Title V Block Grant Needs Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Songs by Title Karaoke Night with the Patman
Songs By Title Karaoke Night with the Patman Title Versions Title Versions 10 Years 3 Libras Wasteland SC Perfect Circle SI 10,000 Maniacs 3 Of Hearts Because The Night SC Love Is Enough SC Candy Everybody Wants DK 30 Seconds To Mars More Than This SC Kill SC These Are The Days SC 311 Trouble Me SC All Mixed Up SC 100 Proof Aged In Soul Don't Tread On Me SC Somebody's Been Sleeping SC Down SC 10CC Love Song SC I'm Not In Love DK You Wouldn't Believe SC Things We Do For Love SC 38 Special 112 Back Where You Belong SI Come See Me SC Caught Up In You SC Dance With Me SC Hold On Loosely AH It's Over Now SC If I'd Been The One SC Only You SC Rockin' Onto The Night SC Peaches And Cream SC Second Chance SC U Already Know SC Teacher, Teacher SC 12 Gauge Wild Eyed Southern Boys SC Dunkie Butt SC 3LW 1910 Fruitgum Co. No More (Baby I'm A Do Right) SC 1, 2, 3 Redlight SC 3T Simon Says DK Anything SC 1975 Tease Me SC The Sound SI 4 Non Blondes 2 Live Crew What's Up DK Doo Wah Diddy SC 4 P.M. Me So Horny SC Lay Down Your Love SC We Want Some Pussy SC Sukiyaki DK 2 Pac 4 Runner California Love (Original Version) SC Ripples SC Changes SC That Was Him SC Thugz Mansion SC 42nd Street 20 Fingers 42nd Street Song SC Short Dick Man SC We're In The Money SC 3 Doors Down 5 Seconds Of Summer Away From The Sun SC Amnesia SI Be Like That SC She Looks So Perfect SI Behind Those Eyes SC 5 Stairsteps Duck & Run SC Ooh Child SC Here By Me CB 50 Cent Here Without You CB Disco Inferno SC Kryptonite SC If I Can't SC Let Me Go SC In Da Club HT Live For Today SC P.I.M.P. -
Spring 2019 Table of Contents “I’M at the Deep End” by Kayra Yavuz
Copy Write RJ Reynolds High School Literary Magazine Spring 2019 Table of Contents “I’m at the Deep End” by Kayra Yavuz .................4 “A Queen’s Pride” by Cayle Manning ...................5 “Bare Feet” by Jordan McCracken ........................6 “These Eyes” by Luna Jay .......................................7 “I am From” by Rama Alsakhita ...........................9 “Your Light-Your Love” by J.C. Jones ...................10 “Gina Gold” by Jordyn Reid ..................................12 “Untitled” by Tanya Avila ......................................14 “El Crepusculo” by Ella Mir ..................................16 “A Story in a Star” by Mattie Reeves .....................17 “The Savior” by Danny Saucedo ............................18 “A Childhood” by Amelia Rhodes .........................20 “A House” by Kenna Gokey ....................................22 “I am From” by Daphne Wishart ...........................24 “Untitled” by Mattie Reeves ....................................25 “Thank You” by Jalah Moore ...................................26 Copy Write Staff Cayle Manning, Jordan McCracken, Mattie Reeves, Kenna Gokey, Luna Jay Sponsor Stacey Jolly Special Thanks to Phil Benenati and his digital photography class “Black & Gold” Yearbook Editors Todd Echols and Maribeth Mohr 2 Parker Hunt and Michael Culbertson Dear Readers, Thank you so much for reading Copy Write! We are pleased to give you this 2019 edition of our annual magazine. In this edition, our central theme is the unveiling of your inner self. The emotions and experience that you hide from others. The stories that you are afraid of confessing or stories that are untold. Some of these stories and poems are things you may never hear from before or never experienced. These writings are about the effect of life itself has on others and themselves. This edition showcases the lightest parts of humanity to the darkest parts of it. -

61368/Sheet Music/9-36
10 Sheet Music Direct 11 Complete Alphabetical Sheet Listing 30 Wedding Sheet Music 30 Easy Piano Sheet Music 31 Piano Solo Sheet Music 33 Big-Note Piano Sheet Music 34 Five-Finger Sheet Music 34 Piano Duet Sheet Music 34 Vocal Sheet Music 35 Organ Sheet Music 35 Guitar Sheet Music 35 Accordion Sheet Music 35 Instrumental Sheet Music 10 SHEETSHEET MUSICMUSIC DIRECTDIRECT SHEET MUSIC The most popular site on the web for downloading top-quality, accurate, legal sheet music! Sheet Music Direct (www.SheetMusicDirect.com) features nearly 10,000 popular songs in a variety of musical and notation styles, ranging from piano/vocal to guitar tablature. More top songs are added to Sheet Music Direct daily and are searchable by title, artist, composer or format. With state-of-the-art Scorch® 2 technology from Sibelius®, sheet music files are quick to download, fun to interact with, and easy to use; visitors can see the music on screen, transpose the song to any key, and even listen to a MIDI file of the tune before you buy it! We have the strongest encryption commercially available so you can be assured that all transactions are completely safe. Hal Leonard offers excellent in-store and on-line affiliate programs: The In-Store Program allows you to sell your customers sheet music from a computer within your store. You can view the music, transpose to any key, test print it, and listen to it before the customer purchases it. The On-Line Affiliate Program allows you to place a link to SMD on your own website, and earn commissions on the sales that these click- These programs are available to any throughs generate. -

Marvin Brato Sr - Poems
Poetry Series Marvin Brato Sr - poems - Publication Date: 2015 Publisher: Poemhunter.com - The World's Poetry Archive Marvin Brato Sr(March 2,1960) I am a simple man with simple dreams, my sole happiness is to see my family healthy and happy! I work hard to make them happy. I love them more than anything else in this world, I won't give them up for silver or gold! I write poems (mostly acrostics) to express inner thoughts and emotions toward the various processes and essence of existence! Thank God for this life, it is very short hence make it useful! Spend it with your love ones, for when we are gone good memories are remembered. I work as Medical Technologist IV at Southern Philippines Medical Center formerly Davao Medical Center, a government hospital located in Davao City, Philippines. www.PoemHunter.com - The World's Poetry Archive 1 ' Cancer (10 Words) ' Resting on bed smiling to greet visitors awaiting my death! Marvin Brato Sr www.PoemHunter.com - The World's Poetry Archive 2 ' A Family (Acrostic) ' Being with family is best part, real world to spend meaningful life; and it is when you feel at home... to mingle with people you love. Family is the basic unit and the foundation of society. making peace and unity at home, is the secret of a progressive community. life shall become worthwhile for all the people yearning for a happy family is to make it happened. Marvin Brato Sr www.PoemHunter.com - The World's Poetry Archive 3 ' A First Love ' Reckoning love I obtain Overflowing like fountain. -

Legit Songlist
LEGIT SONGLIST Marvin Gaye / Tammy Terrell Ain't No Mountain High Enough 50S, 60S AND 70S Linda Ronstadt/Aaron Neville All My Life Heatwave Always and Forever Lonestar Amazed Jeff Healy Band Angel Eyes Toni Braxton Another Sad Love Song Carol King Anyone at All Etta James At Last Celine Dion Because You Love Me Elvis Presley Blue Suede Shoes R. Kelly Body Calling Johnnie C. Boogaloo Down Broadway The Foundations Build Me Up Buttercup Sade By Your Side James Ingram Can You Stop The Rain Elvis Presley Can't Help Falling in Love Otis Reading Can't Turn You Loose The Association Cherish Kenny Loggins Cody's Song Nora Jones Come Away With Me The Capitals Cool Jerk Van Morrison Crazy Love Nora Jones Don't Know Why Paul Simon Father Daughter Sting Fields of Gold Rod Stewart For the First Time Shania Twain/ Brian White From This Moment Whitney Houston Greatest Love of All Van Morrison Have I Told You Lately Celene Dion Have You Ever Been in Love Enrique Iglesias Hero Tricia Yearwood How Do I Live Without You James Taylor How Sweet It Is Aerosmith I Don't Want To Miss A Thing James Brown I Feel Good Barbra Streisand/Bryon Adams I Finally Found Someone Jackson Five I Want You Back Whitney Houston I Will Always Love You Stevie Wonder I Wish The Spinners I'll Be Around Van Morrison I'll be Your Lover Too R. Kelly/Celine Dion I'm Your Angel Alicia Keys If I Ain't Got You Ray Charles If I Could Beatles In My Life Elvis Presley Jail House Rock Smokey Robinson Just My Imagination Billy Joel Just The Way You Are Ritchie Valens La Bamba Elvis Presley Love Me Tender Brian McNight Love of My Life Billy Joel Lullaby Kelly Clark Moment Like This Kelly Clark Moments In Time Eddie Vinson Mr. -

Songs by Artist
YouStarKaraoke.com Songs by Artist 602-752-0274 Title Title Title 1 Giant Leap 1975 3 Doors Down My Culture City Let Me Be Myself (Wvocal) 10 Years 1985 Let Me Go Beautiful Bowling For Soup Live For Today Through The Iris 1999 Man United Squad Loser Through The Iris (Wvocal) Lift It High (All About Belief) Road I'm On Wasteland 2 Live Crew The Road I'm On 10,000 MANIACS Do Wah Diddy Diddy When I M Gone Candy Everybody Wants Doo Wah Diddy When I'm Gone Like The Weather Me So Horny When You're Young More Than This We Want Some PUSSY When You're Young (Wvocal) These Are The Days 2 Pac 3 Doors Down & Bob Seger Trouble Me California Love Landing In London 100 Proof Aged In Soul Changes 3 Doors Down Wvocal Somebody's Been Sleeping Dear Mama Every Time You Go (Wvocal) 100 Years How Do You Want It When You're Young (Wvocal) Five For Fighting Thugz Mansion 3 Doors Down 10000 Maniacs Until The End Of Time Road I'm On Because The Night 2 Pac & Eminem Road I'm On, The 101 Dalmations One Day At A Time 3 LW Cruella De Vil 2 Pac & Eric Will No More (Baby I'ma Do Right) 10CC Do For Love 3 Of A Kind Donna 2 Unlimited Baby Cakes Dreadlock Holiday No Limits 3 Of Hearts I'm Mandy 20 Fingers Arizona Rain I'm Not In Love Short Dick Man Christmas Shoes Rubber Bullets 21St Century Girls Love Is Enough Things We Do For Love, The 21St Century Girls 3 Oh! 3 Wall Street Shuffle 2Pac Don't Trust Me We Do For Love California Love (Original 3 Sl 10CCC Version) Take It Easy I'm Not In Love 3 Colours Red 3 Three Doors Down 112 Beautiful Day Here Without You Come See Me -

Adult Contemporary
ADULT CONTEMPORARY Click to open ‘bookmarks’ on left side for easier search Song Title Artist Song Title Artist TURN THE BEAT AROUND GLORIA ESTEFAN POMP & CIRCUMSTANCE BOSTON POPS FADE INTO YOU MAZZY STAR NOBODY DOES IT BETTER CARLY SIMON DREAM ON AEROSMITH POWER OF LOVE CELINE DION ALL OUT OF LOVE AIR SUPPLY BEHIND CLOSED DOORS CHARLIE RICH HEAD OVER FEET ALANIS MORISSETTE THE MOST BEAUTIFUL GIRL CHARLIE RICH IRONIC ALANIZ MORISSETTE WICKED GAME CHRIS ISAAK EVERY HEARTBEAT AMY GRANT I WILL TAKE YOU FOREVER CHRISTOPHER CROSS LOVE STORY ANDY WILLIAMS SAILING CHRISTOPHER CROSS MAY EACH DAY ANDY WILLIAMS LONGER DAN FOGELBERG MOON RIVER ANDY WILLIAMS SOMETIMES WHEN WE TOUCH DAN HILL MORE ANDY WILLIAMS GOOD TIMES DAN SEALS THEME FROM THE GODFATHER ANDY WILLIAMS WHERE ARE YOU GOING DAVE MATTHEWS WISHIN & HOPIN ANI DEFRANCO WAIT A LITTLE WHILE DAVEKOZ I ONLY HAVE EYES FOR YOU ART GARFUNKEL LADY IS A TRAMP DAVID HUNTSINGER EVERGREEN BARBARA STREISAND THAT'S WHAT FRIENDS ARE FOR DIONNE WARWICK MEMORY BARBARA STREISAND NEVER ON A SUNDAY DON COSTA BARBRA STREISAND / HEARTACHE TONIGHT EAGLES I FINALLY FOUND SOMEONE BRYAN ADAMS SHINING STAR EARTH WIND & FIRE BARBRA STREISAND / NEIL LA VIE EN ROSE EDITH PIAF YOU DON'T BRING ME FLOWERS DIAMOND I'LL BE EDWIN MCCAIN COPACABANA 1993 BARRY MANILOW BLESSED ELTON JOHN I WRITE THE SONGS BARRY MANILOW CIRCLE OF LIFE ELTON JOHN MANDY BARRY MANILOW ROCKET MAN ELTON JOHN BOOGIE WOOGIE BUGLE BOY BETTE MIDLER TINY DANCER ELTON JOHN FROM A DISTANCE BETTE MIDLER ENGELBERT THE ROSE BETTE MIDLER AFTER THE LOVIN' HUMPERDINCK -

First Dance/Parent Dance Suggestions
Love Song Suggestions BUTCH GRAY DISC JOCKEY/ ENTERTAINER, LLC 815 Flanders Road Southington, Connecticut 06489 860.306.5560 [email protected] www.butchgraydj.com To Make You Feel My Love - Trisha Year- First Dance: wood Tonight I Celebrate My Love - Peabo Bryson Always and Forever - Heatwave / Roberta Flack Always - Atlantic Star True Companion - Marc Cohn Amazed - Lonestar Unchained Melody - Righteous Brothers Angel Eyes - Jeff Healey We've Only Just Begun - The Carpenters At Last - Etta James When A Man Loves A Woman - Percy Sledge Beautiful In My Eyes - Joshua Kadison When I Said I Do - Clint Black Because You Loved Me - Celine Dion Wonderful Tonight - Eric Clapton Breathe - Faith Hill You're Still The One - Shania Twain Can't Help Falling In Love - Elvis Presley Could I Have This Dance - Anne Murray Mother-Son Dance: Dance of Love - Dan Hill Crazy - Patsy Cline A Song For My Son - Vickie Mereck Endless Love - Diana Ross / Lionel Ritchie Wind Beneath My Wings - Bette Midler Everything I Do - Bryan Adams I'll Be - Reba McIntyre Faithfully - Journey I Hope You Dance - Leann Womack Forever and Ever, Amen - Randy Travis A Song For Mama - Boys II Men From Here To Eternity - Michael Peterson From This Moment - Shania Twain - Bryan Mother-Daughter Dance: White Give Me Forever I Do - James Ingram / John Tesh Because You Loved Me - Celine Dion Grow Old With Me - Mary Chapin Carpenter Through The Years - Kenny Rogers Have I Told You Lately - Rod Stewart Wind Beneath My Wings - Bette Midler Have I Told You Lately - Van Morrison 26 cents - -

Sweet Adelines International Arranged Music List
Sweet Adelines International Arranged Music List ID# Song Title Arranger I03803 'TIL I HEAR YOU SING (From LOVE NEVER DIES) June Berg I04656 (YOUR LOVE HAS LIFTED ME) HIGHER AND HIGHER Becky Wilkins and Suzanne Wittebort I00008 004 MEDLEY - HOW COULD YOU BELIEVE ME Sylvia Alsbury I00011 005 MEDLEY - LOOK FOR THE SILVER LINING Mary Ann Wydra I00020 011 MEDLEY - SISTERS Dede Nibler I00024 013 MEDLEY - BABY WON'T YOU PLEASE COME HOME* Charlotte Pernert I00027 014 MEDLEY - CANADIAN MEDLEY/CANADA, MY HOME* Joey Minshall I00038 017 MEDLEY - BABY FACE Barbara Bianchi I00045 019 MEDLEY - DIAMONDS - CONTEST VERSION Carolyn Schmidt I00046 019 MEDLEY - DIAMONDS - SHOW VERSION Carolyn Schmidt I02517 028 MEDLEY - I WANT A GIRL Barbara Bianchi I02521 031 MEDLEY - LOW DOWN RYTHYM Barbara NcNeill I00079 037 MEDLEY - PIGALLE Carolyn Schmidt I00083 038 MEDLEY - GOD BLESS THE U.S.A. Mary K. Coffman I00139 064 CHANGES MEDLEY - AFTER YOU'VE GONE* Bev Sellers I00149 068 BABY MEDLEY - BYE BYE BABY Carolyn Schmidt I00151 070 DR. JAZZ/JAZZ HOLIDAY MEDLEY - JAZZ HOLIDAY, Bev Sellers I00156 072 GOODBYE MEDLEY - LIES Jean Shook I00161 074 MEDLEY - MY BOYFRIEND'S BACK/MY GUY Becky Wilkins I00198 086 MEDLEY - BABY LOVE David Wright I00205 089 MEDLEY - LET YOURSELF GO David Briner I00213 098 MEDLEY - YES SIR, THAT'S MY BABY Bev Sellers I00219 101 MEDLEY - SOMEBODY ELSE IS TAKING MY PLACE Dave Briner I00220 102 MEDLEY - TAKE ANOTHER GUESS David Briner I02526 107 MEDLEY - I LOVE A PIANO* Marge Bailey I00228 108 MEDLEY - ANGRY Marge Bailey I00244 112 MEDLEY - IT MIGHT -

Songs by Artist
Sound Master Entertianment Songs by Artist smedenver.com Title Title Title .38 Special 2Pac 4 Him Caught Up In You California Love (Original Version) For Future Generations Hold On Loosely Changes 4 Non Blondes If I'd Been The One Dear Mama What's Up Rockin' Onto The Night Thugz Mansion 4 P.M. Second Chance Until The End Of Time Lay Down Your Love Wild Eyed Southern Boys 2Pac & Eminem Sukiyaki 10 Years One Day At A Time 4 Runner Beautiful 2Pac & Notorious B.I.G. Cain's Blood Through The Iris Runnin' Ripples 100 Proof Aged In Soul 3 Doors Down That Was Him (This Is Now) Somebody's Been Sleeping Away From The Sun 4 Seasons 10000 Maniacs Be Like That Rag Doll Because The Night Citizen Soldier 42nd Street Candy Everybody Wants Duck & Run 42nd Street More Than This Here Without You Lullaby Of Broadway These Are Days It's Not My Time We're In The Money Trouble Me Kryptonite 5 Stairsteps 10CC Landing In London Ooh Child Let Me Be Myself I'm Not In Love 50 Cent We Do For Love Let Me Go 21 Questions 112 Loser Disco Inferno Come See Me Road I'm On When I'm Gone In Da Club Dance With Me P.I.M.P. It's Over Now When You're Young 3 Of Hearts Wanksta Only You What Up Gangsta Arizona Rain Peaches & Cream Window Shopper Love Is Enough Right Here For You 50 Cent & Eminem 112 & Ludacris 30 Seconds To Mars Patiently Waiting Kill Hot & Wet 50 Cent & Nate Dogg 112 & Super Cat 311 21 Questions All Mixed Up Na Na Na 50 Cent & Olivia 12 Gauge Amber Beyond The Grey Sky Best Friend Dunkie Butt 5th Dimension 12 Stones Creatures (For A While) Down Aquarius (Let The Sun Shine In) Far Away First Straw AquariusLet The Sun Shine In 1910 Fruitgum Co. -

Catalogue Karaoke
CHANSONS ANGLAISES A A A 1 CAUGHT IN THE MIDDLE NO MORE SAME OLD BRAND NEW YOU Aallyah THE ONE I GAVE MY HEART TO Aaliyah & Timbaland WE NEED A RESOLUTION Abba CHIQUITITA DANCING QUEEN KNOWING ME AND KNOWING YOU MONEY MONEY MONEY SUPER TROUPER TAKE A CHANCE ON ME THANK YOU FOR THE MUSIC Ace of Base ALL THAT SHE WANTS BEAUTIFUL LIFE CRUEL SUMMER DON'T TURN AROUND LIVING IN DANGER THE SIGN Adrews Sisters BOOGIE WOOGIE BUGLE BOY Aerosmith I DON'T WANT TO MISS A THING SAME OLD SONG AND DANCE Afroman BECAUSE I GOT HIGH After 7 TILL YOU DO ME RIGHT Air Supply ALL OUT OF LOVE LOST IN LOVE Al Green LET'S STAY TOGETHER TIRED OF BEING ALONE Al Jolson ANNIVERSARY SONG Al Wilson SHOW AND TELL Alabama YOU'VE GOT THE TOUCH Aladdin A WHOLE NEW WORLD Alanis Morissette EVERYTHING IRONIC PRECIOUS ILLUSIONS THANK YOU Alex Party DON'T GIVE ME YOUR LIFE Alicia Keys FALLIN' 31 CHANSONS ANGLAISES HOW COME YOU DON'T CALL ME ANYMORE IF I AIN'T GOT YOU WOMAN'S WORTH Alison Krauss BABY, NOW THAT I'VE FOUND YOU All 4 One I CAN LOVE YOU LIKE THAT I CROSS MY HEART I SWEAR All Saints ALL HOOKED UP BOTIE CALL I KNOW WHERE IT’S AT PURE SHORES Allan Sherman HELLO MUDDUH, HELLO FADDUH ! Allen Ant Fam SMOOTH CRIMINAL Allure ALL CRIED OUT Amel Larrieux FOR REAL America SISTER GOLDEN HAIR Amie Stewart KNOCK ON WOOD Amy Grant BABY BABY THAT'S WHAT LOVE IS FOR Amy Studt MISFIT Anastacia BOOM I'M OUTTA LOVE LEFT OUTSIDE ALONE MADE FOR LOVING YOU WHY'D YOU LIE TO ME Andy Gibb AN EVERLASTING LOVE Andy Stewart CAMPBELTOWN LOCH Andy Williams CAN'T GET USED TO LOSING YOU MOON RIVER -
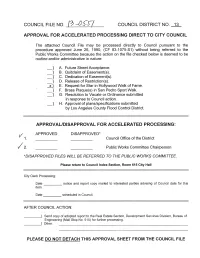
Engineering (Mail Stop No
COUNCIL FILE NO. 13 -fJS-S7 COUNCIL DISTRICT NO. 13 i APPROVAL FOR ACCELERATED PROCESSING DIRECT TO CITY COUNCIL The attached Council File may be processed directly to Council pursuant to the procedure approved June 26, 1990, (CF 83-1075-S1) without being referred to the Public Works Committee because the action on the file checked below is deemed to be routine and/or administrative in nature: } A. Future Street Acceptance. -} B. Quitclaim of Easement(s). -} C. Dedication of Easement(s). -} D. Release of Restriction(s). -20 E. Request for Star in Hollywood Walk of Fame. -} F. Brass Plaque(s) in San Pedro Sport Walk. } G. Resolution to Vacate or Ordinance submitted in response to Council action. } H. Approval of plans/specifications submitted by Los Angeles County Flood Control District. APPROVAL/DISAPPROVAL FOR ACCELERATED PROCESSING: APPROVED DISAPPROVED* Council Office of the District Public Works Committee Chairperson *DISAPPROVED FILES WILL BE REFERRED TO THE PUBLIC WORKS COMMITTEE. Please return to Council Index Section, Room 615 City Hall City Clerk Processing: Date notice and report copy mailed to interested parties advising of Council date for this item. Date scheduled in Council. AFTER COUNCIL ACTION: ____ I Send copy of adopted report to the Real Estate Section, Development Services Division, Bureau of Engineering (Mail Stop No. 515) for further processing. ____ I Other: PLEASE DO NOT DETACH THIS APPROVAL SHEET FROM THE COUNCIL FILE ACCELERATED REVIEW PROCESS - E Office of the City Engineer Los Angeles California To the Honorable Council APR (; t 2013 Of the City of Los Angeles Honorable Members: C. D.