Community Service Usage Pack for Practices
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Draft Recommendations on the Future Electoral Arrangements for Newark & Sherwood in Nottinghamshire
Draft recommendations on the future electoral arrangements for Newark & Sherwood in Nottinghamshire Further electoral review December 2005 Translations and other formats For information on obtaining this publication in another language or in a large-print or Braille version please contact The Boundary Committee for England: Tel: 020 7271 0500 Email: [email protected] The mapping in this report is reproduced from OS mapping by The Electoral Commission with the permission of the Controller of Her Majesty’s Stationery Office, © Crown Copyright. Unauthorised reproduction infringes Crown Copyright and may lead to prosecution or civil proceedings. Licence Number: GD 03114G 2 Contents Page What is The Boundary Committee for England? 5 Executive summary 7 1 Introduction 15 2 Current electoral arrangements 19 3 Submissions received 23 4 Analysis and draft recommendations 25 Electorate figures 26 Council size 26 Electoral equality 27 General analysis 28 Warding arrangements 28 a Clipstone, Edwinstowe and Ollerton wards 29 b Bilsthorpe, Blidworth, Farnsfield and Rainworth wards 30 c Boughton, Caunton and Sutton-on-Trent wards 32 d Collingham & Meering, Muskham and Winthorpe wards 32 e Newark-on-Trent (five wards) 33 f Southwell town (three wards) 35 g Balderton North, Balderton West and Farndon wards 36 h Lowdham and Trent wards 38 Conclusions 39 Parish electoral arrangements 39 5 What happens next? 43 6 Mapping 45 Appendices A Glossary and abbreviations 47 B Code of practice on written consultation 51 3 4 What is The Boundary Committee for England? The Boundary Committee for England is a committee of The Electoral Commission, an independent body set up by Parliament under the Political Parties, Elections and Referendums Act 2000. -

Charged for Violent Offences Between 21 281113.Pdf
Alliance against Violence 28 November 2013 Today is the final day of our second week of action relating to the Alliance Against Violence. During this week Chief Inspector Ted Antill, the force lead for hate crime, has spoken out about it, Mickey Donald, a victim of disability hate crime has shared his story, and we have also reported on new projects funded by the Police and Crime Commissioner. Information on support for victims has also been made available. While the focus of the week has been hate crime we are continuing to drive home the message that we will not accept any form of violent crime. Between Thursday 21 November 2013 and Thursday 28 November 2013 89 people were charged in relation to violent offences. The below is a full list of those charged: First name Surname Age Address Offence Status Paul WRIGHT 32 CATKIN DRIVE Assault by Charged and Anthony GILTBROOK beating Bailed To NOTTINGHAM Court Calvin John HENRY 47 HAYDN ROAD Assault by Charged and NOTTINGHAM beating Bailed To Court Carl GALLON 27 DENNIS AVENUE, Assault a Charged and Andrew BEESTON person Bailed To David thereby Court occasioning them actual bodily harm Sam SCOTT 26 ROLLESTON DRIVE Assault by Charged and ARNOLD beating Bailed To Court Kismet ALTAF 55 SKIPTON CIRCUS Assault by Charged and NOTTINGHAM beating Bailed To Court Anthony SEDDON 45 CARLTON HILL, Assault by Charged and John CARLTON beating Bailed To Court Nevin TAYLOR 29 RADFORD ROAD Assault by Charged and NOTTINGHAM beating Bailed To Court Richard WILDING 31 COLSTON ROAD Common Charged and Michael NOTTINGHAM -

The Newark & Sherwood (Electoral Changes) Order 2014
Draft Order laid before Parliament under section 59(9) of the Local Democracy, Economic Development and Construction Act 2009; draft to lie for forty days pursuant to section 6(1) of the Statutory Instruments Act 1946, during which period either House of Parliament may resolve that the Order be not made. DRAFT STATUTORY INSTRUMENTS 2014 No. LOCAL GOVERNMENT, ENGLAND The Newark & Sherwood (Electoral Changes) Order 2014 Made - - - - *** Coming into force in accordance with article 1(2) Under section 58(4) of the Local Democracy, Economic Development and Construction Act 2009( a) (“the Act”) the Local Government Boundary Commission for England( b) (“the Commission”) published a report dated March 2014 stating its recommendations for changes to the electoral arrangements for the district of Newark & Sherwood. The Commission has decided to give effect to the recommendations. A draft of the instrument has been laid before Parliament and a period of forty days has expired and neither House has resolved that the instrument be not made. The Commission makes the following Order in exercise of the power conferred by section 59(1) of the Act: Citation and commencement 1. —(1) This Order may be cited as the Newark & Sherwood (Electoral Changes) Order 2014. (2) This Order comes into force— (a) for the purpose of proceedings preliminary or relating to the election of councillors, on 15th October 2014; (b) for all other purposes, on the ordinary day of election of councillors in 2015. Interpretation 2. In this Order— “map” means the map marked “Map referred to in the Newark & Sherwood (Electoral Changes) Order 2014”, prints of which are available for inspection at the principal office of the Local Government Boundary Commission for England; (a) 2009 c.20. -

Michael John Wilson
CHURCH OF ENGLAND GENERAL SYNOD ELECTION ADDRESS FOR Michael John Wilson I am standing for election to the House of Laity for the General Synod of the Church of England, to represent the Southwell and Nottingham Diocese and ask you to cast your vote in my favour. I am a member of the Diocesan Synod at which I have enjoyed contributing to the debates and in particular listening to other members. I was elected by the synod to be a member of the Diocesan Board of Education at which I have witnessed a number of changes to church school provision in response to the changes introduced by the government. I believe my previous experience in education has help me make worthwhile and supportive contributions. I am the lay-chair of the Newark and Southwell Deanery which so far has been challenging, interesting but also stimulating. Trying to work with so many parishes within the deanery, especially with over half being in vacancy, has been a big challenge but I have learnt so much about the wider Church of England as a result. This has been the interesting part, seeing how different and varied parishes are but at the same time enjoying a common fellowship and faith. The stimulation is to go forward to use what gifts, experiences and skills I have at another level within the churches structure, hence my candidature. I worship at St Giles, Balderton where my main role is of treasurer. I have served as the editor of the parish magazine and choir master, although I continue to sing in the stalls and help with the music as best I can. -

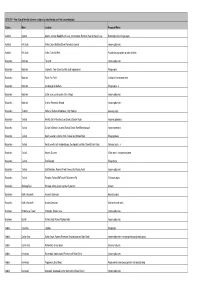
Nottinghamshire County Council Day Services Day Service Client Group
Nottinghamshire County Council day services Day Service Client Group Address Telephone Email Address Number Ashfield Day Learning disabilities, Sheepwash Lane 01623 550376 [email protected] Service physical disabilities, Sutton in Ashfield older people, mental NG17 5GG health Bassetlaw Day Learning disabilities, Albion Close 01909 474144 [email protected] Service (Main Site) physical disabilities, Worksop older people S80 1RA Bassetlaw Day Learning disabilities, Watson Road 01909 474144 [email protected] Service (Library) physical disabilities, Worksop mental health S80 2BL Broxtowe Day Learning disabilities, Sunnyside Road 0115 [email protected] Service (Main Site) physical disabilities, Beeston 9674805 older people, mental NG9 4FR health Gedling Day Learning disabilities, Howbeck Road 0115 [email protected] Service (Main Site) physical disabilities, Arnold 9674805 older people, mental NG5 8AA health Gedling Day Learning disabilities, Ley Street 0115 [email protected] Service physical disabilities Netherfield 9613639 (Netherfield) NG4 2PH Page 1 of 2 Day Service Client Group Address Telephone Email Address Number Mansfield Day Learning disabilities, Southwell Road West 01623 795991 [email protected] Service physical disabilities, Rainworth older people, mental Mansfield health NG21 0HJ Newark and Learning disabilities, Main Road 01909 474144 [email protected] Sherwood Day older people Boughton Service (Main Site) Newark NG22 9TD Newark and Learning disabilities, London Road 01909 474144 [email protected] Sherwood Day physical disabilities, New Balderton Service (Newark) older people Newark NG24 3AL Rushcliffe Day Older people Moor Lane 01949 836652 [email protected] Service (Bingham) Bingham NG13 8AS Page 2 of 2 . -

Annual Report2016/17
P s ri e m ic v ar r y e In y S teg nit rated Commu Primary Integrated Community Services Limited Registered Office: Unit H4, Ash Tree Court, Nottingham Business Park, Nottingham NG8 6PY P s ri e m ic v ar r Tel: 03000 830000 y e In y S [email protected] teg nit rated mmu www.picsnhs.org.uk Co Annual Report 2016/17 Excellence in patient and primary care Registered in England & Wales Company Registration Number 8763136 Primary Integrated Community Services Foreword Primary care Integrated Community Services are proud to present a copy of the second Annual Report The report highlights our achievements and progress over the last year, including a summary of our accounts and current financial position. ‘We Care’ “We Care” about our patients, carers and families, our partners and all the people we work with underpinned by our core values and our “can do” approach. We regularly review our values and ensure these are integral at all levels of the organisation. Our Values Our values are integral at every level of the organisation and were created by “us” the people that work here. n Family and patient need is central to our decision making n We have a “can do” approach that is responsive, creative and innovative n We are non-judgemental, open and transparent with a no blame culture n We are inclusive and collaborative inside and outside the organisation n We are professional and passionate about our care for patients and one another n We put safety first in everything we do n We protect and support General Practice and our clinicians n Our care is evidence based, safe and effective 2 3 Message from Message from Alison Rounce Managing Director Dr Kelvin Lim Medical Director I am very proud of the progress PICS has working with some groups of practices to Our organisation has grown considerably over This good work was led by Dr Kerri Sallis. -

Vebraalto.Com
TANGRA, 64 LONDON ROAD New Balderton, Newark, Nottinghamshire, NG24 3AH TANGRA, 64 LONDON ROAD New Balderton, Newark, Nottinghamshire, NG24 3AH A timeless property set in the popular, sought after location of Newark, featuring a high quality interior with bespoke cabinetry by Tristan Goff handcrafted furniture, beautiful flooring and elegant design throughout. The double fronted period property has been renovated to provide practical whilst luxurious living space, three double bedrooms and a second floor entertainment room/ fourth bedroom. There is ample parking to the side and rear, a tandem garage and manicured gardens. Ground Floor Approached through a pedestrian gate through the wrought iron fence, the stone path, flanked by symmetrical raised brick based shrubbery beds, leads to the front door, which opens into the welcoming entrance hall. From the entrance hall, the first door on the right leads into the beautiful kitchen which benefits from a range of luxury, bespoke modern shaker style ground and wall units. The feature marble countertops blend seamlessly into a splash back and the atmospheric hidden lighting used throughout the room highlights the beautiful cabinetry and crown molding. The two built in ovens are housed below the electric hob. A large split level island with sink and lower level breakfast seating provides a great family and entertaining space. The kitchen flows directly into the utility area towards the rear of the property, which can also be accessed by the hallway. The utility benefits from further bespoke cabinetry and beautiful countertops, with a sink and large area for a free standing American style fridge/freezer. A door to the rear of the utility enters into the boot room with further bespoke storage and access to the rear garden. -

Retford, Newark, Nottingham & Bingham
Archdeaconry Wills for the Deaneries of - Retford, Newark, Nottingham & Bingham Page 2 James BEALBY of North Collingham, Wheelwright - proved 10th Aug 1846. (died 14th April 1846). Page 5, 6 & 7 Mary TODER, of Newark upon Trent, widow- Admon - 26th Sept 1838 mentions she was a legatee in the Will of Thomas DERRY, proved 19th Jan 1822. + Admon Bond 8th Dec 1846. Page 8 Alexander Newman GIRTON of Newark upon Trent, Yeoman - proved 22nd June 1846 (died 26th Aug 1845) Page 12 William GRASBY of Moorhouse in the parish of Laxton - proved 10th Aug 1848. (died 20th Feb 1846). Page 14 Samuel HALL of South Collingham, Blacksmith - proved 10th Aug 1846. ( died 12th Nov 1845). Page 18 Richard HARRISON of Balderton, Farmer. - proved, 16 Oct 1846. (died 31st Dec 1845). Page 23 Thomas HOPKINSON of Girton, Farmer - proved, 10th Aug 1846. (died 28th Sept 1845). Page 26 Joseph TAYLOR, snr of Weston, Publican - proved,10th Aug 1846. (died 5th Jan 1846). Page 29 Joseph BOWMAN of Eakring, Yeoman - proved, 28 Aug 1847. ( died 27th Sept 1846). Page 31 Richard CROSBY of Coddington, Yeoman - Admon 19th March 1847. (died 25th Sept 1846). Page 36 William ELSON of Newark, Lock Keeper - proved 19th March 1847. (died 27th Aug 1846). Page 40 Elizabeth FEATHERSTONE of Barnby in the Willows, widow, - Admon 28th Aug 1847. (died 30th Nov 1846). Page 42 John LONG of Elston Lodge, Farmer. - proved 16th July 1847. (died 11th April 1847). Page 44 John MANTLE of Newark - proved 28th Aug 1847. (died 9th May 1847) Page 46 John OLDHAM, of Balderton, Surveyor. -
05 Local Improvement Scheme App 1A-Local Identity Schemes
2011/2012 - Year 8 Local Identity Schemes ( subject to detail design and final cost estimation) District Ward Location Proposed Works Ashfield Selston Selston, Alfreton Road/Church Lane, Commonside, Portland Road & Stoney Lane Restoration of four finger posts Ashfield KIA South Kirkby Cross, Mayfield Street Recreation Ground Improve play area Ashfield KIA South Kirkby, Titchfield Park Provide play equipment for older children Bassetlaw Misterton Torworth Improve play area Bassetlaw Misterton Clayworth, Town Street (north & south approaches) Village signs Bassetlaw Misterton Ranby Fun Field Creation of recreational area Bassetlaw Misterton Clarborough & Welham Village signs - 2 Bassetlaw Misterton Sutton cum Lound (centre of the Village) Improve play area Bassetlaw Misterton Everton Recreation Ground Improve play area Bassetlaw Tuxford Holbeck, Welbeck Woodhouse, High Holbeck Gateway signs Bassetlaw Tuxford North & South Wheatley, Low Street & Sturton Road Improved gateways Bassetlaw Tuxford Sturton le Steeple, Leverton Road & Station Road/Gainsborough Improve gateways Bassetlaw Tuxford South Leverton, entrance from Treswell and Station Road Village gateway Bassetlaw Tuxford North Leverton with Habblesthorpe, Southgate Lane/Main Street/Sturton Road Gateway signs - 3 Bassetlaw Tuxford Newark Sustrans 1 Seat and 1 interpretation panel Bassetlaw Tuxford East Drayton Village Signs Bassetlaw Tuxford East Markham, Rayner's Field (Community Playing Field) Improve play area Bassetlaw Tuxford Rampton, Retford Rd/Trawell Rd/Laneham Rd 3 Gateway signs -

Nottingham and Nottinghamshire Pcns: Information Pack
Nottingham and Nottinghamshire PCNs: information pack Contents Introduction ....................................................................................................................................................................... 2 Mid Nottinghamshire ........................................................................................................................................................ 3 Overview ......................................................................................................................................................................... 3 Mansfield and Ashfield CCG ........................................................................................................................................... 4 CCG overview ............................................................................................................................................................ 4 Ashfield North PCN .................................................................................................................................................... 4 Ashfield South PCN .................................................................................................................................................... 5 Mansfield North PCN .................................................................................................................................................. 5 Mansfield South PCN ................................................................................................................................................ -

Lindley of Nottinghamshire Joseph WATERALL
Lindley of Nottinghamshire Joseph WATERALL Benjamin HAMILTON Isabella WREE Joseph PURVIS Mary SMITH John RALSTON Mathew KENYON-STOW Susan ... William Henry PEAT Fanny RAXBY Hannah RAXBY Mary WATERALL Edward LINDLEY b ca. 1798 Hexham b ca. 1800 Hexham b ca. 1800 Warden, b ca. 1817 Roxburghshire, contractor b ca. 1806 Scotland b ca. 1813 London b ca. 1816 Kentish Town, MDX b ca. 1817 South Shields, b ca. 1805 Monkwearmouth, b ca. 1801 Selston, Notts. b ca. 1796 1851: Shoemaker & Grocer, 1851: Bread Baker Northumberland Scotland 1881: Income from Interests 1861: Produce Broker of 4 Kidbrooke Durham Durham bp 13 Dec 1801 Selston 1841, 1851 licenced victualler Gilligate, Hexham d 1875 m 31 Jan 1836 Ancrum 1841: Boundaries, Jedburgh, Sneyd Park Lodge, Terrace, Kidbrooke, Kent 1861, 1871: visiting brother m 18 Mar 1827 Greasley Yew Tree Inn, Derby/Mansfield Rd. 1861: Grocer & Shoemaker, Roxburghshire, Scotland Roxburghshire, Scotland Westbury on Trym 1871: Colonial Produce Broker, in law William PEAT 1851: grocer of Beggarlee, Old Brinsley, Greasley Galligate, Hexham 1841: not found 1861: Retired Grocer, Law Gloucestershire Heath House, Greenwich Greasley 1871: Retired publican, widower, 1871: Retired Tradesman, 1851: Horse Trainer of Leases, Hexham 1891: Produce Broker Agent of d 1866iii Basford 7b 50, Mansfield Rd, Brinsley, Greasley 10, Gillegate, Hexham Haugh Lane, Hexham, South Hayes, South side age 64 d 1876 Northumberland Wimbledon Common 1859 dau m: merchant 16 servants d reg 1852 Hexham Visitor: Maitland F. KENYON-STOW Edward CORBETT John HAMILTON Sarah HAMILTON Joseph HAMILTON Barbara HAMILTON John PURVIS Mary CORBETT George PURVIS Hannah HAMILTON Elizabeth Marion PEAT Sir Robert PURVIS Isabella PURVIS Agnes PURVIS John Alexander RALSTON Martha PURVIS Selina M KENYON-STOW Maitland F KENYON-STOW Frederick Melkington KENYON-STOW Alice Millicent PEAT Arthur R PEAT James Ernest PEAT Alfred Edward PEAT Eliza KNOWLES William LINDLEY John BENTLEY Eliza .. -
Vasectomy Leaflet
NOTTINGHAMSHIRE COMMUNITY VASECT OMY SERVICE FREE NHS SERVICE To make an appointment CONTACT US TELEPHONE 01623 624137 FAX 016 2 3 422137 Email: [email protected] [email protected] www.nottinghamroad.co.uk Nottinghamshire Community Vasectomy Service Is a FREE NHS service provided for patients registered with an NHS general Practice within the Nottinghamshire area. How do I get referred? Men who wish to have a vasectomy can be referred by their Family Doctor or if they wish may REFER THEMSELVES directly to the Nottinghamshire Community Vasectomy Service using the contact details on the front of this leaflet. Who performs the operation? The Vasectomy Service is provided by 6 local medical practitioners working within your community who are specially trained, accredited and experienced to provide the operation close to the patients’ own home without having to go to hospital. The 6 Vasectomy surgeons have performed several thousand vasectomies over the last 12 years for the community. How soon can I expect an appointment? Appointments are generally within two weeks. Please let us know which surgeon you would like to see: Mr M. Ashraf Nottingham Road Clinic Mansfield Mr M. Ashraf Balderton/Newark Dr M. Atkinson Carlton – Park House Dr M. Atkinson Balderton/Newark Dr A. Hopwood Bramcote Dr R. Martin Sneinton TBA Dr H. Pabla Bullwell What is a vasectomy? This is the male form of sterilisatio n perform ed as a minor operation under local anaesthetic. What doe s the operation involve? The skin and tubes are numbed with local anaesthetic.The operation uses a No Scalpel ‘nick’ in the skin of the scrotum to retrieve the two vas tubes which carry the sperm to the testicles.