community Health, Nutrition Division. Permission is granted to photocopy this guide except for the three reprinted articles from the American Academy of Pediatrics and two articles from the American Academy of Family Physicians. Adapted from the Philadelphia Breastfeeding Resource Handbook. hhhhhhhhhhhhhhhhhhhhTable of Contents Organizational statements on breastfeeding…………………………………………………………….2 Breastfeeding and the Use of Human Milk, American Academy of Pediatrics…………………….6 Breastfeeding Position Paper, American Academy of Family Physicians……………………...…19 Breastfeeding initiatives………………………...……………………………………………………...…37 Breastfeeding support and services…………………………………………...………………...…....…39 La Leche League International leaders………….…………………………………………………...….40 Lactation consultants………………………………………………………………………………….…..44 -

Mifepristone
Mifepristone sc-203134 Material Safety Data Sheet Hazard Alert Code EXTREME HIGH MODERATE LOW Key: Section 1 - CHEMICAL PRODUCT AND COMPANY IDENTIFICATION PRODUCT NAME Mifepristone STATEMENT OF HAZARDOUS NATURE CONSIDERED A HAZARDOUS SUBSTANCE ACCORDING TO OSHA 29 CFR 1910.1200. NFPA FLAMMABILITY1 HEALTH0 HAZARD INSTABILITY0 SUPPLIER Company: Santa Cruz Biotechnology, Inc. Address: 2145 Delaware Ave Santa Cruz, CA 95060 Telephone: 800.457.3801 or 831.457.3800 Emergency Tel: CHEMWATCH: From within the US and Canada: 877-715-9305 Emergency Tel: From outside the US and Canada: +800 2436 2255 (1-800-CHEMCALL) or call +613 9573 3112 PRODUCT USE ■ Steroid. Abortifacient steroid. Progesterone receptor antagonist. Binds strongly to progesterone and glucocorticoid recptors, weakly to androgen receptors, but has no anti-oestrogenic or mineralocorticoid activity. Inhibits ovulation when given in the late follicular phase of the menstrual cycle. SYNONYMS C29-H35-N-O2, C29-H35-N-O2, "estra-4, 9-diene-3-one, ", "estra-4, 9-diene-3-one, ", "11-[4-(dimethylamino)phenyl]-17- hydroxy-17-(1-propynyl)-, (11beta, ", 17beta)-, "11-[4-(dimethylamino)phenyl]-17-hydroxy-17-(1-propynyl)-, (11beta, ", 17beta)-, 17beta-hydroxy-11beta-(4-dimethylaminophenyl-1)-, "17alpha-(prop-1-ynyl)oestra-4, 9-dien-3-one", "17alpha-(prop- 1-ynyl)oestra-4, 9-dien-3-one", Mifegyn, R-38486, R-38486, "RU 486", RU-486-6, "RU 38486", "abortifacient oestrogen/ estrogen steroid", "morning after pill" Section 2 - HAZARDS IDENTIFICATION CANADIAN WHMIS SYMBOLS EMERGENCY OVERVIEW RISK May impair fertility. May cause harm to the unborn child. Toxic to aquatic organisms, may cause long-term adverse effects in the aquatic environment. -

The Ins and Outs of Inverted Nipple Repair
The Ins and Outs of Inverted Nipple Repair plasticsurgerypractice.com/2009/11/the-ins-and-outs-of-inverted-nipple-repair/ The proper appearance of the breast and the nipple can be very important to women and men alike. An inverted nipple, something that women may notice increasing at the onset of puberty, is something that can be rectified with a simple 15-minute surgical procedure. PSP recently spoke with M. Mark Mofid, MD, FACS, a plastic surgeon in La Jolla, Calif, about the various techniques of inverted nipple surgery as well as nipple reduction. Mofid is a staff surgeon at several California hospitals, including Scripps Memorial Hospital in La Jolla, Palomar Medical Center in Escondido, and Sharp Chula Vista Medical Center. In addition, he serves on the clinical faculty of the University of California, San Diego, Division of Plastic Surgery. He earned his undergraduate degree magna cum laude from Harvard University. He then attended The Johns Hopkins University School of Medicine, where he completed his medical degree training in general surgery and plastic surgery, and well as completed an advanced craniofacial research fellowship. PSP: How new is the inverted nipple procedure, and how popular is it? Mofid: Numerous techniques have been described over the last several decades for inverted nipple repair. In my own practice, at least one to two patients per month request this procedure. PSP: Are there different types of inverted nipple surgery and different ways of performing the surgery? Mofid: Virtually all techniques involve some variation of a release of the nipple from its basilar attachments. Fixation (whether internal or external) prevents the nipple from re-retracting during the healing process. -
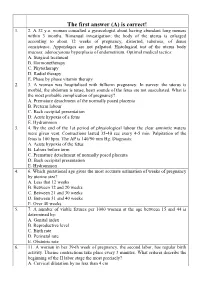
The First Answer (A) Is Correct! 1
The first answer (A) is correct! 1. 2. A 32 y.o. woman consulted a gynecologist about having abundant long menses within 3 months. Bimanual investigation: the body of the uterus is enlarged according to about 12 weeks of pregnancy, distorted, tuberous, of dense consistence. Appendages are not palpated. Histological test of the uterus body mucosa: adenocystous hyperplasia of endometrium. Optimal medical tactics: A. Surgical treatment B. Hormonetherapy C. Phytotherapy D. Radial therapy E. Phase by phase vitamin therapy 2. 3. A woman was hospitalised with fullterm pregnancy. In survey: the uterus is morbid, the abdomen is tense, heart sounds of the fetus are not auscultated. What is the most probable complication of pregnancy? A. Premature detachment of the normally posed placenta B. Preterm labour C. Back occipital presentation D. Acute hypoxia of a fetus E. Hydramnion 3. 4. By the end of the 1st period of physiological labour the clear amniotic waters were given vent. Contractions lasted 35-40 sec every 4-5 min. Palpitation of the fetus is 100 bpm. The AP is 140/90 mm Hg. Diagnosis: A. Acute hypoxia of the fetus B. Labors before term C. Premature detachment of normally posed placenta D. Back occipital presentation E. Hydramnion 4. 6. Which gestational age gives the most accurate estimation of weeks of pregnancy by uterine size? A. Less that 12 weeks B. Between 12 and 20 weeks C. Between 21 and 30 weeks D. Between 31 and 40 weeks E. Over 40 weeks 5. 7. A number of viable fetuses per 1000 women at the age between 15 and 44 is determined by: A.