Article Urinary Angiotensinogen and Risk of Severe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplemental Figure 1. Vimentin
Double mutant specific genes Transcript gene_assignment Gene Symbol RefSeq FDR Fold- FDR Fold- FDR Fold- ID (single vs. Change (double Change (double Change wt) (single vs. wt) (double vs. single) (double vs. wt) vs. wt) vs. single) 10485013 BC085239 // 1110051M20Rik // RIKEN cDNA 1110051M20 gene // 2 E1 // 228356 /// NM 1110051M20Ri BC085239 0.164013 -1.38517 0.0345128 -2.24228 0.154535 -1.61877 k 10358717 NM_197990 // 1700025G04Rik // RIKEN cDNA 1700025G04 gene // 1 G2 // 69399 /// BC 1700025G04Rik NM_197990 0.142593 -1.37878 0.0212926 -3.13385 0.093068 -2.27291 10358713 NM_197990 // 1700025G04Rik // RIKEN cDNA 1700025G04 gene // 1 G2 // 69399 1700025G04Rik NM_197990 0.0655213 -1.71563 0.0222468 -2.32498 0.166843 -1.35517 10481312 NM_027283 // 1700026L06Rik // RIKEN cDNA 1700026L06 gene // 2 A3 // 69987 /// EN 1700026L06Rik NM_027283 0.0503754 -1.46385 0.0140999 -2.19537 0.0825609 -1.49972 10351465 BC150846 // 1700084C01Rik // RIKEN cDNA 1700084C01 gene // 1 H3 // 78465 /// NM_ 1700084C01Rik BC150846 0.107391 -1.5916 0.0385418 -2.05801 0.295457 -1.29305 10569654 AK007416 // 1810010D01Rik // RIKEN cDNA 1810010D01 gene // 7 F5 // 381935 /// XR 1810010D01Rik AK007416 0.145576 1.69432 0.0476957 2.51662 0.288571 1.48533 10508883 NM_001083916 // 1810019J16Rik // RIKEN cDNA 1810019J16 gene // 4 D2.3 // 69073 / 1810019J16Rik NM_001083916 0.0533206 1.57139 0.0145433 2.56417 0.0836674 1.63179 10585282 ENSMUST00000050829 // 2010007H06Rik // RIKEN cDNA 2010007H06 gene // --- // 6984 2010007H06Rik ENSMUST00000050829 0.129914 -1.71998 0.0434862 -2.51672 -

Appendix 2. Significantly Differentially Regulated Genes in Term Compared with Second Trimester Amniotic Fluid Supernatant
Appendix 2. Significantly Differentially Regulated Genes in Term Compared With Second Trimester Amniotic Fluid Supernatant Fold Change in term vs second trimester Amniotic Affymetrix Duplicate Fluid Probe ID probes Symbol Entrez Gene Name 1019.9 217059_at D MUC7 mucin 7, secreted 424.5 211735_x_at D SFTPC surfactant protein C 416.2 206835_at STATH statherin 363.4 214387_x_at D SFTPC surfactant protein C 295.5 205982_x_at D SFTPC surfactant protein C 288.7 1553454_at RPTN repetin solute carrier family 34 (sodium 251.3 204124_at SLC34A2 phosphate), member 2 238.9 206786_at HTN3 histatin 3 161.5 220191_at GKN1 gastrokine 1 152.7 223678_s_at D SFTPA2 surfactant protein A2 130.9 207430_s_at D MSMB microseminoprotein, beta- 99.0 214199_at SFTPD surfactant protein D major histocompatibility complex, class II, 96.5 210982_s_at D HLA-DRA DR alpha 96.5 221133_s_at D CLDN18 claudin 18 94.4 238222_at GKN2 gastrokine 2 93.7 1557961_s_at D LOC100127983 uncharacterized LOC100127983 93.1 229584_at LRRK2 leucine-rich repeat kinase 2 HOXD cluster antisense RNA 1 (non- 88.6 242042_s_at D HOXD-AS1 protein coding) 86.0 205569_at LAMP3 lysosomal-associated membrane protein 3 85.4 232698_at BPIFB2 BPI fold containing family B, member 2 84.4 205979_at SCGB2A1 secretoglobin, family 2A, member 1 84.3 230469_at RTKN2 rhotekin 2 82.2 204130_at HSD11B2 hydroxysteroid (11-beta) dehydrogenase 2 81.9 222242_s_at KLK5 kallikrein-related peptidase 5 77.0 237281_at AKAP14 A kinase (PRKA) anchor protein 14 76.7 1553602_at MUCL1 mucin-like 1 76.3 216359_at D MUC7 mucin 7, -

MALE Protein Name Accession Number Molecular Weight CP1 CP2 H1 H2 PDAC1 PDAC2 CP Mean H Mean PDAC Mean T-Test PDAC Vs. H T-Test
MALE t-test t-test Accession Molecular H PDAC PDAC vs. PDAC vs. Protein Name Number Weight CP1 CP2 H1 H2 PDAC1 PDAC2 CP Mean Mean Mean H CP PDAC/H PDAC/CP - 22 kDa protein IPI00219910 22 kDa 7 5 4 8 1 0 6 6 1 0.1126 0.0456 0.1 0.1 - Cold agglutinin FS-1 L-chain (Fragment) IPI00827773 12 kDa 32 39 34 26 53 57 36 30 55 0.0309 0.0388 1.8 1.5 - HRV Fab 027-VL (Fragment) IPI00827643 12 kDa 4 6 0 0 0 0 5 0 0 - 0.0574 - 0.0 - REV25-2 (Fragment) IPI00816794 15 kDa 8 12 5 7 8 9 10 6 8 0.2225 0.3844 1.3 0.8 A1BG Alpha-1B-glycoprotein precursor IPI00022895 54 kDa 115 109 106 112 111 100 112 109 105 0.6497 0.4138 1.0 0.9 A2M Alpha-2-macroglobulin precursor IPI00478003 163 kDa 62 63 86 72 14 18 63 79 16 0.0120 0.0019 0.2 0.3 ABCB1 Multidrug resistance protein 1 IPI00027481 141 kDa 41 46 23 26 52 64 43 25 58 0.0355 0.1660 2.4 1.3 ABHD14B Isoform 1 of Abhydrolase domain-containing proteinIPI00063827 14B 22 kDa 19 15 19 17 15 9 17 18 12 0.2502 0.3306 0.7 0.7 ABP1 Isoform 1 of Amiloride-sensitive amine oxidase [copper-containing]IPI00020982 precursor85 kDa 1 5 8 8 0 0 3 8 0 0.0001 0.2445 0.0 0.0 ACAN aggrecan isoform 2 precursor IPI00027377 250 kDa 38 30 17 28 34 24 34 22 29 0.4877 0.5109 1.3 0.8 ACE Isoform Somatic-1 of Angiotensin-converting enzyme, somaticIPI00437751 isoform precursor150 kDa 48 34 67 56 28 38 41 61 33 0.0600 0.4301 0.5 0.8 ACE2 Isoform 1 of Angiotensin-converting enzyme 2 precursorIPI00465187 92 kDa 11 16 20 30 4 5 13 25 5 0.0557 0.0847 0.2 0.4 ACO1 Cytoplasmic aconitate hydratase IPI00008485 98 kDa 2 2 0 0 0 0 2 0 0 - 0.0081 - 0.0 -

Urinary Proteomics for the Early Diagnosis of Diabetic Nephropathy in Taiwanese Patients Authors
Urinary Proteomics for the Early Diagnosis of Diabetic Nephropathy in Taiwanese Patients Authors: Wen-Ling Liao1,2, Chiz-Tzung Chang3,4, Ching-Chu Chen5,6, Wen-Jane Lee7,8, Shih-Yi Lin3,4, Hsin-Yi Liao9, Chia-Ming Wu10, Ya-Wen Chang10, Chao-Jung Chen1,9,+,*, Fuu-Jen Tsai6,10,11,+,* 1 Graduate Institute of Integrated Medicine, China Medical University, Taichung, 404, Taiwan 2 Center for Personalized Medicine, China Medical University Hospital, Taichung, 404, Taiwan 3 Division of Nephrology and Kidney Institute, Department of Internal Medicine, China Medical University Hospital, Taichung, 404, Taiwan 4 Institute of Clinical Medical Science, China Medical University College of Medicine, Taichung, 404, Taiwan 5 Division of Endocrinology and Metabolism, Department of Medicine, China Medical University Hospital, Taichung, 404, Taiwan 6 School of Chinese Medicine, China Medical University, Taichung, 404, Taiwan 7 Department of Medical Research, Taichung Veterans General Hospital, Taichung, 404, Taiwan 8 Department of Social Work, Tunghai University, Taichung, 404, Taiwan 9 Proteomics Core Laboratory, Department of Medical Research, China Medical University Hospital, Taichung, 404, Taiwan 10 Human Genetic Center, Department of Medical Research, China Medical University Hospital, China Medical University, Taichung, 404, Taiwan 11 Department of Health and Nutrition Biotechnology, Asia University, Taichung, 404, Taiwan + Fuu-Jen Tsai and Chao-Jung Chen contributed equally to this work. Correspondence: Fuu-Jen Tsai, MD, PhD and Chao-Jung Chen, PhD FJ Tsai: Genetic Center, China Medical University Hospital, No.2 Yuh-Der Road, 404 Taichung, Taiwan; Telephone: 886-4-22062121 Ext. 2041; Fax: 886-4-22033295; E-mail: [email protected] CJ Chen: Graduate Institute of Integrated Medicine, China Medical University, No.91, Hsueh-Shih Road, 404, Taichung, Taiwan; Telephone: 886-4-22053366 Ext. -

Supplementary Table 1
Supplementary Table 1. 492 genes are unique to 0 h post-heat timepoint. The name, p-value, fold change, location and family of each gene are indicated. Genes were filtered for an absolute value log2 ration 1.5 and a significance value of p ≤ 0.05. Symbol p-value Log Gene Name Location Family Ratio ABCA13 1.87E-02 3.292 ATP-binding cassette, sub-family unknown transporter A (ABC1), member 13 ABCB1 1.93E-02 −1.819 ATP-binding cassette, sub-family Plasma transporter B (MDR/TAP), member 1 Membrane ABCC3 2.83E-02 2.016 ATP-binding cassette, sub-family Plasma transporter C (CFTR/MRP), member 3 Membrane ABHD6 7.79E-03 −2.717 abhydrolase domain containing 6 Cytoplasm enzyme ACAT1 4.10E-02 3.009 acetyl-CoA acetyltransferase 1 Cytoplasm enzyme ACBD4 2.66E-03 1.722 acyl-CoA binding domain unknown other containing 4 ACSL5 1.86E-02 −2.876 acyl-CoA synthetase long-chain Cytoplasm enzyme family member 5 ADAM23 3.33E-02 −3.008 ADAM metallopeptidase domain Plasma peptidase 23 Membrane ADAM29 5.58E-03 3.463 ADAM metallopeptidase domain Plasma peptidase 29 Membrane ADAMTS17 2.67E-04 3.051 ADAM metallopeptidase with Extracellular other thrombospondin type 1 motif, 17 Space ADCYAP1R1 1.20E-02 1.848 adenylate cyclase activating Plasma G-protein polypeptide 1 (pituitary) receptor Membrane coupled type I receptor ADH6 (includes 4.02E-02 −1.845 alcohol dehydrogenase 6 (class Cytoplasm enzyme EG:130) V) AHSA2 1.54E-04 −1.6 AHA1, activator of heat shock unknown other 90kDa protein ATPase homolog 2 (yeast) AK5 3.32E-02 1.658 adenylate kinase 5 Cytoplasm kinase AK7 -

Composition of the Peptide Fraction in Human Blood Plasma: Database of Circulating Human Peptides
Journal of Chromatography B, 726 (1999) 25±35 Composition of the peptide fraction in human blood plasma: database of circulating human peptides Rudolf Richtera,* , Peter Schulz-Knappe b , Michael Schrader b , Ludger StandkerÈ a , Michael JurgensÈ ba , Harald Tammen , Wolf-Georg Forssmann a aLower Saxony Institute for Peptide Research, Feodor-Lynen-Strasse 31, D-30625 Hannover, Germany bBioVisioN, Feodor-Lynen-Strasse 5, D-30625 Hannover, Germany Received 7 September 1998; received in revised form 28 December 1998; accepted 28 December 1998 Abstract A database was established from human hemo®ltrate (HF) that consisted of a mass database and a sequence database, with the aim of analyzing the composition of the peptide fraction in human blood. To establish a mass database, all 480 fractions of a peptide bank generated from HF were analyzed by MALDI-TOF mass spectrometry. Using this method, over 20 000 molecular masses representing native, circulating peptides were detected. Estimation of repeatedly detected masses suggests that approximately 5000 different peptides were recorded. More than 95% of the detected masses are smaller than 15 000, indicating that HF predominantly contains peptides. The sequence database contains over 340 entries from 75 different protein and peptide precursors. 55% of the entries are fragments from plasma proteins (®brinogen A 13%, albumin 10%, b2-microglobulin 8.5%, cystatin C 7%, and ®brinogen B 6%). Seven percent of the entries represent peptide hormones, growth factors and cytokines. Thirty-three percent belong to protein families such as complement factors, enzymes, enzyme inhibitors and transport proteins. Five percent represent novel peptides of which some show homology to known peptide and protein families. -

Diagnostic Urinary Proteome Profile for Immunoglobulin a Nephropathy
Archive of SID KIDNEY DISEASES Diagnostic Urinary Proteome Profile for Immunoglobulin A Nephropathy Shiva Samavat,1,2 Shiva Kalantari,3 Mohsen Nafar,3 Dorothea Rutishauser,4,5 Mostafa Rezaei-Tavirani,6,7 Mahmud Parvin,8 Roman A Zubarev4,5 1Department of Nephrology, Introduction. Immunoglobulin A (IgA) nephropathy, the most Shahid Labbafinejad Medical common type of glomerulonephritis, is only diagnosed by invasive Center, Shahid Beheshti kidney biopsy. Urine proteome panel might help in noninvasive University of Medical Sciences, Tehran, Iran diagnosis and also better understanding of pathogenesis of IgA 2Urology and Nephrology nephropathy. Research Center, Shahid Materials and Methods. Second mid-stream urine samples of 13 Beheshti University of Medical patients with biopsy-proven IgA nephropathy and 8 healthy controls Sciences, Tehran, Iran were investigated by means of nanoscale liquid chromatography 3Chronic Kidney Diseases Research Center, Shahid tandem mass spectrometry. Multivariate analysis of quantified Beheshti University of Medical label-free proteins was performed by the principal component Sciences, Tehran, Iran analysis and partial least squares models. 4Department of Medical Results. A total number of 493 unique proteins were quantified Biochemistry and Biophysics, by nanoscale liquid chromatography tandem mass spectrometry, Karolinska Institute, Stockholm, of which 46 proteins were considered as putative biomarkers of Sweden 5SciLifeLab, Stockholm, Sweden IgA nephropathy, after multivariate analysis and additional filter 6Department of Basic Sciences, criterion and comparing the patients and the controls. Some of the Faculty of Paramedical Sciences, significant differentially expressed proteins were CD44, glycoprotein Shahid Beheshti University of 2, vasorin, epidermal growth factor, CLM9, protocadherin, Medical Sciences, Tehran, Iran utreoglobin, dipeptidyl peptidase IV, NHL repeat-containing protein 7Proteomics Research Center, Faculty of Paramedical Sciences, 3, and SLAM family member 5. -

Identification of Genomic Targets of Krüppel-Like Factor 9 in Mouse Hippocampal
Identification of Genomic Targets of Krüppel-like Factor 9 in Mouse Hippocampal Neurons: Evidence for a role in modulating peripheral circadian clocks by Joseph R. Knoedler A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Neuroscience) in the University of Michigan 2016 Doctoral Committee: Professor Robert J. Denver, Chair Professor Daniel Goldman Professor Diane Robins Professor Audrey Seasholtz Associate Professor Bing Ye ©Joseph R. Knoedler All Rights Reserved 2016 To my parents, who never once questioned my decision to become the other kind of doctor, And to Lucy, who has pushed me to be a better person from day one. ii Acknowledgements I have a huge number of people to thank for having made it to this point, so in no particular order: -I would like to thank my adviser, Dr. Robert J. Denver, for his guidance, encouragement, and patience over the last seven years; his mentorship has been indispensable for my growth as a scientist -I would also like to thank my committee members, Drs. Audrey Seasholtz, Dan Goldman, Diane Robins and Bing Ye, for their constructive feedback and their willingness to meet in a frequently cold, windowless room across campus from where they work -I am hugely indebted to Pia Bagamasbad and Yasuhiro Kyono for teaching me almost everything I know about molecular biology and bioinformatics, and to Arasakumar Subramani for his tireless work during the home stretch to my dissertation -I am grateful for the Neuroscience Program leadership and staff, in particular -

Increased Alveolar Soluble Annexin V Promotes Lung Inflammation and Fibrosis
Increased alveolar soluble Annexin V promotes lung inflammation and fibrosis Supplemental data - Materials and methods Human BALF. Bronchoalveolar Lavage (BALF) was performed at the National Institute of Respiratory Diseases (INER), Mexico City, Mexico,as approved by the Ethics Committee at INER. is performed through flexible fiberoptic bronchoscopy under local anesthesia. Briefly, 200 ml of normal saline is instilled in 50-ml aliquots, with an average recovery of 60%–70%. The cells are pelleted from the BALF, and the cell-free supernatant is frozen at -80oC. The control group for Figure 1 included 3 healthy volunteers, and 2 individuals without HRCT-scan evidence of lung disease who required a bronchoscopy for the diagnosis of unexplained cough. In all cases bronchoscopy did not display any abnormality. Removal of Annexin V from BALF by immunoprecipitation. BALF samples with known elevated Annexin V levels were pre-cleared by mixing with 1g rabbit IgG and 20l of protein A/G agarose at 4o for 30 mins, followed by centrifuging at 1000g for 30s at 4oC. The supernatants were removed to clean tubes and incubated with mixing for 1h with 4g rabbit anti-Annexin V antibody or 4g rabbit IgG, then. 20l of protein A/G agarose was added and the tubes were incubated with mixing for 1h at 40C. The tubes were centrifuged for 30s at 1000g, and the supernatant carefully removed. PBS washes of the immunoprecipitate were pooled with the supernatant. Successful reduction of Annexin V levels was confirmed by ELISA. Intra-tracheal instillation of Annexin V solution. 8 week C57 female black mice were anaesthetized with isofluorane and suspended at a 45-60°C angle on an intubation platform. -

The Detection of Circulating Breast Cancer Cells in Blood a M Gilbey, D Burnett, R E Coleman, I Holen
903 REVIEW J Clin Pathol: first published as 10.1136/jcp.2003.013755 on 27 August 2004. Downloaded from The detection of circulating breast cancer cells in blood A M Gilbey, D Burnett, R E Coleman, I Holen ............................................................................................................................... J Clin Pathol 2004;57:903–911. doi: 10.1136/jcp.2003.013755 At present, sampling of the lymph nodes or bone marrow demand for supportive, palliative, and medical services. for the detection of regions of metastatic disease in patients with breast cancer can only be undertaken at the time of BREAST CANCER METASTASES initial diagnosis and surgery. However, the sampling of The metastatic process these tissues and the methods used are inaccurate, time Metastasis is a cascade of linked sequential steps involving multiple host–tumour interactions.4 consuming, and cannot be used for easy routine screening Cancer cells possessing multiple genetic abnorm- to determine disease recurrence and response to treatment. alities grow unregulated and eventually lose the Because of the problems encountered with current methods ability to adhere to one another.4 Thus, tumour cells detach from the primary tumour, migrate and tissues sampled at the time of breast cancer diagnosis, through the basement membrane and extracel- this review discusses the urgent requirement for and lular matrix, intravasate, and travel in the potential development of a quick, simple, and accurate lymphatic and/or blood systems to a new site, before attachment, extravasation, and the devel- diagnostic test utilising the haematogenous system, a opment of a new focus and neovascularistion.5 source of circulating tumour cells in patients with breast When cancer cells enter the lymphatic system, cancer, and highly sensitive molecular biological they travel to the lymph nodes (LN)4—in the case of breast cancer, to the sentinel nodes in the techniques, such as reverse transcription polymerase chain axilla and intercostal spaces—before entering the reaction. -

Neutrophil Recruitment and Phagocytosis of Boar Spermatozoa
REPRODUCTIONRESEARCH Effect of low-dose mifepristone administration on day 2 after ovulation on transcript profiles in implantation-stage endometrium of rhesus monkeys D Ghosh, A M Sharkey1, D S Charnock-Jones2, S K Smith3 and Jayasree Sengupta Department of Physiology, All India Institute of Medical Sciences, New Delhi 110029, India, Departments of 1Pathology and 2Obstetrics and Gynaecology, University of Cambridge, Cambridge CB2 2SW, UK and 3Faculty of Medicine, Imperial College London, London SW7 2AZ, UK Correspondence should be addressed to D Ghosh; Email: [email protected] Abstract Progesterone is essential for endometrial receptivity in primates. In studies previously performed using global gene profiling based on microarray technology, attempts have been made to identify changes in gene expression between early luteal-phase and mid-luteal-phase endometria. However, the issue of the putative impact of preimplantation embryo-derived signal in the process of endometrial receptivity was missing in the previous studies. In the present study, an attempt has been made to delineate the transcripts profile in implantation-stage endometrium under combinatorial regulation of progesterone and embryo-derived signal in the rhesus monkey. To this effect, we have compared transcript profiles for 409 known genes between control receptive stage (nZ13), and mifepristone-induced desynchronized and non-receptive stage (nZ12) monkey endometrial samples collected on days 4 (nZ12) and 6 (nZ13) after ovulation from mated, potential conception cycles, -
Downloaded from the Mouse Lysosome Gene Database, Mlgdb
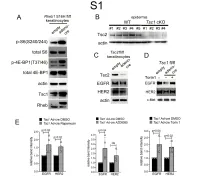
1 Supplemental Figure Legends 2 3 Supplemental Figure S1: Epidermal-specific mTORC1 gain-of-function models show 4 increased mTORC1 activation and down-regulate EGFR and HER2 protein expression in a 5 mTORC1-sensitive manner. (A) Immunoblotting of Rheb1 S16H flox/flox keratinocyte cultures 6 infected with empty or adenoviral cre recombinase for markers of mTORC1 (p-S6, p-4E-BP1) 7 activity. (B) Tsc1 cKO epidermal lysates also show decreased expression of TSC2 by 8 immunoblotting of the same experiment as in Figure 2A. (C) Immunoblotting of Tsc2 flox/flox 9 keratinocyte cultures infected with empty or adenoviral cre recombinase showing decreased EGFR 10 and HER2 protein expression. (D) Expression of EGFR and HER2 was decreased in Tsc1 cre 11 keratinocytes compared to empty controls, and up-regulated in response to Torin1 (1µM, 24 hrs), 12 by immunoblot analyses. Immunoblots are contemporaneous and parallel from the same biological 13 replicate and represent the same experiment as depicted in Figure 7B. (E) Densitometry 14 quantification of representative immunoblot experiments shown in Figures 2E and S1D (r≥3; error 15 bars represent STDEV; p-values by Student’s T-test). 16 17 18 19 20 21 22 23 Supplemental Figure S2: EGFR and HER2 transcription are unchanged with epidermal/ 24 keratinocyte Tsc1 or Rptor loss. Egfr and Her2 mRNA levels in (A) Tsc1 cKO epidermal lysates, 25 (B) Tsc1 cKO keratinocyte lysates and(C) Tsc1 cre keratinocyte lysates are minimally altered 26 compared to their respective controls. (r≥3; error bars represent STDEV; p-values by Student’s T- 27 test).