Childhood Vaccines in Uganda and Zambia: Determinants and Barriers to Effective Coverage
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Measles in Sudan
Measles in Sudan Diagnosis, Epidemiology and Humoral Immune Response Mazelen in Soedan Diagnostiek, epidemiologie en humorale imuunrespons Thesis to obtain the degree of Doctor from the Erasmus University Rotterdam by command of the Rector Magnificus Prof.dr. S.W.J. Lamberts and according to the decision of the Doctorate Board The public defence shall be held on Wednesday 28 January 2004 at 15.45 hrs by Haja Sittana El Mubarak born at Maryland, USA Doctoral Committee Promotor: Prof.dr. A.D.M.E. Osterhaus Other members: Prof.dr. R. de Groot Prof.dr. E.H.J.H.M. Claassen Prof.dr. C.P. Muller Copromotor: Dr. R.L. de Swart The studies described in this thesis were performed at the department of Virology of the Erasmus MC in Rotterdam, the Netherlands, in close collaboration with the Institute of Endemic Diseases of the University of Khartoum, Sudan. The studies received financial support from INCO-DC grant IC18CT96-0116 from the European Commission. Printing of this thesis was financially supported by: ViroClinics BV, Rotterdam, ViroNovative BV, Rotterdam, Meddens Diagnostics BV, Vorden, DakoCytomation BV, Glostrup. Production: Optima Grafische Communicatie, Rotterdam, The Netherlands To Mohammed and Nimah, my dear parents, lovely family and to Sudan Contents Chapter 1 General Introduction 10 Chapter 2 Diagnosis and molecular epidemiology 23 2.1 Serological and virological characterisation of 25 clinically diagnosed measles cases in suburban Khartoum. J Clin Microbiol 2000;38: 987-991 2.2 Prevention of measles in Sudan: a prospective study 35 on vaccination, diagnosis and epidemiology. Vaccine 2001; 19: 2254-2257 2.3 Genetic characterisation of wild-type measles viruses 41 circulating in suburban Khartoum, 1997-2000. -
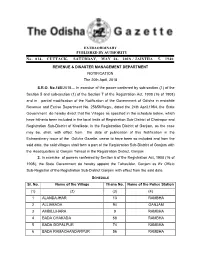
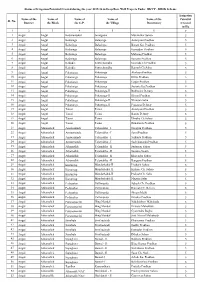
EXTRAORDINARY PUBLISHED by AUTHORITY No
EXTRAORDINARY PUBLISHED BY AUTHORITY No. 814, CUTTACK, SATURDAY, MAY 26, 2018 / JAISTHA 5, 1940 REVENUE & DISASTER MANAGEMENT DEPARTMENT NOTIFICATION The 20th April, 2018 S.R.O. No.185/2018— In exercise of the power conferred by sub-section (1) of the Section 5 and sub-section (1) of the Section 7 of the Registration Act. 1908 (16 of 1908) and in partial modification of the Notification of the Government of Odisha in erstwhile Revenue and Excise Department No. 25656/Regn., dated the 24th April,1964, the State Government do hereby direct that the Villages as specified in the schedule below, which have hitherto been included in the local limits of Registration Sub-District of Chatrapur and Registration Sub-District of Khalikote, in the Registration District of Ganjam, as the case may be, shall, with effect from the date of publication of this Notification in the Extraordinary issue of the Odisha Gazette, cease to have been so included and from the said date, the said villages shall form a part of the Registration Sub-District of Ganjam with the Headquarters at Ganjam Tahasil in the Registration District, Ganjam . 2. In exercise of powers conferred by Section 6 of the Registration Act, 1908 (16 of 1908), the State Government do hereby appoint the Tahasildar, Ganjam as Ex Officio Sub-Registrar of the Registration Sub-District Ganjam with effect from the said date. SCHEDULE Sl. No. Name of the Village Thana No. Name of the Police Station (1) (2) (3) (4) 1 ALANDAJHAR 13 RAMBHA 2 ALLIABADA 94 GANJAM 3 AMBILIJHARA 9 RAMBHA 4 BADA CHAKADA 58 RAMBHA 5 BADA GOPALPUR 74 RAMBHA 6 BADA RAMACHANDARPUR 56 RAMBHA 2 Sl. -

Soccer & Society, Vol
Hay, Roy and McDonald, Heath 2007, A victory for the fans? Melbourne's new football club in recent historical perspective, Soccer & society, vol. 8, no. 2/3, pp. 298-315. This is the postprint version. This is an Accepted Manuscript of an article published by Taylor & Francis in Soccer & society in 2007, available at: http://www.tandfonline.com/10.1080/14660970701224558 ©2007, Taylor & Francis Reproduced by Deakin University with the kind permission of the copyright owner. Available from Deakin Research Online: http://hdl.handle.net/10536/DRO/DU:30007257 A Victory for the fans? Melbourne’s new football club in recent historical perspective.1 Roy Hay and Heath McDonald © Sports and Editorial Services Australia and Deakin University In 2005 a completely new football (soccer) team, the Melbourne Victory, was created in Victoria, Australia to play in a new national league, the A-League.2 Within a year it was drawing more than 50 000 fans to a regular season home game against Sydney FC in a league whose eight participants stretch from Perth, Western Australia to Auckland in New Zealand.3 This was the third time in less than a decade that a new soccer team had been launched in a city which is best known for its devotion to Australian Rules football, cricket and horse racing.4 The other two, Collingwood Warriors and Carlton, lasted one season and three seasons and eight games respectively before collapsing in acrimony and debt. Collingwood and Carlton began with on-field success. Collingwood won the National Soccer League (NSL) cup in 1996–67, -

References for L'affaire Wakefield: Shades Of
REFERENCES FOR L’AFFAIRE WAKEFIELD: SHADES OF DREYFUS 1 Alpha-1-Antitrypsin, Autism, And Coeliac Disease, John Walker-Smith and Judith Andrews, The Lancet, 1972; cited by Professor Walker-Smith in his autobiography, Enduring Memories, 2012, p. 211-3; Perinatal Measles Infection And Subsequent Crohn’s Disease. Ekbom A, Wakefield AJ, Zack M, Adami HO. Lancet 1994; Detection Of Immunoreactive Antigen, With A Monoclonal Antibody To Measles Virus, In Tissue From A Patient With Crohn's Disease, Hiroyuki Miyamoto, Tomoyuki Tanaka, Noritoshi Kitamoto, Yoshihiro Fukuda, Takashi Shimoyama, Journal of Gastroenterology, 1995 2 Closed Financial Loops, Kevin De Jesus-Morales and Vinay Prasad , The Hastings Center, 2017 3 Of Measles and Flu, Editor’s Choice, Fiona Godlee, October 2006 4 The Tamiflu Trials, Editorial by Elizabeth Loder, David Tovey, and Fiona Godlee, BMJ, 2014 5 The Next MMR – Could We Do Better? Fiona Godlee, Head of BMJ Knowledge, power point presentation, British National Formulary, 2004 6 Reflections on Investigating Wakefield, Brian Deer, BMJ, February 2, 2010 7 Deposition of Jane Smith, BMJ Deputy Editor June 28, 2012, Wakefield vs. BMJ (Texas litigation) BMJ 8523, p. 45-46 8 How The Case Against The MMR Vaccine Was Fixed, BMJ, January 6, 2011; How The Vaccine Crisis Was Meant To Make Money, BMJ, January 11, 2011; The Lancet’s Two Days To Bury Bad News, BMJ, January 18, 2011 9 Wakefield’s Article Linking MMR Vaccine And Autism Was Fraudulent , Editorial by Fiona Godlee, Editor-in-Chief; Jane Smith, Deputy Editor; Harvey Marcovitz, Associate Editor, BMJ, January 5, 2011 10 CNN, Anderson Cooper 360 Degrees, January 5, 2011 92 11 Merck’s MMR is the only one used in the U.S. -

Odisha Coast - INDIA 1 1 3 3 2 2 ! Bhadrak Storm - Situation As of 05/05/2019 ! ! Delineation - Overview Map 01
270000 300000 330000 360000 390000 420000 450000 480000 510000 84°40'0"E 85°0'0"E 85°20'0"E 85°40'0"E 86°0'0"E 86°20'0"E 86°40'0"E 87°0'0"E GLIDE number: 2019-000043-IND Activation ID: EMSR357 Int. Charter call ID: 608 Product N.: 01ODISHACOAST, v2 0 0 0 0 0 0 0 0 Odisha Coast - INDIA 1 1 3 3 2 2 ! Bhadrak Storm - Situation as of 05/05/2019 ! ! Delineation - Overview map 01 G Sankh a B Jharkhand West n g r a e h Bengal s m a Angul n Jajpur i Dhenkanal Orissa China N " 0 ' 0 4 M N ° " a 0 Pakistan 0 ' Nepal 2 h ^ Bhutan 0 an 4 adi New Delhi ° 0 2 India 0 0 Odisha Coast Myanmar 0 0 Bay of Bengal 0 0 01 0 0 (! 8 8 2 2 Arabian Sea 2 2 Bay of Bengal Andaman Sri Sea ! Laccadive Lanka Kendrapara Sea Boudh ! ! 80 ! km ! ! Cartographic Information ! Cuttack 1:400000 Full color A1, 200 dpi resolution C ) 0 5 10 20 O 0 C 0 N " 0 0 S T 0 ' km 0 0 0 M U 0 0 2 N " ° 5 5 0 0 O 4 ' 2 2 2 0 5 2 2 - 2 : Grid: WGS 1984 UTM Zone 45N map coordinate system ° S 0 3 2 k 2 Tick marks: WGS 84 geographical coordinate system y M 9 ± 1 e 0 d 2 / ( 5 Legend 0 ! 5 0 ! / / Crisis Information Administrative boundaries Hydrography Transportation 0 4 5 0 Paradip Flooded Area ( Province Coastline Primary Road / (04/05/2019 23:54 UTC, 2 d 05/05/2019 00:18 UTC) 0 Placenames e River Secondary Road 1 General Information M ! 9 Placename Nayagarh y Stream Long-distance railway ! 0 Area of Interest ! k Kandhamal 0 S Lake : 1 - Detail map ! ! 8 O Land Subject to Inundation Sensor Metadata ! ! U M ! ! Jagatsinghpur T S Image Footprint Reservoir C ! O ) C Not Analysed - No data River ! Land use - Land Cover Detail 02 ! Features available in the vector package Puri Consequences within the AOI 0 0 Unit of measurement Affected Total in AOI 0 0 0 0 Flooded area ha 13483.3 0 0 2 2 2 2 Estimated population 2 2 Number of inhabitants 76719 4797016 Settlements Residential No. -

Men's Athlete Profiles 1 49KG – SIMPLICE FOTSALA – CAMEROON
Gold Coast 2018 Commonwealth Games - Men's Athlete Profiles 49KG – SIMPLICE FOTSALA – CAMEROON (CMR) Date Of Birth : 09/05/1989 Place Of Birth : Yaoundé Height : 160cm Residence : Region du Centre 2018 – Indian Open Boxing Tournament (New Delhi, IND) 5th place – 49KG Lost to Amit Panghal (IND) 5:0 in the quarter-final; Won against Muhammad Fuad Bin Mohamed Redzuan (MAS) 5:0 in the first preliminary round 2017 – AFBC African Confederation Boxing Championships (Brazzaville, CGO) 2nd place – 49KG Lost to Matias Hamunyela (NAM) 5:0 in the final; Won against Mohamed Yassine Touareg (ALG) 5:0 in the semi- final; Won against Said Bounkoult (MAR) 3:1 in the quarter-final 2016 – Rio 2016 Olympic Games (Rio de Janeiro, BRA) participant – 49KG Lost to Galal Yafai (ENG) 3:0 in the first preliminary round 2016 – Nikolay Manger Memorial Tournament (Kherson, UKR) 2nd place – 49KG Lost to Ievgen Ovsiannikov (UKR) 2:1 in the final 2016 – AIBA African Olympic Qualification Event (Yaoundé, CMR) 1st place – 49KG Won against Matias Hamunyela (NAM) WO in the final; Won against Peter Mungai Warui (KEN) 2:1 in the semi-final; Won against Zoheir Toudjine (ALG) 3:0 in the quarter-final; Won against David De Pina (CPV) 3:0 in the first preliminary round 2015 – African Zone 3 Championships (Libreville, GAB) 2nd place – 49KG Lost to Marcus Edou Ngoua (GAB) 3:0 in the final 2014 – Dixiades Games (Yaounde, CMR) 3rd place – 49KG Lost to Marcus Edou Ngoua (GAB) 3:0 in the semi- final 2014 – Cameroon Regional Tournament 1st place – 49KG Won against Tchouta Bianda (CMR) -

HIGHSCHOOLS in GANJAM DISTRICT, ODISHA, INDIA Block Type of High Sl
-1- HIGHSCHOOLS IN GANJAM DISTRICT, ODISHA, INDIA Block Type of High Sl. Block G.P. Concerned Village Name of the School Sl. School 1 1 Aska Aska NAC Aska Govt. Girl's High School, Aska Govt. 2 2 Aska Aska NAC Aska Harihar High School, Aska Govt. 3 3 Aska Aska NAC Aska Tech High School, Aska Govt. 4 4 Aska Munigadi G. P. Munigadi U. G. Govt. High School, Munigadi Govt. U.G. 5 5 Aska Mangalpur G. P. Mangalpur Govt. U. G. High School, Mangalpur Govt. U.G. 6 6 Aska Khaira G. P. Babanpur C. S. High School, Babanpur New Govt. 7 7 Aska Debabhumi G. P. Debabhumi G. P. High School, Debabhumi New Govt. 8 8 Aska Gunthapada G. P. Gunthapada Jagadalpur High School, Gunthapada New Govt. 9 9 Aska Jayapur G. P. Jayapur Jayapur High School, Jayapur New Govt. 10 10 Aska Bangarada G. P. Khukundia K & B High School, Khukundia New Govt. 11 11 Aska Nimina G. P. Nimina K. C. Girl's High School, Nimina New Govt. 12 12 Aska Kendupadar G. P. Kendupadar Pragati Bidyalaya, Kendupadar New Govt. 13 13 Aska Baragam Baragam Govt. U.G. High School, Baragam NUG 14 14 Aska Rishipur G.P. Rishipur Govt. U.G. High School, Rishipur NUG 15 15 Aska Aska NAC Aska N. A. C. High School, Aska ULB 16 16 Aska Badakhalli G. P. Badakhalli S. L. N. High School, Badakhalli Aided 17 17 Aska Balisira G. P. Balisira Sidheswar High School, Balisira Aided 18 18 Aska GangapurG. P. K.Ch. Palli Sudarsan High School, K.Ch. -

YONGSTOWN STATE UNIVERSITY ORAL HISTORY PROGRAM World
YONGSTOWN STATE UNIVERSITY ORAL HISTORY PROGRAM World War I1 Personal Experiences O.H. 1816 David Simerlink Interviewed By Elaine Fowler On June 1 1,1996 David J. Simerlink David Simerlink was born in Youngstown, Ohio, September 25, 1923. He attended James Hillman Junior High and Garfield High School. David joined the U.S. Navy Reserves in 1940. He was discharged from the Navy in 1946. While home on leave in Youngstown he married Rita Simerlink on June 25, 1945. After the war he returned to Youngstown. Rita and David have four children, David - 50, Richard - 48, Thomas - 4 1, and Ronald - 39. David was employed by the Youngstown Water Department for ten years, 1970- 1980. He retired in 1980. Simerlink is a member of the St. Nicholas. He is also associated with the AMVETS. He had been a Boy Scout, Cub Scouts, and Explorer leader. His special interests are cutting stamps for the vets and woodworking. Youngstown State University Oral History Department World War I1 O.H. # 1816 Interviewee: DAVID J. SIMERLINK Interviewer: Elaine Fowler Subject: World War II Date: June 11, 1996 EF: David Simerlink at 1917 Lynn Ave in Youngstown, Ohio for the Youngstown State University Oral History Program by Elaine Fowler at approximately 9:27am. Mr. Simerlink? DS: Simerlink, yes. EF: What do you remember about your parents? DS: My parents they were hard workers. My dad worked in the steel mill and my mother was a hard worker. We had, there were seven boys at our house, I have six brothers and my grandmother lived with us. -

P19.E$S 3 Layout 1
SUNDAY, NOVEMBER 16, 2014 SPORTS ‘Don’t think, just play’: MIT engineers football success NEW YORK: The Massachusetts Institute common.” The architect of the school’s because it gives him a chance to “not place in pop culture decades ago when “Four years ago, we didn’t get a lot of of Technology’s reputation of academic new-found gridiron greatness is 42-year- think.” He said it’s natural for MIT players late comedian George Carlin read the people out to the games,” said senior superiority is well chronicled. But the pri- old Chad Martinovich, a soft-spoken to be analytical because their days in scoreline “MIT, 3 to the 4th power.” running back Justin Wallace, who has vate research university is now excelling coach who has the team riding a never- class revolve around problem-solving. No one is suggesting MIT is ready to scored 16 touchdowns this season while in a sector of society once deemed before-seen three-year winning streak. Still, the books versus ball balancing take on undefeated and top-ranked averaging an eyebrow-raising 7.4 yards unthinkable for a bastion of brainpower: He endures the kinds of problems act is a delicate one, he said. “I’m much Mississippi State, as the list of its victims per carry. “We do now.” With 81 Nobel football. you might expect coaching a bunch of more productive during the season,” this year includes Becker College, Salve laureates having ties to MIT, the percep- MIT is undefeated going into its last rocket scientists. “It’s both rewarding and Goldsberry said. -
Sl. No. Name of the District Name of the Block Name of the G.P. Name Of
Status of Irrigation Potential Created during the year 2015-16 in Deep Bore Well Projects Under BKVY - DBSK Scheme Irrigation Name of the Name of Name of Name of Name of the Potential Sl. No. District the Block the G.P. the Village Beneficiary Created in Ha. 12 3 4 5 6 7 1 Angul Angul Badakantakul Jamugadia Muralidhar Sahoo 5 2 Angul Angul Balasinga Balasinga Antaryami Pradhan 5 3 Angul Angul Balasinga Balasinga Basant Ku. Pradhan 5 4 Angul Angul Balasinga Balasinga Kumudini Pradhan 5 5 Angul Angul Balasinga Balasinga Maharag Pradhan 5 6 Angul Angul Balasinga Balasinga Santanu Pradhan 5 7 Angul Angul Kakudia Santarabandha Govinda Ch.Pradhan 5 8 Angul Angul Kakudia Santarabandha Ramesh Ch.Sahu 5 9 Angul Angul Pokatunga Pokatunga Akshaya Pradhan 5 10 Angul Angul Pokatunga Pokatunga Dillip Pradhan 5 11 Angul Angul Pokatunga Pokatunga Gagan Pradhan 5 12 Angul Angul Pokatunga Pokatunga Susanta Ku.Pradhan 5 13 Angul Angul Pokatunga Pokatunga-II Budhadev Dehury 5 14 Angul Angul Pokatunga Pokatunga-II Khirod Pradhan 5 15 Angul Angul Pokatunga Pokatunga-II Niranjan Sahu 5 16 Angul Angul Pokatunga Pokatunga-II Prasanna Dehury 5 17 Angul Angul Tainsi Tainsi Antaryami Pradhan 5 18 Angul Angul Tainsi Tainsi Banita Dehury 5 19 Angul Angul Tainsi Tainsi Dhruba Ch.Sahoo 5 20 Angul Angul Tainsi Tainsi Runakanta Pradhan 5 21 Angul Athamalick Amsarmunda Talamaliha - I Narayan Pradhan 5 22 Angul Athamalick Amsarmunda Talamaliha - I Saroj Pradhan 5 23 Angul Athamalick Amsarmunda Talamaliha - I Srikanta Pradhan 5 24 Angul Athamalick Amsarmunda Talamaliha - I Sachidananda Pradhan 5 25 Angul Athamalick Athamallik Talamaliha - II Sudarsan Sahoo 5 26 Angul Athamalick Athamallik Talamaliha - II Susanta Swain 5 27 Angul Athamalick Athamallik Talamaliha - II Khirendra Sahoo 5 28 Angul Athamalick Athamallik Talamaliha - II Banguru Pradhan 5 29 Angul Athamalick Kurumtap Mandarbahal-II Pitabash Sahoo 5 30 Angul Athamalick Kurumtap Mandarbahal-II Kishore Ch. -

4(4) C: List of Channels Available on the Network
Declaration under Section 4(4) of The Telecommunication (Broadcasting and Cable) Services Interconnection (Addressable Systems) Regulations, 2017 (No. 1 of 2017) 4(4) a: Target market 1. Odisha a. Bhubaneswar , Cuttack , Angul , Paradeep , Dhenkanl , Jagatsinghpur , Balasore , Jaleswar , Baripada , Soro , Bhadrak , Anandpur , Keunjhar , Jharsuguda , Sambalpur , Sonepur , Titlagarh , Bhawanipatna , Balangir , Berhmapur , Rambha , Asika , Khalikote , Puri , Nayagarh , Banki, Nimapara , Narasignhpur , Khurda , Tangi , Balugaon , Rayagada , Jeypure , Damanjodi , Malkangiri , Nabragpur 2. AP / Telengana a. Ichhapur,Palasa,Parwada,Parbatipuram,Kadri,Palconda,Ongole,Kalikiri,Madaksira,Pu ttaparthi,Thorrur,Miralguda,Nalgonda,Bhadrachalam 1. Local Channels considered as 1 SD; 2. Consideration in SD Terms is clarified as 1 SD = 1 SD; 1 HD = 2 SD; 3. Number of channels will vary within the area serviced by a distribution network location depending upon available Bandwidth capacity 4(4) c: List of channels available on the network Count in SD SR NO Channel Name Term SD/HD/LOCAL/REDIO 1 Star Plus 1 SD 2 Star Bharat 1 SD 3 Star Gold 1 SD 4 Star Jalsha 1 SD 5 Maa Movies 1 SD 6 Asianet 1 SD 7 Asianet Movies 1 SD 8 Star Movies 1 SD 9 Star World 1 SD 10 Star sports 1 1 SD 11 Star sports 1 Hindi 1 SD 12 Star Sports 1 Tamil 1 SD 13 Star Sports Select 1 1 SD 14 Star Sports Select 2 1 SD 15 Star Utsav 1 SD 16 Movies ok 1 SD 17 Star Utsav Movies 1 SD 18 Jalsha Movies 1 SD 19 Maa Gold 1 SD 20 Maa Music 1 SD 21 Star Sports 2 1 SD 22 Star Sports 3 1 SD 23 Star -

Health Practitioner Index (HPI) Code Set HISO 10006
Health Practitioner Index (HPI) Code Set HISO 10006 To be used in conjunction with HISO 10005 Health Practitioner Index (HPI) Data Set Copyright information This document has been approved as a standard for the New Zealand Health and Disability sector by the Health Information Standards Organisation (HISO). The copyright owner of this document is the Ministry of Health, which is part of the New Zealand Crown. Ministry of Health work on this document may be reproduced in any number of copies and in any format or medium provided: • the content is not changed • the material is not sold • the material is not used to promote or endorse any product or service • the material is not used in an inappropriate or a misleading context having regard to the nature of the material • any disclaimers included on the published information are reproduced on the material • a copyright acknowledgment to the New Zealand Ministry of Health is included. Permission to reproduce Ministry of Health work does not extend to include any work identified in this document as the copyright material of a party other than the Ministry of Health. Authorisation to reproduce such material must be obtained from the copyright holders concerned. First published in May 2005, updated in July 2008 by the Ministry of Health PO Box 5013, Wellington, New Zealand ISBN 978-0-478-31795-4 (online) This document is available on the HISAC website: http://www.hisac.govt.nz ii Health Practitioner Index (HPI) Code Set v1.2 July 2008 Updates Date Version Page Status Number May 2005 1.0 Published May 2008 1.1 iii - v The New Zealand HPI system – a context document removed, from version 1.0 May 2008 1.1 3 Identifier Type table updated May 2008 1.1 8 Job Role Code Set removed and replaced by link to ANZSCO website.