Child Rec Cover Final
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Impact of Food Processing on the Safety Assessment for Proteins Introduced Into Biotechnology-Derived Soybean and Corn Crops ⇑ B.G
Food and Chemical Toxicology 49 (2011) 711–721 Contents lists available at ScienceDirect Food and Chemical Toxicology journal homepage: www.elsevier.com/locate/foodchemtox Review Impact of food processing on the safety assessment for proteins introduced into biotechnology-derived soybean and corn crops ⇑ B.G. Hammond a, , J.M. Jez b a Monsanto Company, Bldg C1N, 800 N. Lindbergh Blvd., St. Louis, Missouri 63167, USA b Washington University, Department of Biology, One Brookings Drive, Campus Box 1137, St. Louis, Missouri 63130, USA article info abstract Article history: The food safety assessment of new agricultural crop varieties developed through biotechnology includes Received 1 October 2010 evaluation of the proteins introduced to impart desired traits. Safety assessments can include dietary risk Accepted 10 December 2010 assessments similar to those performed for chemicals intentionally, or inadvertently added to foods. For Available online 16 December 2010 chemicals, it is assumed they are not degraded during processing of the crop into food fractions. For intro- duced proteins, the situation can be different. Proteins are highly dependent on physical forces in their Keywords: environment to maintain appropriate three-dimensional structure that supports functional activity. Food Biotech crops crops such as corn and soy are not consumed raw but are extensively processed into various food frac- Introduced proteins tions. During processing, proteins in corn and soy are subjected to harsh environmental conditions that Processing soy and corn Denaturation proteins drastically change the physical forces leading to denaturation and loss of protein function. These condi- Dietary exposure tions include thermal processing, changes in pH, reducing agents, mechanical shearing etc. -

University of Ghana, Legon GHANA LEAP 1000 IMPACT EVALUATION E
Institute of Statistical, Social & Economic Research (ISSER), University of Ghana, Legon GHANA LEAP 1000 IMPACT EVALUATION ENDLINE SURVEY HOUSEHOLD INSTRUMENT 2017 1 COVER SHEET ......................................................................................................................................................................................................................................................... 4 FUTURE CONTACT INFORMATION ................................................................................................................................................................................................................... 5 SECTION A1: HOUSEHOLD COMPOSITION CONFIRMATION ....................................................................................................................................................................... 6 SECTION A2: NEW HOUSEHOLD MEMBER ...................................................................................................................................................................................................... 8 SECTION 1: HOUSEHOLD ROSTER .................................................................................................................................................................... Error! Bookmark not defined. SECTION 2: EDUCATION OF ALL HOUSEHOLD MEMBERS AGED 3 YEARS OR OLDER ........................................................................................................................ 9 SECTION 3: HEALTH OF ALL HOUSEHOLD -
Introduction to the Structure of the Ewe Language And"Reasonable Practice" in Speaking
DOCUMENT RESUME ED 028 444 49 AL 001 946 By-Warburton. Irene; And Others Ewe Basic Course. Revised Version. Indiana Univ., Bloomington. African Studies Program.; Peace Corps(Dept. of State), Washington. D.C. Spons Agency-Office of Education (DHEW), Washington. D.C. Bureauof Research. Report No-NDEA-6-602 Bureau No- BR -7-0097 Pub Date 69 Contract- OEC-3- 7-070097-2201 Note- 304p. EDRS Price MF-S125 HC-S15.30 Descriptors- Audiolingual Methods, Cultural Context, *Ewe, Grammar,:*Instructional Materials, *Language Instruction, Pattern Drills (Language). Phonology. Tone Languages The purpose of this beginning text in Ewe is to provide thestudent with an introduction to the structure of the Ewe language and"reasonable practice" in speaking. It is intended to be taught with the assistanceof a native speaker of Ewe. Linguistic terminology is minimal. Suggested teaching time rangesfrom two semesters of class meetings of three hours each week toapproximately 250 hours in an intensive course. The first section of the volume presents abrief description of the language background and some general linguisticfeatures, followed by pre-speed)" phonology drills. The section on grammar presents the basic structures indialogs glossed in English and accompanied by explanatory notes onthe grammar and culture, paragraphs for comprehension practice, andcomprehension and discussion ciuestions. The final section comprises a glossaryof vocabulary used in the text. (AMM) EWE BASICCOURSE Irene Warburton Pro s per Kpotuf e Roland Glover with the helpof Catherine Felten Revised Version & WELFARE HEWN, EDUCMION U.S. DRAMMEN!OF OFFICE OFEDUCMION ME EMILY ASRECEIVED FROM IIAS BEENREPRODUCED MIS DOCUMENI VIEW OROPINIONS ORIGIIIMING II.POINIS OF PERSON ORORGANIZMION OFFICIAL OFFICEOF EDUCMION REPRESENI SIMED DO1101 NECESSARILY P05III011 ORPOLICY. -

The Africa Project a PROGRAM of the ASSOCIATION of YALE ALUMNI
The Africa Project A PROGRAM OF THE ASSOCIATION OF YALE ALUMNI YAMORANSA AND ACCRA, GHANA July 27 – August 7, 2012 (Extension to August 10 – North Ghana) Half NEWSLETTER June 2012 Table of Contents FUN STUFF ............................................................................................................... 1 HARD WORK ........................................................................................................... 1 CHOW TIME! ............................................................................................................ 2 ACTION ITEMS OR WHAT YOU NEED TO DO NOW! ....................................... 4 Fun stuff The purpose of this Newsletter is to let you know that iif you are in town, sometime within the next week you should receive your package of travel goodies from AYA. It should contain: - A hat - A tourbook - A Participant Directory - A bag - Two Luggage Tags - And a Packing List Please bring all the items except the packing list with you on the trip – naturally the luggage tags should be put to their proper use right away. If you have not received the package by July 1, please contact Joao at [email protected] to let him know. Hard Work Thank you to all of those, which is most of you, who have been working so hard to prepare for your projects. Today I received a long list of students – this will be amazing. I will send the list to the education and athletics groups as I soon as I know from Kwame whether we make the class sections or if they will do that. If I haven’t heard by tomorrow, I will send it as is (don’t be overwhelmed – this is opportunity!) Keep those emails flying… The Africa Project NEWSLETTER #5 June 2012 Chow Time! What kind of food will you be eating in Ghana? Wikipedia can tell you all about it with some small annotations from us… There are diverse traditional dishes from each ethnic group, tribe and clan from the north to the south and from the east to west. -
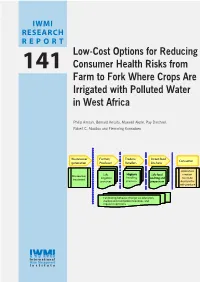
Low-Cost Options for Reducing Consumer Health Risks from Farm to Fork Where Crops Are Irrigated with Polluted Water in West Africa
IWMI Related Publications RESEARCH Drechsel, P.; Graefe, S.; Sonou, M.; Cofie, O. O. 2006. Informal irrigation in urban West Africa: An overview. Colombo, Sri Lanka: International Water Management Institute. 40p. (IWMI Research Report 102). REPOR T www.iwmi.org/Publications/IWMI_Research_Reports/PDF/pub102/RR102.pdf Drechsel, P.; Scott, C. A.; Raschid-Sally, L.; Redwood, M.; Bahri, A. (eds.). 2010. Wastewater irrigation and health: Low-Cost Options for Reducing Assessing and mitigating risks in low-income countries. London, UK: Earthscan; Ottawa, Canada: IDRC; Colombo, Sri Lanka: International Water Management Institute (IWMI), 404p. www.iwmi.org/Publications/books/pdf/Wastewater_Irrigation_and_Health_book.pdf 141 Consumer Health Risks from IWMI (International Water Management Institute). 2006. Recycling realities: Managing health risks to make wastewater an asset. Colombo, Sri Lanka: International Water Management Institute (IWMI). 6p. (IWMI Water Policy Farm to Fork Where Crops Are Briefing 017) www.iwmi.org/Publications/Water_Policy_Briefs/PDF/WPB17.pdf Irrigated with Polluted Water McCartney, M. P.; Boelee, E.; Cofie, O.; Mutero, C. M. 2007. Minimizing the negative environmental and health impacts of agricultural water resources development in sub-Saharan Africa. Colombo, Sri Lanka: International Water Management Institute. 41p. (IWMI Working Paper 117). in West Africa http://www.iwmi.cgiar.org/Publications/Working_Papers/working/WOR117.pdf Raschid-Sally, L.; Jayakody, P. 2008. Drivers and characteristics of wastewater agriculture -

Improving Blood Retinol Concentrations with Complementary Foods Fortified with Moringa Oleifera Leaf Powder – a Pilot Study
YALE JOURNAL OF BIOLOGY AND MEDICINE 91 (2018), pp.83-94. Original Contribution Improving Blood Retinol Concentrations with Complementary Foods Fortified with Moringa oleifera Leaf Powder – A Pilot Study Laurene Boatenga,*, Irene Ashleyb, Agartha Ohemenga, Matilda Asanteb, and Matilda Steiner- Asiedua aDepartment of Nutrition and Food Science, University of Ghana, Accra, Ghana; bDepartment of Nutrition and Dietetics, University of Ghana, Accra, Ghana Vitamin A deficiency (VAD†) remains a major public health issue and is reported to be the cause of about 6 percent of child deaths under the age of 5 years in Africa. Inadequate dietary intake of vitamin A-rich foods is a major cause of VAD. Moringa oleifera leaf powder (MLP) is rich in nutrients particularly vitamin A and its use in infant feeding has been explored. This pilot study was designed to test the efficacy of MLP in improving blood retinol concentrations among infants in a rural district in Ghana. A subset of infants participating in a randomized controlled trial (ISRCTN14377902) were randomly assigned to receive one of the three study foods (MCL-35g and MS-5g both of which were fortified with MLP, and a third food, CF-35g, a cereal legume blend which served as the control food) in a feeding intervention that lasted for 6 weeks. Primary outcome of the pilot study was retinol levels measured in 5 ml of whole blood at baseline and endline using the iCheck™ Fluoro device. A total of 103 infant-mother pairs were recruited at baseline, of which 65 completed the study. All the infants in the study were vitamin A deficient at both baseline and endline when compared to the World Health Organization (WHO) threshold of 0.70µmol/l. -

Full Text (PDF)
Academia Journal of Food Research 1(3): 050-058, September 2013 DOI: http://dx.doi.org/10.15413/ajfr.2012.0117 ISSN: 2315-7763 ©2013 Academia Publishing Research Paper Production and evaluation of weaning meal from fermented red maize fortified with cowpea Accepted 16th June, 2013 ABSTRACT A weaning food blend was prepared from an improved variety of maize (Marggi Red) and cowpea. Standard method was used for the analysis. The protein content Modu S, Ibrahim Z, Hajjagana L, of the weaning blend (12.68±0.45) was not able to meet the recommended Dietary Falmata AS, Babagana M and Allowance of infants of weaning age. The Calcium content of the weaning food Bintu BP blend (50.08±0.09) was compared favorably with commercial weaning food Department of Biochemistry, frisocrem® (52.00). Processing resulted in increase in-vitro protein digestibility Faculty of Science, University (77.91±0.29 to 83.40±1.96) at one hour and (83.93±0.12 to 87.86±0.05) at six of Maiduguri hours of the composite meal. Corresponding author email: [email protected] Key words: red maize, cowpea, nutritional value. INTRODUCTION Weaning is a gradual process of introducing solid foods to food blends. an infant’s diet, alongside breast milk from the age of three to four months, since the breast feeding along cannot meet Maize yields more flour, with much less bran than wheat. the infant nutritional requirement (Salmon et al., 2008). In However, it lacks the protein gluten of wheat and therefore, Nigeria, traditional weaning foods consist of monocereal makes baked food poor rising capability (USDA Nutrient grains, prepared from either millet, maize or sorghum Database, 2009). -

Product Wdevelopfmenatt for Root and T Eubr Crops
'1, Vj 5 -Ifi' .f ..;** L L Product wDevelopfmenatt for Root and T eubr CroPS Volume III - Africa Tropical Agriculture INTERNATIONAL POTATO CENTER (CIP) International Institute of TIHE INTERNATIONAL.POTATo CENTER (CII') is a scientific, aujonomous, and non-profit institution dedicaled to developing and disseminating knowledge for greater use of the potato, swctlpotato, other and tuber crops as baLic ft-×xs in the developing world. ('IP was eslablished by agreement with the Government of Peru and is supported by the Consultative Group on International Agricultural Re.seardh k'tc;AR) whose members provide funding for international agricullural development. TH-lEtI"II ROII('Al, agriculturl research and training institute supported..\;RI('iltIgTIIST: (OIITA)is a non-profit, international primarily by the C(GIAR. IrTA employs about 18) scient ists and prof1essional staff membe rs from over " 41 countries and abou I14X) support staff, mostly from Nigeria. t'os our objectives are: (I) to improve agricultural pr(duction systems for the African humid and subhumid tropics which can be sustained without degradation of the environment; (2) to improve he pcrfonnancc ofseleccd ftod crops which cun be integrated into improved and sustainable production systems; (3) to develop naitional agricultural research capabilities including ces on a ha.sis of sharcd responsibility human rc'';:ur with IITA, by means of training, information, and othcr ctiv outreach itics; and (4) to improvL food quality and availabilit\. including food storage, processing, and marketing. TXQ' '- El, CI:NTRO INTI-:RNA(IONAL, "-LJL'\L A(;RIt't;RTIR ROIAI.( (C IATis) tural research i,'stiution dedicated to the application a developmcnt-oricnted agricul of science towards lasting alleviation of hunger and poverty in developing countries. -

Assessing Rural Consumers' WTP for Orange, Biofortified Maize in Ghana
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Research Papers in Economics Assessing rural consumers’ WTP for orange, biofortified maize in Ghana with experimental auctions and a simulated radio message By De Groote, Hugo; Tomlins, Keith; Haleegoah, Joyce; Awool, Manfred; Frimpong, Benedicta; Banerji, Abijit; Chowdury, Shyamal; and Meenakshi, J. V. Contributed Paper presented at the Joint 3rd African Association of Agricultural Economists (AAAE) and 48th Agricultural Economists Association of South Africa (AEASA) Conference, Cape Town, South Africa, September 19-23, 2010. Assessing rural consumers’ WTP for orange, biofortified maize in Ghana with experimental auctions and a simulated radio message Hugo De Groote1, Keith Tomlins, Joyce Haleegoah, Manfred Awool, Benedicta Frimpong, Abijit Banerji , Shyamal Chowdury, J. V. Meenakshi 1 International Maize and Wheat Improvement Centre, CIMMYT, PO Box 1041-00621 Nairobi, Kenya, [email protected] Paper prepared for submission to the African Agricultural Economics Association Meetings – Cape Town, 19-23 September 2010 Submission to Prof. Nick Vink, [email protected] Abstract Deficiencies of micronutrients such as vitamin A are widespread, expecially in Africa. Biofortified crops such as maize, bred for high levels of provitamin A might offer a solution, but these crops are often bright orange, and African maize consumers prefer white. To estimate the consumers interest in orange biofortified maize, sensory evaluations were organized in rural Ghana with white, yellow and orange maize. The effect of information on willingness to pay for biofortification was estimated using a simulated radio message. Results indicate that color preferences are highly regional, wide variation exist within regions, and the provision of information is able to change these preferences. -

Urban Market Opportunities for High Quality Cassava Products in Ghana
Urban market opportunities for high quality cassava products in Ghana C.C. Collinson1, G. Van Dyck2, S. Gallat1 and A. Westby1 1 Natural Resources Institute, University of Greenwich, Central Avenue, Chatham, Kent ME4 4TB, United Kingdom. 2.Research International, PO Box 01960, Osu, Accra, Ghana ABSTRACT Growing urban populations and changing food preferences potentially offer new market opportunities that could be exploited by rural micro-scale processors and small and medium scale enterprises. This paper reports on a market assessment study conducted in four urban areas in Ghana. It was found that amongst the target group for the survey (young professionals in Living Standards Measure groups 5-8), there was a high willingness to buy into the concept of purchasing hygienically prepared and packaged cassava products. The majority (90%) said that they were likely to purchase. Price, hygienic manufacture and packaging of products were determined to be key criteria for adoption of the products. Acceptable retail price ranges for different product types are reported. INTRODUCTION The production and marketing of traditionally processed cassava products are important income generating activities in many countries in sub-Saharan Africa. As well as creating great social challenges in these countries, urbanisation bringseconomic opportunities, such as the expansion of the middle class and its demand for high quality and convenient foods. This study was carried out to determine the public’s acceptance of hygienically processed and packaged convenient forms of traditional cassava products in Ghana. These products included fufu (non-fermented), gari, kokonte and agbelima. Specifically the study sought to: determine the public’s awareness of hygienically processed and packaged products; establish levels of acceptance; ascertain attitudes towards the products; suggest interventions that can could lead to positive attitudinal change and to determine the optimum price levels for these products. -

“Paddling a Canoe and Preparing Rice Balls”: the Semantics of Tafi Cuisine ______
Bobuafor: “Paddling A Canoe and Preparing Rice Balls”: The Semantics of Tafi Cuisine ________________________________________________________________________ http://dx.doi.org/10.4314/gjl.v7i2.6 “PADDLING A CANOE AND PREPARING RICE BALLS”: THE SEMANTICS OF TAFI CUISINE Mercy Bobuafor Abstract The culinary field is where three of the well-authenticated examples of human universals; tool making, use of fire and cooking of food, come together. Yet in this field, cultures differ in their conceptualisation and linguistic representation of food preparation. In this study, I discuss the language of cooking in Tafi, a Ghana-Togo Mountain Language, focusing on five verbs: tɔ́ “cook, boil”; pʊ́ɩ̄ “bake, roast”, gba “fry, roast; sweep”; ge “cook (e.g. dumpling); drive (e.g. a car)” and tú “pound”. I investigate the semantic relations among them and explore the cultural logic that unites the interpretations suggested by their translation equivalents. Thus, I show that the contextual interpretation of tɔ́ depends on the classes of nouns it collocates with: With kɩ́dɔ̄ “thing” it signals “prepare a meal”. Where its complement is a specific product, the interpretation is “to make something” e.g., tɔ́ bésh(e)ɔkɔ̃ɛ̃ “prepare local soap”. But if the complement names a food then it means “prepare that particular food” e.g. tɔ́ (elí) oni “prepare (oil-palm) soup”. If the complement is a (raw) foodstuff, it is interpreted as “boil in water to”, e.g. tɔ́ kídzē “egg” is interpreted as “cook egg” or “boil egg in water”. Furthermore, I argue that the use of the activity verbs gba “sweep”, ge “drive, paddle” (cf. Akan ka) and tú “pound” in the culinary field is based on the manner of food preparation. -

Ewe Proverbs By
A COLLECTION OF EWE PROVERBS BY CEPHAS YAO AGBEMENU NAIROBI, KENYA: PRIVATELY PRINTED 1 NOVEMBER 2010 1 TABLE OF CONTENTS 1. Abo mekpe na wu ata o. 2. Adaata so ha, mo le eme. 3. Adzofu di aha vuu, amatsi woku ne. 4. Afevemegbo, gbodome wotsina. 5. Afi du ke, Ke mevona le efe nkume o. 6. Afotude memu na De o. 7. Agbavito meduna anyanya o. 8. Agbebadaa metia agbeto o. 9. Agbebadaa metia agbeto o. 10. Ago bia De bia, gake Ago me daa ami o. 11. Agobaya mefoanu dzro o. Yaa do Agome. 12. Ako be nemedi vu o ha, kpo yefe bleme da. 13. Akota gbadzaa melo na hala o. 14. Akpo be yeda de, gake yemekpo ndito hafi yava kpo fie toa. 15. Ale nyemitsi be yele gbome gblem ha, eya nuto fe blenu sako. 16. Ame nutoe nyaa efe Amidolo tata. 17. Ame tso agble gbo medoa ha da o. 18. Amedzro nkugaa, menyaa xodome mo o. 19. Amekuku fotro megbea yome yi o. 20. Amemanoafe fe zemee wodana agbota le. 21. Amenovi menoa atidzi/ Yokuti dzi wodua gbogboa o. 22. Amenutoe nyaa efe avovuvu tata. 23. Asi medina gbedzrogbe o, asidigbe asi dina. 24. Asideka melea Todzo o. 25. Asitoako metsia akota o. 26. Atifufu si tsi moto la, nya le enu. / Atifufu si le motola wome tso ne o. 27. Atoe be yemenyo o ha, dzosagbe ha woayo yi. 28. Avu dufu medua ga o. 29. Avulenu melea Dzata o. 30. Awako metsoa Koklovi wotsoa koklozi dane o. 31. Dadi menoa kevime wodoa aside nu o 32.