Selective Laser Melting of Ti Alloy for Manufacturing the Prosthetic Elements
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Cobalt Chrome Alloy Strength Without Size… Achieving Rigid Fixation Without the Bulk
Cobalt Chrome Alloy Strength Without Size… Achieving Rigid Fixation Without the Bulk • Cobalt Chrome Alloy Rod, 5.5mm Diameter • Polaris™ Deformity System • Trivium™ Derotation System Customizable Spinal Deformity Correction The Polaris™ Deformity System is available in Titanium and Stainless Steel in both 5.5mm and 6.35mm diameter rods. We now offer three tensile strengths of Cobalt Chrome Alloy in 5.5mm diameter rods. Our rod options offer you the ability to customize deformity correction based on curve type, curve stiffness and rigidity, and desired curve correction. Polaris™ Cobalt Chrome Alloy and Stainless Steel rods are Titanium rods are offered in three grades. offered in three tensile strengths. Cobalt Chrome Alloy Stainless Steel Titanium • Available in 5.5mm • Available in 5.5mm • Available in 5.5mm and 6.35mm and 6.35mm • Imaging advantages due • Offered in Titanium alloy and Commercially Pure Titanium to its use with titanium • Retains the initial bend screws and hooks and provides rigid fixation • Less exertion required for bending • Maintaining high strength • Imaging advantages without compromising profile Low Standard CP Ti 5.5mm and Ti Alloy 5.5mm 6.35mm High Ti Alloy 6.35mm Material Comparison Characteristics Cobalt Chrome Alloy Stainless Steel Titanium Stiffness High High Low Strength High High Medium Corrosion Resistance Medium Low High Notch Sensitivity Medium Low High Imaging Compatibility Medium Low High Cobalt Chrome Alloy for Spinal Deformity Correction The Polaris™ Deformity System offers a 5.5mm diameter Cobalt Chrome Alloy (CoCrMo) rod, which is offered in three tensile strengths for use with Polaris™ Titanium Implants. CoCrMo has a history of use in various orthopedic implants, and provides rigid fixation while maintaining imaging capability. -
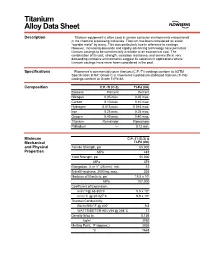
Titanium Alloy Data Sheet
M Titanium Alloy Data Sheet Description Titanium equipment is often used in severe corrosive environments encountered in the chemical processing industries. Titanium has been considered an exotic “wonder metal” by many. This was particularly true in reference to castings. However, increasing demands and rapidly advancing technology have permitted titanium castings to be commercially available at an economical cost. The combination of its cost, strength, corrosion resistance, and service life in very demanding corrosive environments suggest its selection in applications where titanium castings have never been considered in the past. Specifications Flowserve’s commercially pure titanium (C.P.-Ti) castings conform to ASTM Specification B367, Grade C-3. Flowserve’s palladium stabilized titanium (Ti-Pd) castings conform to Grade Ti-Pd 8A. Composition C.P.-Ti (C-3) Ti-Pd (8A) Element Percent Percent Nitrogen 0.05 max. 0.05 max. Carbon 0.10 max. 0.10 max. Hydrogen 0.015 max. 0.015 max. Iron 0.25 max. 0.25 max. Oxygen 0.40 max. 0.40 max. Titanium Remainder Remainder Palladium –– 0.12 min. Minimum C.P.-Ti (C-3) & Mechanical Ti-Pd (8A) and Physical Tensile Strength, psi 65,000 Properties MPa 448 Yield Strength, psi 55,000 MPa 379 Elongation, % in 1" (25 mm), min. 12 Brinell Hardness, 3000 kg, max. 235 Modulus of Elasticity, psi 15.5 x 106 MPa 107,000 Coefficient of Expansion, in/in/°F@ 68-800°F 5.5 x 10-6 m/m/°C @ 20-427°C 9.9 x 10-6 Thermal Conductivity, Btu/hr/ft/ft2/°F @ 400° 9.8 WATTS/METER-KELVIN @ 204°C 17 Density lb/cu in 0.136 kg/m3 3760 Melting Point, °F (approx.) 3035 °C 1668 Titanium Alloy Data Sheet (continued) Corrosion The outstanding mechanical and physical properties of titanium, combined with its Resistance unexpected corrosion resistance in many environments, makes it an excellent choice for particularly aggressive environments like wet chlorine, chlorine dioxide, sodium and calcium hypochlorite, chlorinated brines, chloride salt solutions, nitric acid, chromic acid, and hydrobromic acid. -

Fighting Wear and Corrosion on Stainless Steel and Titanium Accept …And Remember First - a Closer Look at Titanium Allotropic Crystal Structure
AcceptLearn Structure: 1. General Titanium & Titanium alloy knowledge 2. ExpaniteHard-Ti Fighting wear and corrosion on stainless steel and titanium Accept …And remember First - A closer look at Titanium Allotropic crystal structure “Soft one” “Hard one” Extremely generalized a (HCP) 882.5°C b (BCC) Learn First - A closer look at Titanium Classification and general properties: Commercially pure (CP) titanium, alpha and near alpha titanium alloys - Generally non-heat treatable and weldable - Medium strength, good creep strength, good corrosion resistance Alpha-beta titanium alloys - Heat treatable, good forming properties - Medium to high strength, good creep strength Beta titanium alloys - Heat treatable - Readily formable (in solution treated condition) - Very high strength, low ductility Learn First - A closer look at Titanium Classification and general properties: Alpha stabilizers: Al, Sn, O & N a a+b b Beta stabilizers: V, Mo, Cr, Cu, W, Nb. Learn First - A closer look at Titanium Classification and general properties: a - stabilized phase diagram Alpha stabilizers: Al, Sn, O & N Pure titanium 882.5°C a a+b b Beta stabilizers: V, Mo, Cr, Cu, W, Nb. Degree of alloying elements Accept First - A closer look at Titanium a Heat treatment Annealing at 700C produces a-phase Quenching from the b phase field results in a martensitic transformation, i.e. b is converted to HCP-a’ (with some retained b) Air cooling from the b phase field results in a so- called Widmanstätten structure of a-plates Accept First - A closer look at Titanium Near-a Heat treatment The alloy is heated up to the b region • Air-cooling gives Widmanstätten α structure with some b • Quenching gives transformation of b to lath α’ with some b; ageing results in precipitation of α. -

Research on Selective Laser Melting of Ti6al4v: Surface Morphologies, Optimized Processing Zone, and Ductility Improvement Mechanism
metals Article Research on Selective Laser Melting of Ti6Al4V: Surface Morphologies, Optimized Processing Zone, and Ductility Improvement Mechanism Di Wang 1,2 ID , Wenhao Dou 1 and Yongqiang Yang 1,* 1 School of Mechanical and Automotive Engineering, South China University of Technology, Guangzhou 510640, China; [email protected] (D.W.); [email protected] (W.D.) 2 School of Metallurgy and Materials, The University of Birmingham, Birmingham B152TT, UK * Correspondence: [email protected]; Tel./Fax: +86-020-8711-1036 Received: 24 May 2018; Accepted: 15 June 2018; Published: 21 June 2018 Abstract: The quality and mechanical properties of titanium alloy fabricated using selective laser melting (SLM) are critical to the adoption of the process which has long been impeded by the lack of uniformity in SLM-fabrication parameter optimization. In order to address this problem, laser power and scanning speed were combined into linear energy density as an independent variable, while surface morphology was defined as a metric. Based on full-factor experiments, the surface quality of SLM-fabricated titanium alloy was classified into five zones: severe over-melting zone, high-energy density nodulizing zone, smooth forming zone, low-energy density nodulizing zone, and sintering zone. The mechanism resulting in the creation of each zone was analyzed. Parameter uniformity was achieved by establishing a parameter window for each zone, and it also revealed that under smooth forming conditions, the relationship of linear energy density to the quality of the formed surface is not linear. It was also found that fabrication efficiency could be improved in the condition of the formation of a smooth surface by increasing laser power and scanning speed. -

Selective Laser Melting of Titanium Alloy with 50 Wt% Tantalum: Effect of Laser Process
Title: Selective Laser Melting of Titanium Alloy with 50 wt% Tantalum: Effect of Laser Process Parameters on Part Quality Authors: Swee Leong Sing a,b, (S.L. Sing) [email protected] Florencia Edith Wiria a,c, (F.E. Wiria) [email protected] Wai Yee Yeong a,b, (W.Y. Yeong) [email protected] +65 6790 4343 (corresponding author) Affiliations: a SIMTech-NTU Joint Laboratory (3D Additive Manufacturing), Nanyang Technological University Address: HW3-01-01, 65A Nanyang Drive, Singapore 637333 b Singapore Centre for 3D Printing, School of Mechanical & Aerospace Engineering, Nanyang Technological University Address: N3.1-B2C-03, 50 Nanyang Avenue, Singapore 639798 c Singapore Institute of Manufacturing Technology (SIMTech) @ NTU Address: 73 Nanyang Drive, Singapore 637662 Keywords: Additive manufacturing; 3D printing; Selective laser melting; Powder mixture; Titanium; Tantalum Abstract: Selective laser melting (SLM) is a powder bed fusion additive manufacturing (AM) technique that produces three-dimensional (3D) parts by fusing metallic powders with a high-energy laser. SLM involves numerous process parameters that may influence the properties of the final parts. Hence, establishing the effect of the SLM processing parameters is important for producing parts of high quality. In this study, titanium-tantalum alloy was fabricated by SLM using a customized powder blend to achieve in situ alloying. The influence of processing parameters on the microstructure and properties such as relative density, microhardness and surface roughness was investigated. The results show that fully dense titanium-tantalum parts can be obtained from SLM. With laser power of 360 W, scan speed of 400 mm/s, powder layer thickness of 0.05 mm and hatch spacing of 0.125 mm, the titanium-tantalum alloy produced by SLM has relative density of 99.85 ± 0.18 %. -

Applications of an Aluminum-Beryllium Composite for Structural Aerospace Components
Applications of an Aluminum -Beryllium Composite for Structural Aerospace Components William Speer and Omar S. Es -Said Mechanical Engineering Department, Loyola Marymount University, 7900 Loyola Blvd, Los Angeles, CA 90045 -8145, USA Abstract The us e of AlBeMet AM162, an aluminum -beryllium metal matrix composite, is an effective way to reduce the size and weight of many structural aerospace components that are currently made out of aluminum and titanium alloys. These savings, which are essential for today’s technologies, are primarily due to the material’s high modulus and low density combined with its better than average specific strength. The raw material costs are significantly higher than they are for traditional engineering alloys, and the avai lable billet sizes are more limited than they are for aluminum and titanium alloys. Although the material costs are higher for the aluminum -beryllium composite, ease of machining makes it financially competitive when compared to equivalent parts made out of titanium alloys. Due to toxic nature of beryllium, however, debris -generating operations must be strictly regulated to limit worker’s exposure to the material and protect them from potentially fatal diseases. Keywords: Metal matrix; AlBeMet; High el astic modulus; Low density; Weight reduction; Stiffness -driven design 1. Introduction The aerospace industry is continually searching for ways to reduce the weight of its products and maximize the amount of profit -making payload in launch vehicles. One o f the most common ways engineers reduce weight is to make their products out of low-density alloys or engineering composites. These materials offer very high strength and/or stiffness to weight ratios; therefore, they require less mass and take less space to support a given load in comparison to other material choices. -

ATI 45Nb™ Alloy
ATI 45Nb™ Alloy Technical Data Sheet ATI 45Nb™ Alloy Titanium Alloy INTRODUCTION Originally developed for application as an aerospace alloy because of its relative ease of formability, high strength and ductility at temperatures up to 427°C (801°F), ATI 45Nb™ Alloy is an ideal candidate for rivets that secure aluminum aircraft panels, particularly in areas exposed to high engine exhaust temperatures. This alloy has been used as welded flange components that secure high energy physics RF linear accelerator cavities (made from high purity niobium), and has been drawn into superconductivity wire. It is used as a medical device material for cochlear hearing implants and its low elastic modulus makes the material a consideration for a variety of medical and dental devices. ATI 45Nb™ Alloy is easily fabricated into structures and components. Although it is considered a refractory metal, processing techniques are the same as those for other titanium alloys. Parts are typically welded using the GTAW process but require the addition of trailing and backing shields and due to its simple metallurgical structure there is no requirement for post weld heat treatment. Machining requires the use of solid fixture setups, high torque at low RPM ridge machine tools with sharp high rake cutters. With an exceptionally small bend radius capability (down to a bend radius of 1t where t=sheet thickness) and low modulus of elasticity, ATI 45Nb™ Alloy is highly formable and yet still retains excellent tensile and elongation properties. It can also be cast into shapes with the same processes used to cast CP titanium. ATI 45Nb™ Alloy readily accepts surface oxidation treatment to enhance its hardness and wear resistance. -

Understanding the Properties of Low-Cost Iron-Containing Powder Metallurgy Titanium Alloys
Materials and Design 110 (2016) 317–323 Contents lists available at ScienceDirect Materials and Design journal homepage: www.elsevier.com/locate/matdes Understanding the properties of low-cost iron-containing powder metallurgy titanium alloys L. Bolzoni a,⁎, E.M. Ruiz-Navas b, E. Gordo b a WaiCAM (Waikato Centre for Advanced Materials), The University of Waikato, Private Bag 3105, 3240 Hamilton, New Zealand b Department of Materials Science and Engineering, University Carlos III of Madrid, Avda. de la Universidad, 30, 28911 Leganes, Madrid, Spain HIGHLIGHTS GRAPHICAL ABSTRACT • Low-cost iron-containing powder met- allurgy Ti-5%eq.Fe and Ti-7%eq.Fe alloys are designed. • Homogeneous microstructures are ob- tained using the appropriate sintering parameters. • The materials studied show mechanical behavior comparable to wrought α + β alloys. • The novel compositions are potential candidates for cheaper structural com- ponents. article info abstract Article history: The high production costs of titanium in comparison to other structural metals is the main limiting factor for the Received 22 April 2016 wide employment of titanium. Cost reduction can be addressed considering creative fabrication methods and/or Received in revised form 3 July 2016 formulating new chemical compositions. In this work the fabrication of low-cost iron-containing powder metal- Accepted 2 August 2016 lurgy titanium alloys is studied by using a spherical 85Fe/15Ni powder whose small particle size and spherical Available online 03 August 2016 morphology favours both the densification of the material and the diffusion of the alloying elements. The de- Keywords: signed composition are obtained by the blending elemental approach and processed by means of the convention- α β Low-cost titanium alloy al powder metallurgy route. -

TIMETAL Grade 12
Ti-0.8Ni-0.3Mo ® TIMETAL Grade 12 TITANIUM ALLOY WITH EXCELLENT CORROSION RESISTANCE AND STRENGTH TIMETAL® Grade 12 (ASTM Grade 12) is a lean titanium alloy with excellent corrosion resistance and higher strength than ASTM Grade 2. TIMETAL ® Grade 12 shows significant improvement over unalloyed titanium, particularly crevice corrosion in hot brines. It also offers excellent corrosion resistance to acids over unalloyed grades. The higher strength than Grade 2 or Grade 7 at room and elevated temperatures allow material and cost saving through use of thinner sections. Grade 12 is approved by ASME Boiler Code for use up to 600°F. TABLE 1 CHEMICAL COMPOSITION ELEMENT WEIGHT % Max. Nominal Molybdenum 0.4 0.3 TABLE 2 Nickel 0.9 0.8 PHYSICAL PROPERTIES Iron 0.30 0.15 PROPERTY VALUE Carbon 0.08 0.08 English SI 3 3 Nitrogen 0.03 0.03 Density 0.163 lb/in 4.51 g/cm Oxygen 0.25 0.12 Hydrogen 0.015 - Tensile Modulus Residuals (each) 0.10 Tension 15 Msi 103 GPa Residuals (total) 0.30 Torsion 6.2 Msi 42.7 GPa TABLE 3 SELECTED THERMAL PROPERTIES _ Temperature, Specific Heat Thermal Conductivity Coefficient of Thermal Expansion Electrical Resistivity, -6 °F Capacity, Btu/lb.°F λ, Btu/ft.h. °F 10 /°F µΩ.cm (°C) (J/kg) (W/m.K) (10-6/°C) 75 0.13 11 5.3 52 (24) (544) (19.02) (9.54) TABLE 4 MINIMUM MECHANICAL PROPERTIES _ 0.2% Yield Flatten Ability Flaring Ability (% Product UTS, ksi Strength, Elongation Minimum Bend Radius (distance Reduction in expansion of inside Form (MPa) ksi (%) (D/T) between Area diameter) (MPa) platens) All 70 50 18 For bar, billet, -

Progress on Titanium Spring-Baoliang
Ti-2007 Science and Technology, edited by M. Ninomi, S. Akiyama, M. Ikeda, M. Hagiwara, K. Maruyama The Japan Institute of Metals (2007) Progress on Titanium Spring Baoliang Bai, Jianchao Yang, Quan Hong Northwest Institute for Nonferrous Metal Research, Xi'an 710016, China For years the automotive industry has shown interest in titanium alloys for many automotive components. One of the limiting factors in titanium's acceptance over the years has been its relatively high price compared to standard materials. However, as the design engineers strive for lighter weight vehicles with improved performance and the materials manufacturers developed ways to reduce the cost and streamline processing, titanium has become more attractive. Titanium alloys offer weight savings, strength, corrosion resistance and modulus advantages over steels used for automotive applications. This paper addresses the current and potential uses for titanium alloys in spring application. Selected comparisons with conventional alloys are presented. Typical weight and performance advantages as well as a discussion relative to cost will also be made. Attention should be concentrated on the following three areas in the near future: (1) development of lower cost alloys; (2) exploration of low cost manufacturing methods; (3) evaluation of treatments to enhance wear resistance if necessary. Keywords: titanium(Ti), spring, progress, low cost 1. Introduction engineers can reduce the free height of the spring to 50-80% Uniquely among engineering alloys, titanium and titanium that of a comparable steel spring. This can translate into greater alloys possess the strength, density and modulus to make the styling and structural design freedom as well as improved ‘ideal’ spring for almost every application1~3). -

BALLISTIC EXPERIMENTS with TITANIUM and ALUMINUM TARGETS April 2001 6
DOT/FAA/AR-01/21 Ballistic Experiments With Office of Aviation Research Titanium and Aluminum Washington, D.C. 20591 Targets April 2001 Final Report This document is available to the U.S. public through the National Technical Information Service (NTIS), Springfield, Virginia 22161. U.S. Department of Transportation Federal Aviation Administration NOTICE This document is disseminated under the sponsorship of the U.S. Department of Transportation in the interest of information exchange. The United States Government assumes no liability for the contents or use thereof. The United States Government does not endorse products or manufacturers. Trade or manufacturer's names appear herein solely because they are considered essential to the objective of this report. This document does not constitute FAA certification policy. Consult your local FAA aircraft certification office as to its use. This report is available at the Federal Aviation Administration William J. Hughes Technical Center's Full-Text Technical Reports page: actlibrary.tc.faa.gov in Adobe Acrobat portable document format (PDF). Technical Report Documentation Page 1. Report No. 2. Government Accession No. 3. Recipient's Catalog No. DOT/FAA/AR-01/21 4. Title and Subtitle 5. Report Date BALLISTIC EXPERIMENTS WITH TITANIUM AND ALUMINUM TARGETS April 2001 6. Performing Organization Code 7. Author(s) 8. Performing Organization Report No. Raymond P. Gogolowski and Bruce R. Morgan 9. Performing Organization Name and Address 10. Work Unit No. (TRAIS) Lawrence Livermore National Laboratory P.O. Box 808 11. Contract or Grant No. Livermore, CA 94551 DTFA03-97-Z-90007 12. Sponsoring Agency Name and Address 13. Type of Report and Period Covered U.S. -

Comparative Quality Control of Titanium Alloy Ti–6Al–4V, 17–4 PH Stainless Steel, and Aluminum Alloy 4047 Either Manufactu
materials Article Comparative Quality Control of Titanium Alloy Ti–6Al–4V, 17–4 PH Stainless Steel, and Aluminum Alloy 4047 Either Manufactured or Repaired by Laser Engineered Net Shaping (LENS) Noam Eliaz 1,* , Nitzan Foucks 1,2, Dolev Geva 3, Shai Oren 2, Noy Shriki 2, Danielle Vaknin 2, Dimitry Fishman 2 and Ofer Levi 2 1 Biomaterials and Corrosion Lab, Department of Materials Science and Engineering, Tel-Aviv University, Ramat Aviv, Tel Aviv 6997801, Israel; [email protected] 2 Materials Science and Engineering Division, Depot 22, Israel Air Force, P.O. Box 02538, Tel Aviv, Israel; [email protected] (S.O.); [email protected] (N.S.); [email protected] (D.V.); dimitry.fi[email protected] (D.F.); [email protected] (O.L.) 3 Israel Ministry of Defense, Hakirya, Tel Aviv 61909, Israel; [email protected] * Correspondence: [email protected]; Tel.: +972-3-640-7384 Received: 21 August 2020; Accepted: 15 September 2020; Published: 19 September 2020 Abstract: Additive manufacturing attracts much interest for manufacturing and repair of structural parts for the aerospace industry. This paper presents comparative characterization of aircraft items made of Al 4047 alloy, Ti-6Al-4V alloy, and 17-4 precipitation hardened (PH) (AISI 630) stainless steel, either manufactured or repaired by laser engineered net shaping (LENS). Chemical analysis, density, and surface roughness measurements, X-ray micro-computed tomography (µ-CT) analysis, metallography, and micro-hardness testing were conducted. In all three materials, microstructures typical of rapid solidification were observed, along with high density, chemical composition, and hardness comparable to those of the counterpart wrought alloys (even in hard condition).