4 Chimeric and Humanized Antibodies Have a Longer Circulating Half-Life and Reduced Immunogenicity [Adair, F 2002]. 1.5 Objectiv
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Old and New Challenges in Uveitis Associated with Behçet's Disease
Journal of Clinical Medicine Review Old and New Challenges in Uveitis Associated with Behçet’s Disease Julie Gueudry 1,* , Mathilde Leclercq 2, David Saadoun 3,4,5 and Bahram Bodaghi 6 1 Department of Ophthalmology, Hôpital Charles Nicolle, F-76000 Rouen, France 2 Department of Internal Medicine, Hôpital Charles Nicolle, F-76000 Rouen, France; [email protected] 3 Department of Internal Medicine and Clinical Immunology, AP-HP, Centre National de Références Maladies Autoimmunes et Systémiques Rares et Maladies Autoinflammatoires Rares, Groupe Hospitalier Pitié-Salpêtrière, F-75013 Paris, France; [email protected] 4 Sorbonne Universités, UPMC Univ Paris 06, INSERM, UMR S 959, Immunology-Immunopathology-Immunotherapy (I3), F-75005 Paris, France 5 Biotherapy (CIC-BTi), Hôpital Pitié-Salpêtrière, AP-HP, F-75651 Paris, France 6 Department of Ophthalmology, IHU FOReSIGHT, Sorbonne-AP-HP, Groupe Hospitalier Pitié-Salpêtrière, F-75013 Paris, France; [email protected] * Correspondence: [email protected]; Tel.: +33-2-32-88-80-57 Abstract: Behçet’s disease (BD) is a systemic vasculitis disease of unknown origin occurring in young people, which can be venous, arterial or both, classically occlusive. Ocular involvement is particularly frequent and severe; vascular occlusion secondary to retinal vasculitis may lead to rapid and severe loss of vision. Biologics have transformed the management of intraocular inflammation. However, the diagnosis of BD is still a major challenge. In the absence of a reliable biological marker, diagnosis is based on clinical diagnostic criteria and may be delayed after the appearance of the onset sign. However, therapeutic management of BD needs to be introduced early in order to control inflammation, to preserve visual function and to limit irreversible structural damage. -

Fig. L COMPOSITIONS and METHODS to INHIBIT STEM CELL and PROGENITOR CELL BINDING to LYMPHOID TISSUE and for REGENERATING GERMINAL CENTERS in LYMPHATIC TISSUES
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date Χ 23 February 2012 (23.02.2012) WO 2U12/U24519ft ft A2 (51) International Patent Classification: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, A61K 31/00 (2006.01) CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, PCT/US201 1/048297 KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (22) International Filing Date: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 18 August 201 1 (18.08.201 1) NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, (25) Filing Language: English TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (26) Publication Language: English ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/374,943 18 August 2010 (18.08.2010) US kind of regional protection available): ARIPO (BW, GH, 61/441,485 10 February 201 1 (10.02.201 1) US GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, 61/449,372 4 March 201 1 (04.03.201 1) US ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, (72) Inventor; and EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, ΓΓ, LT, LU, (71) Applicant : DEISHER, Theresa [US/US]; 1420 Fifth LV, MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, Avenue, Seattle, WA 98101 (US). -

Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients
antibodies Review Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients Andrew T. Lucas 1,2,3,*, Ryan Robinson 3, Allison N. Schorzman 2, Joseph A. Piscitelli 1, Juan F. Razo 1 and William C. Zamboni 1,2,3 1 University of North Carolina (UNC), Eshelman School of Pharmacy, Chapel Hill, NC 27599, USA; [email protected] (J.A.P.); [email protected] (J.F.R.); [email protected] (W.C.Z.) 2 Division of Pharmacotherapy and Experimental Therapeutics, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 3 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-919-966-5242; Fax: +1-919-966-5863 Received: 30 November 2018; Accepted: 22 December 2018; Published: 1 January 2019 Abstract: The rapid advancement in the development of therapeutic proteins, including monoclonal antibodies (mAbs) and antibody-drug conjugates (ADCs), has created a novel mechanism to selectively deliver highly potent cytotoxic agents in the treatment of cancer. These agents provide numerous benefits compared to traditional small molecule drugs, though their clinical use still requires optimization. The pharmacology of mAbs/ADCs is complex and because ADCs are comprised of multiple components, individual agent characteristics and patient variables can affect their disposition. To further improve the clinical use and rational development of these agents, it is imperative to comprehend the complex mechanisms employed by antibody-based agents in traversing numerous biological barriers and how agent/patient factors affect tumor delivery, toxicities, efficacy, and ultimately, biodistribution. -

Where Do Novel Drugs of 2016 Fit In?
FORMULARY JEOPARDY: WHERE DO NOVEL DRUGS OF 2016 FIT IN? Maabo Kludze, PharmD, MBA, CDE, BCPS, Associate Director Elizabeth A. Shlom, PharmD, BCPS, SVP & Director Clinical Pharmacy Program Acurity, Inc. Privileged and Confidential August 15, 2017 Privileged and Confidential Program Objectives By the end of the presentation, the pharmacist or pharmacy technician participant will be able to: ◆ Identify orphan drugs and first-in-class medications approved by the FDA in 2016. ◆ Describe the role of new agents approved for use in oncology patients. ◆ Identify and discuss the role of novel monoclonal antibodies. ◆ Discuss at least two new medications that address public health concerns. Neither Dr. Kludze nor Dr. Shlom have any conflicts of interest in regards to this presentation. Privileged and Confidential 2016 NDA Approvals (NMEs/BLAs) ◆ Nuplazid (primavanserin) P ◆ Adlyxin (lixisenatide) ◆ Ocaliva (obeticholic acid) P, O ◆ Anthim (obitoxaximab) O ◆ Rubraca (rucaparib camsylate) P, O ◆ Axumin (fluciclovive F18) P ◆ Spinraza (nusinersen sodium) P, O ◆ Briviact (brivaracetam) ◆ Taltz (ixekizumab) ◆ Cinqair (reslizumab) ◆ Tecentriq (atezolizumab) P ◆ Defitelio (defibrotide sodium) P, O ◆ Venclexta (venetoclax) P, O ◆ Epclusa (sofosburvir and velpatasvir) P ◆ Xiidra (lifitigrast) P ◆ Eucrisa (crisaborole) ◆ Zepatier (elbasvir and grazoprevir) P ◆ Exondys 51 (eteplirsen) P, O ◆ Zinbyrta (daclizumab) ◆ Lartruvo (olaratumab) P, O ◆ Zinplava (bezlotoxumab) P ◆ NETSTPOT (gallium Ga 68 dotatate) P, O O = Orphan; P = Priority Review; Red = BLA Privileged and Confidential History of FDA Approvals Privileged and Confidential Orphan Drugs ◆FDA Office of Orphan Products Development • Orphan Drug Act (1983) – drugs and biologics . “intended for safe and effective treatment, diagnosis or prevention of rare diseases/disorders that affect fewer than 200,000 people in the U.S. -

Interleukins in Therapeutics
67 ISSN: 2347 - 7881 Review Article Interleukins in Therapeutics Anjan Khadka Department of Pharmacology, AFMC, Pune, India [email protected] ABSTRACT Interleukins are a subset of a larger group of cellular messenger molecules called cytokines, which are modulators of cellular behaviour. On the basis of their respective cytokine profiles, responses to chemokines, and interactions with other cells, these T-cell subsets can promote different types of inflammatory responses. During the development of allergic disease, effector TH2 cells produce IL-4, IL- 5, IL-9, and IL-32. IL-25, IL- 31, and IL-33 contributes to TH2 responses and inflammation. These cytokines have roles in production of allergen-specific IgE, eosinophilia, and mucus. ILs have role in therapeutics as well as diagnosis and prognosis as biomarker in various conditions. Therapeutic targeting of the IL considered to be rational treatment strategy and promising biologic therapy. Keywords: Interleukins, cytokines, Interleukin Inhibitors, Advances INTRODUCTION meaning ‘hormones’. It was Stanley Cohen in Interleukins are group of cytokines that were 1974 who for the first time introduced the term first seen to be expressed by leucocytes and ‘‘cytokine’’. It includes lymphokines, they interact between cells of the immune monokines, interleukins, and colony stimulating systems. It is termed by Dr. Vern Paetkau factors (CSFs), interferons (IFNs), tumor (University of Victoria) in1979.Interleukins (IL) necrosis factor (TNF) and chemokines. The are able to promote cell growth, differentiation, majority of interleukins are synthesized by and functional activation. The question of how helper CD4 T lymphocytes as well as through diverse cell types communicate with each monocytes, macrophages, and endothelial cells. -

Review Anti-Cytokine Biologic Treatment Beyond Anti-TNF in Behçet's Disease
Review Anti-cytokine biologic treatment beyond anti-TNF in Behçet’s disease A. Arida, P.P. Sfikakis First Department of Propedeutic Internal ABSTRACT and thrombotic complications (1-3). Medicine Laikon Hospital, Athens, Unmet therapeutic needs in Behçet’s Treatment varies according to type and University Medical School, Greece. disease have drawn recent attention to severity of disease manifestations. Cor- Aikaterini Arida, MD biological agents targeting cytokines ticosteroids, interferon-alpha and con- Petros P. Sfikakis, MD other than TNF. The anti-IL-17 anti- ventional immunosuppressive drugs, Please address correspondence to: body secukinumab and the anti-IL-2 such as azathioprine, cyclosporine-A, Petros P. Sfikakis, MD, receptor antibody daclizumab were not cyclophosphamide and methotrexate, First Department of Propedeutic superior to placebo for ocular Behçet’s and Internal Medicine, are used either alone or in combination Laikon Hospital, in randomised controlled trials, com- for vital organ involvement. During the Athens University Medical School, prising 118 and 17 patients, respec- last decade there has been increased use Ag Thoma, 17, tively. The anti-IL-1 agents anakinra of anti-TNF monoclonal antibodies in GR-11527 Athens, Greece. and canakinumab and the anti-IL-6 patients with BD who were refractory E-mail: [email protected] agent tocilizumab were given to iso- to conventional treatment or developed Received on June 7, 2014; accepted in lated refractory disease patients, who life-threatening complications (4, 5). revised form on September 17, 2014. were either anti-TNF naïve (n=9) or Anti-TNF treatment has been shown to Clin Exp Rheumatol 2014; 32 (Suppl. 84): experienced (n=18). -

Challenges and Approaches for the Development of Safer Immunomodulatory Biologics
REVIEWS Challenges and approaches for the development of safer immunomodulatory biologics Jean G. Sathish1*, Swaminathan Sethu1*, Marie-Christine Bielsky2, Lolke de Haan3, Neil S. French1, Karthik Govindappa1, James Green4, Christopher E. M. Griffiths5, Stephen Holgate6, David Jones2, Ian Kimber7, Jonathan Moggs8, Dean J. Naisbitt1, Munir Pirmohamed1, Gabriele Reichmann9, Jennifer Sims10, Meena Subramanyam11, Marque D. Todd12, Jan Willem Van Der Laan13, Richard J. Weaver14 and B. Kevin Park1 Abstract | Immunomodulatory biologics, which render their therapeutic effects by modulating or harnessing immune responses, have proven their therapeutic utility in several complex conditions including cancer and autoimmune diseases. However, unwanted adverse reactions — including serious infections, malignancy, cytokine release syndrome, anaphylaxis and hypersensitivity as well as immunogenicity — pose a challenge to the development of new (and safer) immunomodulatory biologics. In this article, we assess the safety issues associated with immunomodulatory biologics and discuss the current approaches for predicting and mitigating adverse reactions associated with their use. We also outline how these approaches can inform the development of safer immunomodulatory biologics. Immunomodulatory Biologics currently represent more than 30% of licensed The high specificity of the interactions of immu- biologics pharmaceutical products and have expanded the thera- nomodulatory biologics with their relevant immune Biotechnology-derived peutic options available -

Tocilizumab in the Treatment of Severe and Refractory Parenchymal Neuro
TAB0010.1177/1759720X20971908Therapeutic Advances in Musculoskeletal DiseaseJ Liu, D Yan 971908research-article20202020 Therapeutic Advances in Musculoskeletal Disease Case Series Ther Adv Musculoskel Dis Tocilizumab in the treatment of severe and 2020, Vol. 12: 1–8 DOI:https://doi.org/10.1177/1759720X20971908 10.1177/ refractory parenchymal neuro-Behçet’s 1759720X20971908https://doi.org/10.1177/1759720X20971908 © The Author(s), 2020. Article reuse guidelines: syndrome: case series and literature review sagepub.com/journals- permissions Jinjing Liu* , Dong Yan*, Zhimian Wang, Yunjiao Yang, Shangzhu Zhang, Di Wu, Lingyi Peng, Zhichun Liu and Wenjie Zheng Abstract Correspondence to: Objectives: This study aimed to investigate the efficacy and safety of tocilizumab (TCZ) in Wenjie Zheng severe and refractory parenchymal neuro-Behçet’s syndrome (p-NBS). Department of Rheumatology and Clinical Methods: We retrospectively analyzed five patients with p-NBS treated with TCZ in our center Immunology, Peking Union between 2013 and 2020, and six cases from literature research with the index terms “neuro- Medical College Hospital, Chinese Academy of Behçet’s syndrome” and “tocilizumab” on PubMed NCBI. Medical Sciences & Peking Union Medical Results: A total of 11 patients with p-NBS were enrolled (5 males, 6 females), with a mean College, Key Laboratory of age of 34.5 ± 8.0 years at the onset. All the patients had parenchymal neurological lesions, Rheumatology and Clinical Rheumatology, Ministry six patients (54.5%) suffered from multiple lesions, and nine patients (81.8%) were disabled. of Education, National Clinical Research Center Before TCZ administration, all the patients had failed conventional therapy, eight patients for Dermatologic and (72.7%) received two or more immunosuppressants, and five patients showed insufficient Immunologic Diseases, No. -

Anticorps FR-EN 110X90.Indd
MONOCLONAL ANTIBODIES and Fc fusion proteins for therapeutic use DISTRIBUTION OF INTERNATIONAL NONPROPRIETARY NAMES BY INDICATION SOLID TUMORS RHUMATOLOGY PNEUMOLOGY Lung cancer bevacizumab Rheumatoid arthritis etanercept Allergic asthma omalizumab nivolumab infliximab Severe eosinophilic asthma mepolizumab necitumumab adalimumab reslizumab atezolizumab rituximab Colorectal cancer bevacizumab abatacept TRANSPLANTATION cetuximab tocilizumab Transplant rejection basiliximab panitumumab certolizumab pegol belatacept aflibercept golimumab Graft versus host disease inolimomab Bladder cancer atezolizumab Psoriatic arthritis etanercept Breast cancer trastuzumab adalimumab OPHTALMOLOGY bevacizumab infliximab Age related macular ranibizumab pertuzumab golimumab degeneration aflibercept trastuzumab entansine ustekinumab bevacizumab Gastric cancer trastuzumab certolizumab pegol Macular edema ranibizumab ramucirumab secukinumab aflibercept Head and neck cancer cetuximab Ankylosing spondylitis infliximab Myopic choroidal ranibizumab Ovarian cancer bevacizumab etanercept neovascularization aflibercept Fallopian tube cancer bevacizumab adalimumab Cervical cancer bevacizumab golimumab HAEMOSTASIS AND THROMBOSIS Kidney cancer bevacizumab certolizumab pegol nivolumab secukinumab Haemophilia A efmoroctocog α Melanoma ipilimumab Juvenile arthritis etanercept Haemophilia B eftrenonacog α nivolumab adalimumab Reversal of dabigatran idarucizumab Idiopathic thrombocytopenic pembrolizumab abatacept romiplostim Neuroblastoma dinutuximab tocilizumab purpura Malignant -
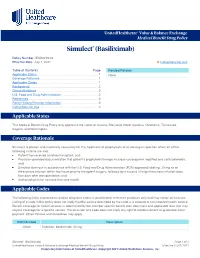
Simulect® (Basiliximab)
UnitedHealthcare® Value & Balance Exchange Medical Benefit Drug Policy Simulect® (Basiliximab) Policy Number: IEXD0219.02 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Policies Applicable States ........................................................................... 1 None Coverage Rationale ....................................................................... 1 Applicable Codes .......................................................................... 1 Background.................................................................................... 2 Clinical Evidence ........................................................................... 2 U.S. Food and Drug Administration ............................................. 2 References ..................................................................................... 2 Policy History/Revision Information ............................................. 2 Instructions for Use ....................................................................... 3 Applicable States This Medical Benefit Drug Policy only applies to the states of Arizona, Maryland, North Carolina, Oklahoma, Tennessee, Virginia, and Washington. Coverage Rationale Simulect is proven and medically necessary for the treatment of prophylaxis of acute organ rejection when all of the following criteria are met: Patient has received a kidney transplant; and Physician provided documentation that patient’s prophylaxis therapy includes cyclosporine modified and corticosteroids; and Simulect -

Sarcoidosis Manifesting During Treatment with Secukinumab for Psoriatic Arthritis Colm Kirby ,1 Darragh Herlihy,2 Lindsey Clarke,3 Ronan Mullan1
Case report BMJ Case Rep: first published as 10.1136/bcr-2020-240615 on 22 February 2021. Downloaded from Sarcoidosis manifesting during treatment with secukinumab for psoriatic arthritis Colm Kirby ,1 Darragh Herlihy,2 Lindsey Clarke,3 Ronan Mullan1 1Rheumatology, Tallaght SUMMARY University Hospital, Dublin, Sarcoidosis is a multisystem inflammatory disorder Ireland 2 of uncertain aetiology. There are numerous case Radiology, Beaumont Hospital, reports of sarcoidosis occurring during treatment with Dublin, Ireland biological immunotherapies. Here, we describe the case 3Pathology, Tallaght University Hospital, Dublin, Ireland of a 52- year- old woman with psoriatic arthritis who developed multisystem sarcoidosis while being treated Correspondence to with secukinumab (anti-interleukin- 17A) therapy which, Dr Colm Kirby; to our knowledge, is the first such case. We discuss colmkirby11@ gmail. com existing literature and hypothesise that IL-17 blockade may precipitate the development of granulomatous Accepted 8 February 2021 disease. BACKGROUND Figure 1 (A) Palmar longitudinal view of dactylitic Sarcoidosis is a multisystem disorder characterised finger showing tendon sheath effusion with power by the presence of non-caseat ing granulomata. Doppler signal. (B) longitudinal view of posterior tibialis While the disease is most commonly character- tendon showing tendon sheath effusion, tenosynovial ised by thoracic adenopathy, lung parenchyma, thickening and power Doppler signal. skin and articular disease, all organ systems may be affected. While the precise aetiology of sarcoid- sedimentation rate (ESR) of 16 mm/hour (1–15), osis is unclear, numerous case reports of sarcoid- normal C- reactive protein (CRP) and normal osis occurring during the treatment with biological rheumatoid factor, anti- cyclic citrullinated peptide immunotherapies indicate that immune dysregula- (anti- CCP) and anti- neutrophil cytoplasm antibody tion plays a key role. -

As Treatment for Refractory Acute Graft-Versus-Host Disease
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Biology of Blood and Marrow Transplantation 12:1135-1141 (2006) provided by Elsevier - Publisher Connector ᮊ 2006 American Society for Blood and Marrow Transplantation 1083-8791/06/1211-0001$32.00/0 doi:10.1016/j.bbmt.2006.06.010 Encouraging Results with Inolimomab (Anti-IL-2 Receptor) as Treatment for Refractory Acute Graft-versus-Host Disease Jose Luis Piñana, David Valcárcel, Rodrigo Martino, M. Estela Moreno, Anna Sureda, Javier Briones, Salut Brunet, Jorge Sierra Division of Clinical Hematology, Hospital de la Santa Creu i Sant Pau, Universitat Autónoma de Barcelona, Barcelona, Spain Correspondence and reprint requests: David Valcárcel, Division of clinical Hematology, Hospital de la Santa Creu i Sant Pau, St Antoni Ma Claret 167, Barcelona 08021, Spain (e-Mail: [email protected]). Received September 16, 2005; accepted June 21, 2006 ABSTRACT Enlimomab, an anti-interleukin-2 receptor (anti-IL-2R) monoclonal antibody, may be useful in the treatment of steroid-refractory acute graft-versus-host disease (aGVHD) by inhibiting 1 of its putative immunopatho- genic pathways. We retrospectively analyzed 40 consecutive patients who received enlimomab as salvage treatment for steroid refractory aGVHD at a single institution between June 1999 and December 2004. Enlimomab was given intravenously at a dose of 11 mg/d for 3 consecutive days, followed by 5.5 mg/d for 7 consecutive days and then 5.5 mg every other day for 5 doses. No infusion-related side effects were noted. Twenty-three patients (58%) responded, including 15 (38%) complete and 8 (20%) partial responses.