Improving Insight and Awareness in Brain Injury Kristy Easley, M.A., CCC-SLP, CBIS Neurorestorative Learning Objectives
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NEGLECT and ANOSOGNOSIA a CHALLENGE for PSYCHOANALYSIS Psychoanalytic Treatment of Neurological Patients with Hemi-Neglect
Psychoanalytische Perspectieven, 2002, 20, 4: 611-631 NEGLECT AND ANOSOGNOSIA A CHALLENGE FOR PSYCHOANALYSIS Psychoanalytic treatment of neurological patients with hemi-neglect Klaus Röckerath1 Introduction This paper deals with two phenomena often observed in patients with a lesion to the right hemisphere of the brain: neglect and anosognosia. Fol- lowing an overview of the neglect syndrome from a neuroscientific per- spective I will present preliminary results and hypotheses formulated by our group based on the psychoanalytic treatment of seven such patients. It may be somewhat unusual for neurologically impaired patients to undergo psychoanalytic treatment. But in recent years, a combined effort to under- stand the underlying mechanisms of psychic phenomena has evolved in psychoanalysis and the neurosciences. Hence, the field of neuro-psycho- analysis established itself, studying the psychic implications of neurologi- cal damage in order to understand and gain insight into the "psychic appa- ratus", as constructed by Freud, from a different point of view. It is well known that Freud, a trained neurologist, hoped that one day the mecha- nism of psychic functions would be understood from a neurologist's point of view. He was convinced that the answer to the psychic problems he encountered with his patients must be rooted in the matter of the mind: the brain. That is why groups of psychoanalysts and neuroscientists all over the world have begun to exchange news and views about their common interest: the human mind. Both sciences basically deal with the same object. One way psychoanalysts can contribute is by looking at neurologically impaired patients in a psychoanalytic framework to establish what is dif- 1.The Neurops ychoanalytic Study Group Frankfurt/Cologne, Germany. -
Treatment of Unawareness of Deficits in Patients with Acquired Brain Injury
J Head Trauma Rehabil Vol. 29, No. 5, pp. E9–E30 Copyright c 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins Treatment of Unawareness of Deficits in Patients With Acquired Brain Injury: A Systematic Review Anne-Claire Schrijnemaekers, MSc; Sanne M. J. Smeets, MSc; Rudolf W. H. M. Ponds, PhD; Caroline M. van Heugten, PhD; Sascha Rasquin, PhD Objective: To review and evaluate the effectiveness and methodological quality of available treatment methods for unawareness of deficits after acquired brain injury (ABI). Methods: Systematic literature search for treatment studies for unawareness of deficits after ABI. Information concerning study content and reported effectiveness was extracted. Quality of the study reports and methods were evaluated. Results: A total of 471 articles were identified; 25 met inclusion criteria. 16 were uncontrolled or single-case studies. Nine were of higher quality: 2 randomized controlled trials, 5 single case experimental designs, 1 single-case design with pre- and posttreatment measurement, and 1 quasi-experimental controlled design. Overall, interventions consisted of multiple components including education and multimodal feedback on performance. Five of the 9 high-quality studies reported a positive effect of the intervention on unawareness in patients with some knowledge of their impairments. Effect sizes ranged from questionable to large. Conclusion: Patients with ABI may improve their awareness of their disabilities and possibly attain a level at which they personally experience problems when they occur. At present, because of lack of evidence, no recommendation can be made for treatment approaches for persons with severe impairment of self-awareness in the chronic phase of ABI. We recommended developing and evaluating theory-driven interventions specifically focused on disentangling the components of treatment that are successful in improving awareness. -
Visual Perceptual Skills
Super Duper® Handy Handouts!® Number 168 Guidelines for Identifying Visual Perceptual Problems in School-Age Children by Ann Stensaas, M.S., OTR/L We use our sense of sight to help us function in the world around us. It helps us figure out if something is near or far away, safe or threatening. Eyesight, also know as visual perception, refers to our ability to accurately identify and locate objects in our environment. Visual perception is an important component of vision that contributes to the way we see and interpret the world. What Is Visual Perception? Visual perception is our ability to process and organize visual information from the environment. This requires the integration of all of the body’s sensory experiences including sight, sound, touch, smell, balance, and movement. Most children are able to integrate these senses by the time they start school. This is important because approximately 75% of all classroom learning is visual. A child with even mild visual-perceptual difficulties will struggle with learning in the classroom and often in other areas of life. How Are Visual Perceptual Problems Diagnosed? A child with visual perceptual problems may be diagnosed with a visual processing disorder. He/she may be able to easily read an eye chart (acuity) but have difficulty organizing and making sense of visual information. In fact, many children with visual processing disorders have good acuity (i.e., 20/20 vision). A child with a visual-processing disorder may demonstrate difficulty discriminating between certain letters or numbers, putting together age-appropriate puzzles, or finding matching socks in a drawer. -

Metacognitive Awareness Inventory
Metacognitive Awareness Inventory What is Metacognition? The simplest definition of metacognition is “thinking about thinking.” This refers to the “self-regulation” effective learners exhibit, meaning they are aware of their learning process and can measure how efficiently they are learning as they study. Essentially, metacognition involves two simultaneous levels of thought: the first level is the student’s thinking/learning about the specific subject content and the second level is the student’s thinking about his/her learning. A student practicing metacognition would ask him/herself “How am I thinking?” or “Where am I in the learning process? Am I learning/understanding this topic? How could I learn more effectively?” These two levels are: knowledge and regulation. Students who are metacognitively aware demonstrate self-knowledge: They know what strategies and conditions work best for them while they are learning. Declarative, procedural, and conditional knowledge are essential for developing conceptual knowledge (content knowledge). Regulation refers to students’ knowledge about the implementation of strategies and the ability to monitor the effectiveness of their strategies. When students regulate, they are continually developing and monitoring their learning strategies based on their evolving self-knowledge. Complete the Metacognitive Awareness Inventory to assess your metacognitive processes. The Inventory Check True or False for each statement below. After you complete the inventory, use the scoring guide. Contact an Academic Coach at the Academic Support Center at (856) 681-6250 to discuss your results and strategies to increase your metacognitive awareness. True False 1. I ask myself periodically if I am meeting my goals. 2. I consider several alternatives to a problem before I answer. -
Will It Blend? Information Systems and Computer Engineering
Will It Blend? Studying Color Mixing Perception Paulo Duarte Esperanc¸a Garcia Thesis to obtain the Master of Science Degree in Information Systems and Computer Engineering Supervisors: Prof. Dr. Daniel Jorge Viegas Gonc¸alves Prof. Dra. Sandra Pereira Gama Examination Committee Chairperson: Prof. Dr. Antonio´ Manuel Ferreira Rito da Silva Supervisor: Prof. Dr. Daniel Jorge Viegas Gonc¸alves Member of the Committee: Prof. Dr. Manuel Joao˜ Caneira Monteiro da Fonseca November 2016 Acknowledgments First, I want to thank my advisor Professor Daniel Gonc¸alves for his excellent guidance, for always having the availability to teach, help and clarify, for his enormous knowledge and expertise, and for al- ways believing in the best result possible of this Master Thesis. Then, I also want to thank my co-advisor Sandra Gama, for her more-than-valuable inputs on Information Visualization and for opening the path for this dissertation and others to come! Additionally, I would like to thank everyone which somehow contributed for this thesis to happen: everyone who participated either online, or on the laboratory sessions, specially those who did it so willingly, without looking at the rewards. Without them, there would be no validity is this thesis. I must express my very profound gratitude to my family, particularly my mother Ondina and brother Diogo, for providing me with unfailing support and continuous encouragement throughout my years of study and through the process of researching and writing this thesis. This accomplishment would not have been possible without them. Thank you! Finally, to my girlfriend Margarida, my beloved partner, my shelter and support, for all the sleepless nights, sweat and tears throughout the last seven years. -
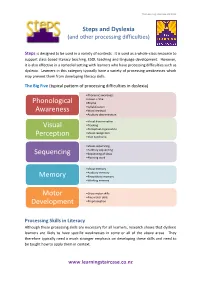
Phonological Awareness Visual Perception Sequencing Memory
The Learning Staircase Ltd 2012 Steps and Dyslexia (and other processing difficulties) Steps is designed to be used in a variety of contexts. It is used as a whole-class resource to support class-based literacy teaching, ESOL teaching and language development. However, it is also effective in a remedial setting with learners who have processing difficulties such as dyslexia. Learners in this category typically have a variety of processing weaknesses which may prevent them from developing literacy skills. The Big Five (typical pattern of processing difficulties in dyslexia) •Phonemic awareness •Onset + rime Phonological •Rhyme •Syllabification Awareness •Word retrieval •Auditory discrimination •Visual discrimination Visual •Tracking •Perceptual organisation •Visual recognition Perception •Irlen Syndrome •Visual sequencing •Auditory sequencing Sequencing •Sequencing of ideas •Planning work •Visual memory •Auditory memory Memory •Kinaesthetic memory •Working memory Motor •Gross motor skills •Fine motor skills Development •Proprioception Processing Skills in Literacy Although these processing skills are necessary for all learners, research shows that dyslexic learners are likely to have specific weaknesses in some or all of the above areas. They therefore typically need a much stronger emphasis on developing these skills and need to be taught how to apply them in context. www.learningstaircase.co.nz The Learning Staircase Ltd 2012 However, there are further aspects which are important, particularly for learners with literacy difficulties, such as dyslexia. These learners often need significantly more reinforcement. Research shows that a non-dyslexic learner needs typically between 4 – 10 exposures to a word to fix it in long-term memory. A dyslexic learner, on the other hand, can need 500 – 1300 exposures to the same word. -

The Riddle of Anosognosia: Does Unawareness of Hemiplegia Involve a Failure to Update Beliefs?
cortex 49 (2013) 1771e1781 Available online at www.sciencedirect.com Journal homepage: www.elsevier.com/locate/cortex Research report The riddle of anosognosia: Does unawareness of hemiplegia involve a failure to update beliefs? Roland Vocat a, Arnaud Saj b and Patrik Vuilleumier a,b,* a Laboratory for Behavioral Neurology & Imaging of Cognition, Department of Neuroscience, Medical School, University of Geneva, Switzerland b Clinic of Neurology, University Hospital of Geneva, Geneva, Switzerland article info abstract Article history: Anosognosia for hemiplegia (AHP) is defined as a lack of awareness for motor incapacity Received 1 February 2012 after a brain lesion. The causes of AHP still remain poorly understood. Many associations Reviewed 10 May 2012 and dissociations with other deficits have been highlighted but no specific cognitive or Revised 30 August 2012 neurological impairment has been identified as a unique causative factor. We hypothe- Accepted 20 October 2012 sized that a failure to update beliefs about current state might be a crucial component of Action editor Giuseppe Vallar AHP. Here, we report results from a new test that are compatible with this view. We Published online 27 November 2012 examined anosognosic and nosognosic brain-damaged patients, as well as healthy con- trols, on a task where they had to guess a target word based on successive clues, with Keywords: increasing informative content. After each clue, participants had to propose a word solu- Anosognosia for hemiplegia tion and rated their confidence. Compared to other participants, anosognosic patients were AHP abnormally overconfident in their responses, even when information from the clues was Awareness insufficient. Furthermore, when presented with new clues incongruent with their previous Denial response, they often stuck to their former “false” beliefs instead of modifying them. -

The Natural Power of Intuition
THE NATURAL POWER OF INTUITION: EXPLORING THE FORMATIVE DIMENSIONS OF INTUITION IN THE PRACTICES OF THREE VISUAL ARTISTS AND THREE BUSINESS EXECUTIVES by Jessica Jagtiani Dissertation Committee: Professor Judith Burton, Sponsor Professor Mary Hafeli Approved by the Committee on the Degree of Doctor of Education Date 16 May 2018 Submitted in partial fulfillment of the requirements for the Degree of Doctor of Education in Teachers College, Columbia University 2018 ABSTRACT THE NATURAL POWER OF INTUITION: EXPLORING THE FORMATIVE DIMENSIONS OF INTUITION IN THE PRACTICES OF THREE VISUAL ARTISTS AND THREE BUSINESS EXECUTIVES Jessica Jagtiani Both artists and business executives state the importance of intuition in their professional practice. Current research suggests that intuition plays a significant role in cognition, decision-making, and creativity. Intuitive perception is beneficial to management, entrepreneurship, learning, medical diagnosis, healing, spiritual growth, and overall well-being, and is furthermore, more accurate than deliberative thought under complex conditions. Accordingly, acquiring intuitive faculties seems indispensable amid present day’s fast-paced multifaceted society and growing complexity. Today, there is an overall rising interest in intuition and an existing pool of research on intuition in management, but interestingly an absence of research on intuition in the field of art. This qualitative-phenomenological study explores the experience of intuition in both professional practices in order to show comparability and extend the base of intuition, while at the same time revealing what is unique about its emergence in art practice. Data gathered from semi-structured interviews and online-journals provided the participants’ experience of intuition and are presented through individual portraits, including an introduction to their work, their worldview, and the experiences of intuition in their lives and professional practice. -

The Mindful Attention Awareness Scale (MAAS)
The Mindful Attention Awareness Scale (MAAS) The trait MAAS is a 15-item scale designed to assess a core characteristic of mindfulness, namely, a receptive state of mind in which attention, informed by a sensitive awareness of what is occurring in the present, simply observes what is taking place. Brown, K.W. & Ryan, R.M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 822-848. Carlson, L.E. & Brown, K.W. (2005). Validation of the Mindful Attention Awareness Scale in a cancer population. Journal of Psychosomatic Research, 58, 29-33. Instructions: Below is a collection of statements about your everyday experience. Using the 1-6 scale below, please indicate how frequently or infrequently you currently have each experience. Please answer according to what really reflects your experience rather than what you think your experience should be. Please treat each item separately from every other item. 1 2 3 4 5 6 almost very somewhat somewhat very almost never always frequently frequently infrequently infrequently _____ 1. I could be experiencing some emotion and not be conscious of it until some time later. _____ 2. I break or spill things because of carelessness, not paying attention, or thinking of something else. _____ 3. I find it difficult to stay focused on what’s happening in the present. _____ 4. I tend to walk quickly to get where I’m going without paying attention to what I experience along the way. _____ 5. I tend not to notice feelings of physical tension or discomfort until they really grab my attention. -

Perception Without Awareness*
PERCEPTION WITHOUT AWARENESS* Fred Dretske We appear to be on the horns of a dilemma with respect to the criteria for consciousness. Phenomenological criteria are valid by definition but do not appear to be scientific by the usual yardsticks. Behavioral criteria are scientific by definition but are not necessarily valid. --Stephen Palmer in Vision Science: Photons to Phenomenology (p. 629) Unknown to Sarah, her neighbor, a person she sees every day, is a spy. When she sees him, therefore, she sees him without awareness of either the fact that he is a spy or the fact that she sees a spy. Why, then, isn't the existence of perception without awareness (or, as some call it, implicit or subliminal perception) a familiar piece of commonsense rather than a contentious issue in psychology?1 It isn't only spies. We see armadillos, galvanometers, cancerous growths, divorcees, and poison ivy without realizing we are seeing any such thing. Most (all?) things can be, and often are (when seen at a distance or bad light), seen without awareness of what is being seen and, therefore, without awareness that one is seeing something of that sort. Why, then, is there disagreement about unconscious perception? Isn't perception without awareness the rule rather than a disputed exception to the rule? I deliberately misrepresent what perception without awareness is supposed to be in order to emphasize an important preliminary point--the difference between awareness of a stimulus (an object of some sort) and awareness of facts about it—including the fact that one is aware of it. -

Assessment and Intervention of Visual Perception and Cognition Following Brain Injury and the Impact on Everyday Functioning
Assessment and Intervention of Visual Perception and Cognition Following Brain Injury and the Impact on Everyday Functioning. Kara Christy, MS, OTRL, CBIS Natasha Huffine, MS, OTRL, CBIS Vision and the Brain •Occipital Lobe • Temporal Lobe • Primary visual cortex • Combines sensory information • Visual association cortex associated with the recognition and identification of objects such • Analyzing orientation, position, and as people, places, and things. movement. • Initiation of Smooth Pursuit Movements • Parietal Lobe • Visual Field Loss • Locating objects • Eye movements • Drawing/construction of objects •Frontal Lobe • Neglect • Saccades and Attention • Movement through space 2 Definitions Visual Perception is the ability to interpret, understand, and define incoming visual information. Form Constancy is the ability to identify objects despite their variation of size, color, shape, position, or texture. Figure ground Perception is the ability to distinguish foreground from background. Visual Closure is the ability to accurately identify objects that are partially covered or missing. Spatial Orientation is the ability to recognize personal position in relation to opposing positions, directions, movement of objects, and environmental locations. Unilateral Inattention is phenomenon that causes one to experience an inability to orient and respond to contralateral visual information. Depth Perception is the ability to perceive relative distance in environmental objects. Visual Memory is the ability to take in a visual stimulus, retain its details, and store for later retrieval. Visual Motor Integration is accurate and quick communication between the eyes and hands. Visuocognition is the ability to use visual information to solve problems, make decisions, and complete planning and organizational tasks through mental manipulation. Executive Functioning is the ability to reason, plan, problem solve, make inferences, and/or evaluate results of actions and decisions. -

Incidence and Diagnosis of Anosognosia for Hemiparesis Revisited B Baier, H-O Karnath
358 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.036731 on 16 February 2005. Downloaded from PAPER Incidence and diagnosis of anosognosia for hemiparesis revisited B Baier, H-O Karnath ............................................................................................................................... J Neurol Neurosurg Psychiatry 2005;76:358–361. doi: 10.1136/jnnp.2004.036731 Background: In previous studies, the incidence of anosognosia for hemiparesis has varied between 17% and 58% in samples of brain damaged patients with hemiparesis. See end of article for Objective: To determine whether this wide variation might be explained by the different criteria used for authors’ affiliations ....................... diagnosing anosognosia. Methods: 128 acute stroke patients with hemiparesis or hemiplegia were tested for anosognosia for Correspondence to: hemiparesis using the anosognosia scale of Bisiach et al. Prof Hans-Otto Karnath, Results: 94% of the patients who were rated as having ‘‘mild anosognosia’’—that is, they did not Centre of Neurology, Hertie-Institute for Clinical acknowledge their hemiparesis spontaneously following a general question about their complaints— Brain Research, University suffered from, and mentioned, other neurological deficits such as dysarthria, ptosis, or headache. of Tu¨bingen, Hoppe- However, they immediately acknowledged their paresis when they were asked about the strength of their Seyler-Str 3, D-72076 Tu¨bingen, Germany; limbs. Their other deficits clearly had a greater