Rabies Information for Dog Owners
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antibody-Mediated Enhancement of Rabies Virus
542 Nature Vol. 290 16 April 1981 rearranged, K-chain gene, for example; region than the salivary gland mRNA. It is Are these findings at all relevant to the only one of these is destined to appear in possible that this affects the translation rabies 'early death' effect? Rabies viruses the mRNA, the remainder being removed efficiences of the mRNA (see 'Discussion' were thought to be serologically identical, by differential splicing. in Young et al.). Although the explanation but a number of rabies-related viruses are Why does the mouse go to all this for this fascinating genetic mechanism is now knownl2 , and antigenic variation trouble? Any explanation should consider the subject of future work, it is, of course, between rabies virus strains has been estab the fact that a-amylase mRNA accounts likely to be tied up with the primary lished I3 • Mice inoculated with Lagos Bat or for 2 per cent of the cytoplasmic mRNA in question - what determines the different Mokola viruses, two of the rabies-related the salivary gland, but only 0.02 per cent in level of a-amylase in two different tissues? viruses, and subsequently challenged with liver. This level may reflect the transcrip In the rat (and other mammals) the rabies virus, also died more quicklyl4. tion rate from the two genes; the 'salivary situation may be even more complicated. These findings suggest that it is not gland' promoter would then be consider MacDonald and his co-workers (Nature essential to have homologous neutralizing ably stronger than the 'liver' promoter. 287, 17; 1980) have analysed the rat antibodies to produce the rabies 'early Alternatively, the rate of RNA processing a-amylase genes and these studies point to death' effect, but that cross-reacting sera andlor export to the cytoplasm may be at least five non-allelic a-amylase genes or may also be active in this system as in the different for the two mRNAs. -

Bite, Rabies, and Quarantine Information
Rabies and Vaccinations Rabies is a disease caused by a virus (Lyssavirus) found in the saliva of infected animals and is transmitted to other warm- blooded animals, including humans by a bite, scratch or through an open cut. The virus infects Always be alert and know your dog. Watch for signs your dog the central nervous system, causing swelling in is uncomfortable or feeling aggressive and be on the the brain and ultimately death. lookout for potentially dangerous situations. To protect the public, California requires Animal Services to quarantine dogs and cats that have: bitten a human causing a break in the skin, were imported, or exposed to potentially rabid animals, for signs of rabies, for a minimum of 10 days. Dogs are required to be vaccinated for rabies at four months of age. Cats can be vaccinated as early as three months. The first rabies vaccine is What happens during a quarantine? If a dog bite occurs effective for one year. After that initial shot, your Your pet will be placed under quarantine (isolation) 1. Move victim to a safe area. pet should be re-vaccinated every three years. for 10 days to be observed for signs of rabies; this 2. Thoroughly wash the wound with soap and warm Rabies Vaccinations are inexpensive and must allows Animal Services to contain possible rabies water. be administered by a licensed veterinarian. outbreaks. Quarantine can be done at your home if 3. Seek advanced medical aid if necessary; call 9-1-1. Check with Hesperia Animal Services or your authorities are satisfied with the containment area, 4. -

Characterizing and Evaluating the Zoonotic Potential of Novel Viruses Discovered in Vampire Bats
viruses Article Characterizing and Evaluating the Zoonotic Potential of Novel Viruses Discovered in Vampire Bats Laura M. Bergner 1,2,* , Nardus Mollentze 1,2 , Richard J. Orton 2 , Carlos Tello 3,4, Alice Broos 2, Roman Biek 1 and Daniel G. Streicker 1,2 1 Institute of Biodiversity, Animal Health and Comparative Medicine, College of Medical, Veterinary and Life Sciences, University of Glasgow, Glasgow G12 8QQ, UK; [email protected] (N.M.); [email protected] (R.B.); [email protected] (D.G.S.) 2 MRC–University of Glasgow Centre for Virus Research, Glasgow G61 1QH, UK; [email protected] (R.J.O.); [email protected] (A.B.) 3 Association for the Conservation and Development of Natural Resources, Lima 15037, Peru; [email protected] 4 Yunkawasi, Lima 15049, Peru * Correspondence: [email protected] Abstract: The contemporary surge in metagenomic sequencing has transformed knowledge of viral diversity in wildlife. However, evaluating which newly discovered viruses pose sufficient risk of infecting humans to merit detailed laboratory characterization and surveillance remains largely speculative. Machine learning algorithms have been developed to address this imbalance by ranking the relative likelihood of human infection based on viral genome sequences, but are not yet routinely Citation: Bergner, L.M.; Mollentze, applied to viruses at the time of their discovery. Here, we characterized viral genomes detected N.; Orton, R.J.; Tello, C.; Broos, A.; through metagenomic sequencing of feces and saliva from common vampire bats (Desmodus rotundus) Biek, R.; Streicker, D.G. and used these data as a case study in evaluating zoonotic potential using molecular sequencing Characterizing and Evaluating the data. -

Everything You Always Wanted to Know About Rabies Virus ♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣ (But Were Afraid to Ask) Benjamin M
ANNUAL REVIEWS Further Click here to view this article's online features: t%PXOMPBEmHVSFTBT115TMJEFT t/BWJHBUFMJOLFESFGFSFODFT t%PXOMPBEDJUBUJPOT Everything You Always Wanted t&YQMPSFSFMBUFEBSUJDMFT t4FBSDILFZXPSET to Know About Rabies Virus (But Were Afraid to Ask) Benjamin M. Davis,1 Glenn F. Rall,2 and Matthias J. Schnell1,2,3 1Department of Microbiology and Immunology and 3Jefferson Vaccine Center, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, Pennsylvania, 19107; email: [email protected] 2Fox Chase Cancer Center, Philadelphia, Pennsylvania 19111 Annu. Rev. Virol. 2015. 2:451–71 Keywords First published online as a Review in Advance on rabies virus, lyssaviruses, neurotropic virus, neuroinvasive virus, viral June 24, 2015 transport The Annual Review of Virology is online at virology.annualreviews.org Abstract This article’s doi: The cultural impact of rabies, the fatal neurological disease caused by in- 10.1146/annurev-virology-100114-055157 fection with rabies virus, registers throughout recorded history. Although Copyright c 2015 by Annual Reviews. ⃝ rabies has been the subject of large-scale public health interventions, chiefly All rights reserved through vaccination efforts, the disease continues to take the lives of about 40,000–70,000 people per year, roughly 40% of whom are children. Most of Access provided by Thomas Jefferson University on 11/13/15. For personal use only. Annual Review of Virology 2015.2:451-471. Downloaded from www.annualreviews.org these deaths occur in resource-poor countries, where lack of infrastructure prevents timely reporting and postexposure prophylaxis and the ubiquity of domestic and wild animal hosts makes eradication unlikely. Moreover, al- though the disease is rarer than other human infections such as influenza, the prognosis following a bite from a rabid animal is poor: There is cur- rently no effective treatment that will save the life of a symptomatic rabies patient. -

Birmans: What a Unique Breed! PET MEDICAL CENTER
Birmans: What a Unique Breed! Your cat is special! She senses your moods, is curious about your day, and has purred her way into your heart. Chances are that you chose her because you like Birmans (sometimes called “Mitted Cats”) and you expected her to have certain traits that would fit your lifestyle, like: Might "chirrup" or trill her meows to call you when she misses you An affectionate companion and family cat Good with children and other pets Requires minimal grooming Excellent companion However, no cat is perfect! You may have also noticed these characteristics: Needs regular exercise and diet regulation to avoid weight gain Needs the company of other pets or people and does not do well in isolation Exhibits signs of separation anxiety if left alone too much Is it all worth it? Of course! She's full of personality, and you love her for it! She is gentle, friendly and loves to be involved in your daily activities. The origin of the Birman remains a mystery with many unverified tales of their beginnings. Born all white, Birmans do not develop their full color until maturity. They keep their unique white “mittens” on all four paws. Birmans are very social and happy to be involved in your daily activities. They are less apt to climb and jump onto high places, preferring to hang out at ground level or on the couch. Birmans have a playful side and will play fetch or chase when engaged, but prefer to lounge with their family. PET MEDICAL CENTER 501 E. FM 2410 ● Harker Heights, Texas 76548 (254) 690-6769 www.pet-medcenter.com cat's dietary habits is key. -

Bat Rabies and Other Lyssavirus Infections
Prepared by the USGS National Wildlife Health Center Bat Rabies and Other Lyssavirus Infections Circular 1329 U.S. Department of the Interior U.S. Geological Survey Front cover photo (D.G. Constantine) A Townsend’s big-eared bat. Bat Rabies and Other Lyssavirus Infections By Denny G. Constantine Edited by David S. Blehert Circular 1329 U.S. Department of the Interior U.S. Geological Survey U.S. Department of the Interior KEN SALAZAR, Secretary U.S. Geological Survey Suzette M. Kimball, Acting Director U.S. Geological Survey, Reston, Virginia: 2009 For more information on the USGS—the Federal source for science about the Earth, its natural and living resources, natural hazards, and the environment, visit http://www.usgs.gov or call 1–888–ASK–USGS For an overview of USGS information products, including maps, imagery, and publications, visit http://www.usgs.gov/pubprod To order this and other USGS information products, visit http://store.usgs.gov Any use of trade, product, or firm names is for descriptive purposes only and does not imply endorsement by the U.S. Government. Although this report is in the public domain, permission must be secured from the individual copyright owners to reproduce any copyrighted materials contained within this report. Suggested citation: Constantine, D.G., 2009, Bat rabies and other lyssavirus infections: Reston, Va., U.S. Geological Survey Circular 1329, 68 p. Library of Congress Cataloging-in-Publication Data Constantine, Denny G., 1925– Bat rabies and other lyssavirus infections / by Denny G. Constantine. p. cm. - - (Geological circular ; 1329) ISBN 978–1–4113–2259–2 1. -

Eye-Opening Approach to Norovirus Surveillance
LETTERS Rapid collaboration between pub- DOI: 10.3201/eid1608.091380 of norovirus infections in society. lic health authorities in the Philippines We therefore present a new approach and Finland led to appropriate action References to estimate the number of cases and at the site of origin of the rabies case spread of norovirus infections in the 1. Meslin FX. Rabies as a traveler’s risk, es- within a few days. In a country in pecially in high-endemicity areas. J Travel community. which rabies is not endemic, diagnos- Med. 2005;Suppl 1:S30–40. We plotted the number of queries ing rabies and implementing control 2. Srinivasan A, Burton EC, Kuehnert MJ, for *vomit* (asterisks denote any pre- measures in healthcare settings are of- Rupprecht C, Sutker WL, Ksiazek TG, et fi x or suffi x) submitted to the search al. Rabies in Transplant Recipients Inves- ten diffi cult because of limited experi- tigation Team. Transmission of rabies vi- engine on a medical website in Swe- ence with this disease. The last human rus from an organ donor to four transplant den (www.vardguiden.se). This num- rabies case in Finland was diagnosed recipients. N Engl J Med. 2005;352:1103– ber was normalized to account for in 1985, when a bat researcher died 11. DOI: 10.1056/NEJMoa043018 the increasing use of the website over 3. Metlin AE, Rybakov SS, Gruzdev KN, after being bitten by bats abroad and Neuvonen E, Cox J, Huovilainen A. An- time and aggregated by week, starting in Finland (5). For imported cases, pa- tigenic and molecular characterization of with week 40 in 2005. -

Overview, Prevention, and Treatment of Rabies
Overview, Prevention, and Treatment of Rabies Andrea Julia Nigg, Pharm.D., and Pamela L. Walker, Pharm.D. Each year, approximately 55,000 individuals worldwide die from an infection due to the rabies virus. Rabies is a life-threatening disease caused by an RNA virus that is usually transmitted to humans through bites from rabid animals. More recently, reports of transmission by means of organ transplantation have been reported. Since human rabies is nearly 100% fatal if prophylactic measures are not followed, an increased awareness of who should receive prophylaxis and when prophylaxis should be administered is necessary. Preexposure prophylaxis entails the administration of the rabies vaccine to individuals at high risk for exposure to rabies viruses (e.g., laboratory workers who handle infected specimens, diagnosticians, veterinarians, animal control workers, rabies researchers, cave explorers). Preexposure prophylaxis involves a three-dose series of the rabies vaccine that may confer some protection from the virus while simplifying postexposure prophylaxis regimens. Postexposure prophylaxis consists of a multimodal approach to decrease an individual’s likelihood of developing clinical rabies after a possible exposure to the virus. Regimens depend on the vaccination status of the victim and involve a combination of wound cleansing, administration of the rabies vaccine, and administration of human rabies immune globulin. If used in a timely and accurate fashion, postexposure prophylaxis is nearly 100% effective. Once clinical manifestations of rabies have developed, however, treatment options for rabies are limited, and to date, only seven individuals have survived rabies virus infection. Treatment of clinical rabies consists of medical support in an intensive care unit, using a multifaceted approach that includes supportive care, heavy sedation, analgesics, anticonvulsants, and antivirals. -

A Scoping Review of Viral Diseases in African Ungulates
veterinary sciences Review A Scoping Review of Viral Diseases in African Ungulates Hendrik Swanepoel 1,2, Jan Crafford 1 and Melvyn Quan 1,* 1 Vectors and Vector-Borne Diseases Research Programme, Department of Veterinary Tropical Disease, Faculty of Veterinary Science, University of Pretoria, Pretoria 0110, South Africa; [email protected] (H.S.); [email protected] (J.C.) 2 Department of Biomedical Sciences, Institute of Tropical Medicine, 2000 Antwerp, Belgium * Correspondence: [email protected]; Tel.: +27-12-529-8142 Abstract: (1) Background: Viral diseases are important as they can cause significant clinical disease in both wild and domestic animals, as well as in humans. They also make up a large proportion of emerging infectious diseases. (2) Methods: A scoping review of peer-reviewed publications was performed and based on the guidelines set out in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews. (3) Results: The final set of publications consisted of 145 publications. Thirty-two viruses were identified in the publications and 50 African ungulates were reported/diagnosed with viral infections. Eighteen countries had viruses diagnosed in wild ungulates reported in the literature. (4) Conclusions: A comprehensive review identified several areas where little information was available and recommendations were made. It is recommended that governments and research institutions offer more funding to investigate and report viral diseases of greater clinical and zoonotic significance. A further recommendation is for appropriate One Health approaches to be adopted for investigating, controlling, managing and preventing diseases. Diseases which may threaten the conservation of certain wildlife species also require focused attention. -

Rabies Information Sheet
Rabies Information Sheet Compiled from Washington State Deaprtment of Health website Rabies Q&A: What is rabies? Rabies is a severe viral disease that affects the central nervous system. It is almost always fatal. All warm-blooded mammals including humans are susceptible to rabies. What mammals carry rabies? Bats are the only rabies reservoir in the Pacific Northwest. In Washington, rabies has not been found in raccoons, skunks, foxes or coyotes. These species may carry the virus in other regions of the United States. In developing countries, dogs are the principal rabies reservoir. How common is human rabies and what is the source of the rabies virus? Human rabies is an extremely rare disease. Since 1990, the number of reported cases in the United States has ranged from 1 to 6 cases annually. Almost all human rabies cases acquired in the United States since 1980 have been due to bat rabies virus. When human rabies occurs due to exposure outside of the United States it is usually the result of the bite of a rabid dog. Has human rabies occurred in Washington state? There was one fatal case of human rabies in Washington in 1995 and one in 1997. Both were due to bat rabies virus. These cases were the first reported in the state since 1939. How is rabies spread? The rabies virus is found in the saliva of a rabid animal. It is usually spread to humans by animal bites. Rabies could potentially be spread if the virus comes into contact with mucous membranes (eye, nose, and respiratory tract), open cuts, wounds, or abraded skin. -
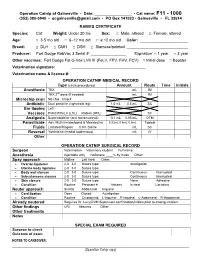
Operation Catnip Medical Records
Operation Catnip of Gainesville • Date: _________________ • Cat name: F11 - 1000 (352) 380-0940 • [email protected] • PO Box 141023 • Gainesville • FL 32614 RABIES CERTIFICATE Species: Cat Weight: Under 20 lbs Sex: □ Male, altered □ Female, altered Age: □ 3-5 mo old □ 6–12 mo old □ ≥ 12 mo old Color: ______________________ Breed: □ DLH □ DMH □ DSH □ Siamese/pointed ____________________________ Producer: Fort Dodge RabVac 3 Serial #: ________________ Expiration: □ 1 year □ 3 year Other vaccines: Fort Dodge Fel-O-Vax LVK III (FeLV, FPV, FHV, FCV) □ Initial dose □ Booster Veterinarian signature: __________________________________ Veterinarian name & license #: __________________________________ OPERATION CATNIP MEDICAL RECORD Type (circle procedures) Amount Route Time Initials Anesthesia TKX mL IM TKX 2nd dose (if needed) mL IM Microchip scan No chip Chip # Antibiotic Dual penicillin (right front leg) 1.0 mL 0.5 mL SC Ear tipping Left Vaccines FVRCP/FeLV (LHL) Rabies (RHL) SC Analgesia Buprenorphine (oral transmucosal) 0.1 mL 0.05 mL OTM Parasiticide Adv. Multi (Imidacloprid & Moxidectin) 0.23mL 0.4mL 0.8mL Topical Fluids Lactated Ringers 0.9% Saline mL SC Reversal Yohimbine (medial saphenous) mL IV Other OPERATION CATNIP SURGICAL RECORD Surgeon Veterinarian Veterinary student Full name: Anesthesia Injectable only Isoflurane ____% by mask Other: Spay approach Midline Left flank Other: Ovarian ligatures 2-0 3-0 Suture type: Autoligation Uterine body ligatures 2-0 3-0 Suture type: Body wall closure 2-0 3-0 Suture type: Continuous Interrupted Subcutaneous closure 2-0 3-0 Suture type: Continuous Interrupted Skin closure 2-0 3-0 Suture type: None Adhesive Condition Routine Pregnant #_______ fetuses In heat Lactating Neuter approach Scrotal Abdominal Inguinal Cord ligation Open Closed Autoligation Condition Routine Cryptorchid: L-Inguinal R-Inguinal L-Abdominal R-Abdominal Already neutered Requires Dr. -
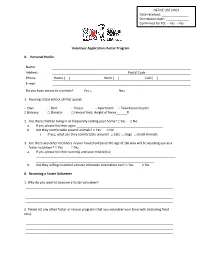
Volunteer Application: Foster Program A. Personal Profile Name
OFFICE USE ONLY Date received: _______________ Orientation date: _____________ Confirmed for FO: □ Yes □ No Volunteer Application: Foster Program A. Personal Profile Name: Address: Postal Code Phone: Home ( ) Work ( ) Cell ( ) E-mail: Do you have access to a vehicle? Yes □ No□ 1. Housing status (check all that apply): □ Own □ Rent □ House □ Apartment □ Townhouse/duplex □ Balcony □ Elevator □ Fenced Yard; Height of fence______ft 2. Are there children living in or frequently visiting your home? □ Yes □ No a. If yes, please list their ages: ________________________________________________ b. Are they comfortable around animals? □ Yes □ No i. If yes, what are they comfortable around? □ Cats □ Dogs □ Small Animals 3. Are there any other members in your household (over the age of 18) who will be assisting you as a foster volunteer? □ Yes □ No a. If yes, please list their name(s) and your relation(s): ______________________________________________________________________________ __________________________________________________________________ b. Are they willing to attend a foster volunteer orientation too? □ Yes □ No B. Becoming a Foster Volunteer 1. Why do you want to become a foster volunteer? 2. Please list any other foster or rescue programs that you volunteer your time with (including feral cats): 3. Please provide a brief description of your experience with very young, ill, injured, or under socialized animals: 5. Please indicate the amount of time per day that you have to dedicate to your foster animal(s): 6. How many hours will your foster animal(s) be alone on a regular basis? 7. We ask foster volunteers to make a commitment of one year to the foster program. Is there anything in the next year that will prevent you from maintaining this commitment (for example: traveling down south for the winter)? 8.