T Cells in Iga Nephropathy: Role in Pathogenesis, Clinical Significance and Potential Therapeutic Target
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Interleukins in Therapeutics
67 ISSN: 2347 - 7881 Review Article Interleukins in Therapeutics Anjan Khadka Department of Pharmacology, AFMC, Pune, India [email protected] ABSTRACT Interleukins are a subset of a larger group of cellular messenger molecules called cytokines, which are modulators of cellular behaviour. On the basis of their respective cytokine profiles, responses to chemokines, and interactions with other cells, these T-cell subsets can promote different types of inflammatory responses. During the development of allergic disease, effector TH2 cells produce IL-4, IL- 5, IL-9, and IL-32. IL-25, IL- 31, and IL-33 contributes to TH2 responses and inflammation. These cytokines have roles in production of allergen-specific IgE, eosinophilia, and mucus. ILs have role in therapeutics as well as diagnosis and prognosis as biomarker in various conditions. Therapeutic targeting of the IL considered to be rational treatment strategy and promising biologic therapy. Keywords: Interleukins, cytokines, Interleukin Inhibitors, Advances INTRODUCTION meaning ‘hormones’. It was Stanley Cohen in Interleukins are group of cytokines that were 1974 who for the first time introduced the term first seen to be expressed by leucocytes and ‘‘cytokine’’. It includes lymphokines, they interact between cells of the immune monokines, interleukins, and colony stimulating systems. It is termed by Dr. Vern Paetkau factors (CSFs), interferons (IFNs), tumor (University of Victoria) in1979.Interleukins (IL) necrosis factor (TNF) and chemokines. The are able to promote cell growth, differentiation, majority of interleukins are synthesized by and functional activation. The question of how helper CD4 T lymphocytes as well as through diverse cell types communicate with each monocytes, macrophages, and endothelial cells. -

Challenges and Approaches for the Development of Safer Immunomodulatory Biologics
REVIEWS Challenges and approaches for the development of safer immunomodulatory biologics Jean G. Sathish1*, Swaminathan Sethu1*, Marie-Christine Bielsky2, Lolke de Haan3, Neil S. French1, Karthik Govindappa1, James Green4, Christopher E. M. Griffiths5, Stephen Holgate6, David Jones2, Ian Kimber7, Jonathan Moggs8, Dean J. Naisbitt1, Munir Pirmohamed1, Gabriele Reichmann9, Jennifer Sims10, Meena Subramanyam11, Marque D. Todd12, Jan Willem Van Der Laan13, Richard J. Weaver14 and B. Kevin Park1 Abstract | Immunomodulatory biologics, which render their therapeutic effects by modulating or harnessing immune responses, have proven their therapeutic utility in several complex conditions including cancer and autoimmune diseases. However, unwanted adverse reactions — including serious infections, malignancy, cytokine release syndrome, anaphylaxis and hypersensitivity as well as immunogenicity — pose a challenge to the development of new (and safer) immunomodulatory biologics. In this article, we assess the safety issues associated with immunomodulatory biologics and discuss the current approaches for predicting and mitigating adverse reactions associated with their use. We also outline how these approaches can inform the development of safer immunomodulatory biologics. Immunomodulatory Biologics currently represent more than 30% of licensed The high specificity of the interactions of immu- biologics pharmaceutical products and have expanded the thera- nomodulatory biologics with their relevant immune Biotechnology-derived peutic options available -
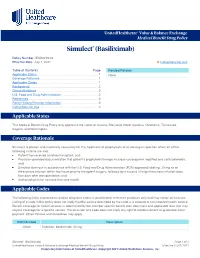
Simulect® (Basiliximab)
UnitedHealthcare® Value & Balance Exchange Medical Benefit Drug Policy Simulect® (Basiliximab) Policy Number: IEXD0219.02 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Policies Applicable States ........................................................................... 1 None Coverage Rationale ....................................................................... 1 Applicable Codes .......................................................................... 1 Background.................................................................................... 2 Clinical Evidence ........................................................................... 2 U.S. Food and Drug Administration ............................................. 2 References ..................................................................................... 2 Policy History/Revision Information ............................................. 2 Instructions for Use ....................................................................... 3 Applicable States This Medical Benefit Drug Policy only applies to the states of Arizona, Maryland, North Carolina, Oklahoma, Tennessee, Virginia, and Washington. Coverage Rationale Simulect is proven and medically necessary for the treatment of prophylaxis of acute organ rejection when all of the following criteria are met: Patient has received a kidney transplant; and Physician provided documentation that patient’s prophylaxis therapy includes cyclosporine modified and corticosteroids; and Simulect -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days. -

B Cell Immunity in Solid Organ Transplantation
REVIEW published: 10 January 2017 doi: 10.3389/fimmu.2016.00686 B Cell Immunity in Solid Organ Transplantation Gonca E. Karahan, Frans H. J. Claas and Sebastiaan Heidt* Department of Immunohaematology and Blood Transfusion, Leiden University Medical Center, Leiden, Netherlands The contribution of B cells to alloimmune responses is gradually being understood in more detail. We now know that B cells can perpetuate alloimmune responses in multiple ways: (i) differentiation into antibody-producing plasma cells; (ii) sustaining long-term humoral immune memory; (iii) serving as antigen-presenting cells; (iv) organizing the formation of tertiary lymphoid organs; and (v) secreting pro- as well as anti-inflammatory cytokines. The cross-talk between B cells and T cells in the course of immune responses forms the basis of these diverse functions. In the setting of organ transplantation, focus has gradually shifted from T cells to B cells, with an increased notion that B cells are more than mere precursors of antibody-producing plasma cells. In this review, we discuss the various roles of B cells in the generation of alloimmune responses beyond antibody production, as well as possibilities to specifically interfere with B cell activation. Keywords: HLA, donor-specific antibodies, antigen presentation, cognate T–B interactions, memory B cells, rejection Edited by: Narinder K. Mehra, INTRODUCTION All India Institute of Medical Sciences, India In the setting of organ transplantation, B cells are primarily known for their ability to differentiate Reviewed by: into long-lived plasma cells producing high affinity, class-switched alloantibodies. The detrimental Anat R. Tambur, role of pre-existing donor-reactive antibodies at time of transplantation was already described in Northwestern University, USA the 60s of the previous century in the form of hyperacute rejection (1). -

Basiliximab Signaling by Therapeutic Antibody Structural Basis for The
Structural Basis for the Blockage of IL-2 Signaling by Therapeutic Antibody Basiliximab This information is current as Jiamu Du, Hui Yang, Dapeng Zhang, Jianchuan Wang, of September 27, 2021. Huaizu Guo, Baozhen Peng, Yajun Guo and Jianping Ding J Immunol 2010; 184:1361-1368; Prepublished online 23 December 2009; doi: 10.4049/jimmunol.0903178 http://www.jimmunol.org/content/184/3/1361 Downloaded from References This article cites 61 articles, 22 of which you can access for free at: http://www.jimmunol.org/content/184/3/1361.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 27, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Structural Basis for the Blockage of IL-2 Signaling by Therapeutic Antibody Basiliximab Jiamu Du,* Hui Yang,*,† Dapeng Zhang,‡ Jianchuan Wang,*,† Huaizu Guo,‡ Baozhen Peng,* Yajun Guo,‡ and Jianping Ding* IL-2 signaling plays a central role in the initiation and activation of immune responses. -

Two-Dose Basiliximab Compared with Two- Dose Daclizumab in Renal Transplantation: a Clinical Study
Copyright ª Blackwell Munksgaard 2006 Clin Transplant 2006: 20: 325–329 DOI: 10.1111/j.1399-0012.2005.00488.x Two-dose basiliximab compared with two- dose daclizumab in renal transplantation: a clinical study Lin M, Ming A, Zhao M. Two-dose basiliximab compared with two-dose Minzhuan Lina,b, Aimin Minga,b and daclizumab in renal transplantation: a clinical study. Ming Zhaoa,b Clin Transplant 2006: 20: 325–329. ª Blackwell Munksgaard, 2006 aOrgan Transplant & Hemopurification Center, China Southern Center of Biological Diagnosis & Abstract: Background: Addition of the interleukin-2 receptor (IL-2R) Therapy, GETDD Hospital, Guangzhou, China, antagonists basiliximab or daclizumab to a calcineurin inhibitor-based bDepartment of Organ Transplantation, Zhujiang regimen significantly reduces risk of acute rejection with a tolerability Hospital, The First Military Medical University, profile similar to a placebo. Use of a truncated two-dose regimen of dac- Guangzhou, China lizumab has been reported, but till date, there has been no controlled study of two-dose daclizumab vs. two-dose basiliximab. Methods: Deceased-donor renal transplant recipients were randomized to basiliximab (20 mg on days 0 and 4) or daclizumab (50 mg on days 1 and 14) with cyclosporine, mycophenolate mofetil and corticosteroids. Flow cytometry was used to calculate the proportion of CD25+ T cells in peripheral blood. Results: Thirty patients were randomized to basiliximab and 28 to dac- Key words: basiliximab – daclizumab – IL-2 – lizumab. There was one patient death in each group, with no other graft IL-2 receptor antagonist – renal transplantation losses. By six months, the incidence of biopsy-proven acute rejection was 0% with basiliximab vs. -

Monoclonal Antibody Therapy and Renal Transplantation: Focus on Adverse Effects
Toxins 2014, 6, 869-891; doi:10.3390/toxins6030869 OPEN ACCESS toxins ISSN 2072-6651 www.mdpi.com/journal/toxins Review Monoclonal Antibody Therapy and Renal Transplantation: Focus on Adverse Effects Gianluigi Zaza 1,*, Paola Tomei 1, Simona Granata 1, Luigino Boschiero 2 and Antonio Lupo 1 1 Renal Unit, Department of Medicine, University-Hospital of Verona, Piazzale A. Stefani 1, Verona 37126, Italy; E-Mails: [email protected] (P.T.); [email protected] (S.G.); [email protected] (A.L.) 2 First Surgical Clinic, Kidney Transplantation Center, University-Hospital of Verona, Piazzale A. Stefani 1, Verona 37126, Italy; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +045-812-2528; Fax: +045-802-7311. Received: 29 November 2013; in revised form: 7 February 2014 / Accepted: 21 February 2014 / Published: 28 February 2014 Abstract: A series of monoclonal antibodies (mAbs) are commonly utilized in renal transplantation as induction therapy (a period of intense immunosuppression immediately before and following the implant of the allograft), to treat steroid-resistant acute rejections, to decrease the incidence and mitigate effects of delayed graft function, and to allow immunosuppressive minimization. Additionally, in the last few years, their use has been proposed for the treatment of chronic antibody-mediated rejection, a major cause of late renal allograft loss. Although the exact mechanism of immunosuppression and allograft tolerance with any of the currently used induction agents is not completely defined, the majority of these medications are targeted against specific CD proteins on the T or B cells surface (e.g., CD3, CD25, CD52). -

Steroid-Refractory Acute GVHD: Lack of Long-Term Improved Survival Using New Generation Anticytokine Treatment
CLINICAL RESEARCH Steroid-Refractory Acute GVHD: Lack of Long-Term Improved Survival Using New Generation Anticytokine Treatment Alienor Xhaard,1 Vanderson Rocha,1,2 Benjamin Bueno,1 Regis Peffault de Latour,1 Julien Lenglet,1 Anna Petropoulou,1 Paula Rodriguez-Otero,1 Patricia Ribaud,1 Raphael Porcher,3 Gerard Socie,1,4 Marie Robin1 There is no consensus on the optimal treatment of steroid-refractory acute graft-versus-host disease (SR-aGVHD) after allogeneic hematopoietic stem cell transplantation. In our center, the treatment policy has changed over time with mycophenolate mofetil (MMF) being used from 1999 to 2003, and etanercept or inolimomab after 2004. An observational study compared survival and infection rates in all consecutive patients receiving 1 of these 3 treatments. Ninety-three patients were included. The main end point was over- all survival (OS). Median age was 37 years. Acute GVHD developed at a median of 15 days after transplanta- tion. Second-line treatment was initiated a median of 12 days after aGVHD diagnosis. Therapies were MMF in 56%, inolimomab in 22%, and etanercept in 23% of the patients. Overall, second-line treatment response rate was 45% (complete response: 28%), MMF: 55%, inolimomab: 35%, and etanercept: 28%. With 74 months median follow-up, the 2-year survival was 30% (95% confidence interval: 22-41). Risk factors significantly associated with OS in multivariate analysis were disease status at transplantation; grade III-IV aGVHD at second-line treatment institution; and liver involvement. None of the second-line therapy influenced this poor outcome. Viral and fungal infections were not statistically different among the 3 treatment options; however, bacterial infections were more frequent in patients treated with anticytokines. -

INN Working Document 05.179 Update 2011
INN Working Document 05.179 Update 2011 International Nonproprietary Names (INN) for biological and biotechnological substances (a review) INN Working Document 05.179 Distr.: GENERAL ENGLISH ONLY 2011 International Nonproprietary Names (INN) for biological and biotechnological substances (a review) Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Essential Medicines and Pharmaceutical Policies (EMP) International Nonproprietary Names (INN) for biological and biotechnological substances (a review) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press through the WHO web site (http://www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Therapeutic Applications of Monoclonal Antibodies
Review Article Therapeutic Applications of Monoclonal Antibodies Prajapati DS, Shah JS, Dave JB, Patel CN Department of Clinical Pharmacy, Shri Sarvajanik Pharmacy College, Mehsana, India ARTICLE INFO ABSTRACT Article history: Monoclonal antibodies drive the development of multibillion dollar biotechnology industry. Many Received 24 March 2010 of the pharmaceuticals companies have entered monoclonal antibodies sector, attracted by quicker Accepted 28 March 2010 and less costly development, higher success rates, premium pricing, and potentially reduced Available online 02 August 2011 threats from generics. The ideal treatment of rheumatoid arthritis (RA) should be safe, produce Keywords: sustained disease remission and stop radiological damage after a brief course of treatment. If Breast cancer, repeated treatments are necessary, they must be safe and economical to use in the long term. It Leukemia, is against these criteria that new treatments for RA, including mAb, should and will be assessed. Monoclonal antibody, Monoclonal antibodies are used in the treatment of cancer, including leukemia, colorectal cancer, Rheumatoid arthritis breast cancer and non-Hodgkin’s lymphoma, RA, ischemic heart disease and transplant rejection. Introduction Cancer therapy Substances foreign to the body, such as disease-causing bacteria Cancer Immunotherapy is the use of the immune system to reject and viruses and other infectious agents, known as antigens, are cancer. The main premise is stimulating the patient’s immune recognized by the body’s immune system as invaders. Our natural system to attack the malignant tumor cells that are responsible defenses against these infectious agents are antibodies, proteins for the disease. This can be either through immunization of the that seek out the antigens and help destroy them.[1,2] patient, in which case the patient’s own immune system is trained Antibodies have two very useful characteristics. -

211 the Impact of Biological Interventions on Health-Related Quality of Life in Adults with Crohn's Disease
211 The impact of biological interventions on health-related quality of life in adults with Crohn's disease The impact of biological interventions on health-related quality of life in adults with Crohn's disease Protocol information Review type: Intervention Review number: 211 Authors Mirjana Stanic Benic1, Vanja Giljaca2, Vera Vlahovic-Palcevski1 1Department of Clinical Pharmacology, Clinical Hospital Centre Rijeka, Rijeka, Croatia 2Directorate of Surgery, Department of Gastroenterology, Heart of England NHS Foundation Trust, Birmingham Heartlands Hospital, Birmingham, UK Citation example: Stanic Benic M, Giljaca V, Vlahovic-Palcevski V. The impact of biological interventions on health- related quality of life in adults with Crohn's disease. Cochrane Database of Systematic Reviews , Issue . Art. No.: . DOI: . Contact person Mirjana Stanic Benic resident in clinical pharmacology and toxicology Department of Clinical Pharmacology Clinical Hospital Centre Rijeka Krešimirova 42 Rijeka 51000 Croatia E-mail: [email protected] Dates Assessed as Up-to-date:Not provided Date of Search: Not provided Next Stage Expected: 28 February 2019 Protocol First Published:Not specified Review First Published: Not specified Last Citation Issue: Not specified What's new Date Event Description History Date Event Description Abstract Background Objectives Search methods Selection criteria Data collection and analysis Main results Authors' conclusions Plain language summary [Summary title] [Summary text] Background Description of the condition 1 / 20 211 The impact of biological interventions on health-related quality of life in adults with Crohn's disease Crohn’s disease (CD) is a relapsing-remitting transmural inflammatory bowel disease (IBD) that may involve any part of the gastrointestinal tract from mouth to anus as well as cause extraintestinal manifestations (skin lesions, arthritis).