Neutrophil Extracellular Traps in the Pathogenesis of Equine Recurrent Uveitis (ERU)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Equine Uveitis Lauren Hughes, DVM
New England Equine Medical & Surgical Center 15 Members Way · Dover NH 03820 · www.newenglandequine.com · 603.749.9111 Understanding Equine Uveitis Lauren Hughes, DVM One of the most common ocular diseases affecting the horse is a condition known as uveitis. This occurs when inflammation affects the uveal tract of the eye that is composed of the iris, ciliary body and choroid. This inflammation can be caused by a variety of conditions including ocular, systemic or immune mediated disease. Fig 1. Equine Eye Cross-Sectional Anatomy Understanding Uveitis In order to better understand uveitis we need to take a closer look at the causes of this relatively common disease. 1-Ocular- Any condition that affects the eye can lead to uveitis as a secondary complication. This includes trauma, corneal ulcers, intraocular tumors, and cataracts (which cause lens-induced uveitis). 2-Systemic- Many infectious diseases can also predispose a horse to development of uveitis. These diseases can be bacterial, viral, parasitic, or neoplastic, with one of the most recognized being the bacterial disease Leptospirosis. 3-Immune Mediated- The most commonly seen presentation of uveitis is an immune mediated form known as equine recurrent uveitis (ERU) or moon blindness. This disease consists of recurrent episodes of inflammation in which the immune system targets the tissues of the eye. This can be an ongoing and frustrating condition for owners as treatment is not curative and lifelong management is often necessary. This condition has been reported to affect upwards of 25% of the horse population with increased prevalence in certain breeds including Appaloosas, draft horses, and warmbloods.1 It can affect one or both eyes, with chronicity potentially leading to permanent vision deficits or blindness. -

List of Horse Breeds 1 List of Horse Breeds
List of horse breeds 1 List of horse breeds This page is a list of horse and pony breeds, and also includes terms used to describe types of horse that are not breeds but are commonly mistaken for breeds. While there is no scientifically accepted definition of the term "breed,"[1] a breed is defined generally as having distinct true-breeding characteristics over a number of generations; its members may be called "purebred". In most cases, bloodlines of horse breeds are recorded with a breed registry. However, in horses, the concept is somewhat flexible, as open stud books are created for developing horse breeds that are not yet fully true-breeding. Registries also are considered the authority as to whether a given breed is listed as Light or saddle horse breeds a "horse" or a "pony". There are also a number of "color breed", sport horse, and gaited horse registries for horses with various phenotypes or other traits, which admit any animal fitting a given set of physical characteristics, even if there is little or no evidence of the trait being a true-breeding characteristic. Other recording entities or specialty organizations may recognize horses from multiple breeds, thus, for the purposes of this article, such animals are classified as a "type" rather than a "breed". The breeds and types listed here are those that already have a Wikipedia article. For a more extensive list, see the List of all horse breeds in DAD-IS. Heavy or draft horse breeds For additional information, see horse breed, horse breeding and the individual articles listed below. -

Leptospirosis Associated Equine Recurrent Uveitis Answers to Your Important Questions What Is Leptospirosis Associated Equine Recurrent Uveitis (LAERU)?
Lisa Dauten, DVM Tri-State Veterinary Services LLC " Leptospirosis Associated Equine Recurrent Uveitis Answers to your Important Questions! What is Leptospirosis Associated Equine Recurrent Uveitis (LAERU)? Let’s start by breaking down some terminology.! Uveitis- inflammation of the uvea. Resulting in cloudiness of the eye, pain, and potential blindness. Also know as “Moon Blindness”. Caused by trauma, infection, or corneal disease.! Uvea- part of the eye containing the iris, ciliary body, and choroid. It keeps the lens of the eye in place, maintains fluid in the eye, and keeps things in the blood from entering the inside of the eye (blood-ocular barrier). ! Recurrent Uveitis- inflammation of the uvea that sporadically reoccurs through out a horses life time. Each time there is a reoccurring episode, the damage to the eye is made worse, eventually leading to permanent damage and potential blindness. ! Leptospirosis- bacteria found in the environment shed in the urine of wildlife and livestock. Horses usually are exposed when grazing pastures or drinking from natural water sources.! LAERU- Recurrent Uveitis in horses caused by Leptospirosis.! What are the clinical signs of Uveitis? Uveitis can come on very suddenly. A lot of times horses present with severe pain in the eye, tearing, squinting, and rubbing face. The eye itself is cloudy, white or blue in color. Sometimes the signs are not as dramatic. The color change of the eye may progress slowly. In these cases, horse owners may mistake the changes for cataracts.! What do I do if I think my horse has Uveitis? Call your veterinarian to request an appointment. -

Electronic Supplementary Material - Appendices
1 Electronic Supplementary Material - Appendices 2 Appendix 1. Full breed list, listed alphabetically. Breeds searched (* denotes those identified with inherited disorders) # Breed # Breed # Breed # Breed 1 Ab Abyssinian 31 BF Black Forest 61 Dul Dülmen Pony 91 HP Highland Pony* 2 Ak Akhal Teke 32 Boe Boer 62 DD Dutch Draft 92 Hok Hokkaido 3 Al Albanian 33 Bre Breton* 63 DW Dutch Warmblood 93 Hol Holsteiner* 4 Alt Altai 34 Buc Buckskin 64 EB East Bulgarian 94 Huc Hucul 5 ACD American Cream Draft 35 Bud Budyonny 65 Egy Egyptian 95 HW Hungarian Warmblood 6 ACW American Creme and White 36 By Byelorussian Harness 66 EP Eriskay Pony 96 Ice Icelandic* 7 AWP American Walking Pony 37 Cam Camargue* 67 EN Estonian Native 97 Io Iomud 8 And Andalusian* 38 Camp Campolina 68 ExP Exmoor Pony 98 ID Irish Draught 9 Anv Andravida 39 Can Canadian 69 Fae Faeroes Pony 99 Jin Jinzhou 10 A-K Anglo-Kabarda 40 Car Carthusian 70 Fa Falabella* 100 Jut Jutland 11 Ap Appaloosa* 41 Cas Caspian 71 FP Fell Pony* 101 Kab Kabarda 12 Arp Araappaloosa 42 Cay Cayuse 72 Fin Finnhorse* 102 Kar Karabair 13 A Arabian / Arab* 43 Ch Cheju 73 Fl Fleuve 103 Kara Karabakh 14 Ard Ardennes 44 CC Chilean Corralero 74 Fo Fouta 104 Kaz Kazakh 15 AC Argentine Criollo 45 CP Chincoteague Pony 75 Fr Frederiksborg 105 KPB Kerry Bog Pony 16 Ast Asturian 46 CB Cleveland Bay 76 Fb Freiberger* 106 KM Kiger Mustang 17 AB Australian Brumby 47 Cly Clydesdale* 77 FS French Saddlebred 107 KP Kirdi Pony 18 ASH Australian Stock Horse 48 CN Cob Normand* 78 FT French Trotter 108 KF Kisber Felver 19 Az Azteca -

Analysis of Breed Effects and Genetic Parameters of Semen Quality Traits for Frozen-Thawed Semen in Stallions
University of Veterinary Medicine Hannover Analysis of breed effects and genetic parameters of semen quality traits for frozen-thawed semen in stallions Thesis Submitted in partial fulfilment of the requirements for the degree -Doctor of Veterinary Medicine- Doctor medicinae veterinariae (Dr. med. vet.) by Theresa Madeleine Greiser München Hannover 2019 Academic supervision: Univ.-Prof. Dr. Dr. Harald Sieme Clinic for horses, Unit for Reproduction Medicine Univ.-Prof. Dr. Dr. habil. Ottmar Distl Institute for Animal Breeding and Genetics 1. Referee: Univ.-Prof. Dr. Dr. habil. Ottmar Distl 2. Referee: Prof. Dr. med. vet. Detlef Rath Day of oral examination: 15.11.2019 To my children Parts of this work have been published in the following journals: 1. Theriogenology 2. Animal Reproduction Science Table of contents 1. Introduction ........................................................................................................................ 2 Chapter contents ............................................................................................................... 2 2. Breed and stallion effects on frozen-thawed semen in warmblood, Light and Quarter horses ................................................................................................................................... 6 2.1 Abstract ....................................................................................................................... 6 2.2 Introduction ................................................................................................................ -

An Analysis of the Inbreeding Level of Holstein Stallions Presented for Classification in 2003–2012
Acta Sci. Pol. Zootechnica 16(2) 2017, 35–38 www.asp.zut.edu.pl pISSN 1644-0714 eISSN 2300-6145 DOI:10.21005/asp.2017.16.2.05 Received: 24.05.2017 ORIGINAL PAPER Accepted: 17.08.2017 AN ANALYSIS OF THE INBREEDING LEVEL OF HOLSTEIN STALLIONS PRESENTED FOR CLASSIFICATION IN 2003–2012 Ryszard Pikuła1B, Wilhelm Grzesiak2, Daniel Zaborski2, Wioletta Werkowska1 1Laboratory of Horse Breeding and Animal Assisted Therapy, West Pomeranian University of Technology, Szczecin, Doktora Judyma 14, 71-466 Szczecin, Poland 2Department of Ruminants Science, West Pomeranian University of Technology, Szczecin, Klemensa Janickiego 29, 71-466 Szczecin, Poland ABSTRACT The aim of the present study was to analyze and compare the inbreeding level of the Holstein stallions presented for classification for breeding in 2003–2012 in Germany. The data were collected from the Holsteiner Körung und Reitepferde – Auktion catalogues. Based on the analysis of 869 pedigrees (up to the fifth generation inclusive), inbreeding coefficients (F), expressed as a percentage for each stallion, were calculated. The highest F values were recorded in 2003 (2.05%) and 2004 (1.74%). Statistically significant differences in the F values of the stallions from individual years were found. The outcomes of the present study show that the breeding work based on conscious assumptions is carried out in order to increase an inbreeding level in the sport horses’ production, regarding at the same time that the value of the inbreeding coefficient cannot be too high. Key words: inbreeding, Holstein, stallions, classification, breeding INTRODUCTION standing ancestors and subsequently consolidating desi- red traits [Pikuła and Werkowska 2009, 2011a, 2011b]. -

Equine Recurrent Uveitis Slowly Releases Medication Over a Period of (ERU) Several Years
Treatment ABOUT THE COLLEGE OF VETERINARY MEDICINE Treatment for uveitis in general depends upon the underlying cause as well as Ranked third in the nation among the severity of the symptoms. In most colleges of veterinary medicine by cases, the eye is treated with topical anti- U.S. News & World Report, NC State’s inflammatories and a pupil-dilating agent to College of Veterinary Medicine is a decrease the pain and inflammation. Oral driving force in veterinary innovation. anti-inflammatories such as Banamine® From our leadership in understanding (Flunixin meglumine) are also instituted, and and defining the interconnections in select cases bodily injections of steroids between animal and human health, to may be necessary. While these treatments groundbreaking research in areas like are helpful in subsiding the inflammation equine health, and our commitment to and pain - they’re not ideal for long-term training the next generation of veterinary use. If infectious disease is suspected to health professionals, we are dedicated be the cause, laboratory tests should be to advancing animal and human health performed followed by medical treatment if from the cellular level through entire recommended. ecosystems. If a horse responds favorably to medical therapy, Cyclosporine Implants may be an option for long-term management. This is the surgical implantation of a small Cyclosporine medicated disc that’s placed deep within the pink tissue surrounding the eye (sclera), it Equine Recurrent Uveitis slowly releases medication over a period of (ERU) several years. This medication modifies the reaction to the immune system and reduces NC State Veterinary Hospital Moon Blindness; Periodic Ophthalamia inflammation. -

Immune Responses to Retinal Autoantigens and Peptides in Equine Recurrent Uveitis
Immune Responses to Retinal Autoantigens and Peptides in Equine Recurrent Uveitis Cornelia A. Deeg,1 Bernd Kaspers,1 Hartmut Gerhards,2 Stephan R. Thurau,3 Bettina Wollanke,2 and Gerhild Wildner3 5 PURPOSE. To test the hypothesis that autoimmune mechanisms unclear. Research has focused on the identification of infec- are involved in horses in which equine recurrent uveitis (ERU) tious agents that may induce uveitis, such as bacteria, viruses, develops spontaneously. or parasites, especially on a possible role for Leptospira inter- 6–8 METHODS. Material obtained from horses treated for spontane- rogans as an initiating agent in this process. However, the ous disease by therapeutic routine vitrectomy was analyzed for concept of an infectious factor that exclusively induces and total IgG content and IgG specific for S-Antigen (S-Ag) and maintains the disease is not sufficient to explain certain aspects interphotoreceptor retinoid-binding protein (IRBP). The cellu- of the clinical course and therapeutic approaches. Because of the recurrence of inflammation,5 the positive effect of cortico- lar infiltrate of the vitreous was analyzed by differential counts 2 of cytospin preparations and flow cytometry using equine steroids, and the insufficient therapeutic success of antibiot- lymphocyte-specific antibodies. Antigen-specific proliferation ics, the concept has emerged that the disease is immune assays were performed comparing peripheral blood lympho- mediated. Therefore, ERU is of high value for studying uveitis, because horses represent the only species besides humans in cytes (PBLs) with vitreal lymphocytes by stimulation with S-Ag 9 and several S-Ag– and IRBP-derived peptides. which recurrent uveitis develops spontaneously. -

Breeding Programme for Oldenburg Horses
Breeding Programme for Oldenburg Horses Verband der Züchter des Oldenburger Pferdes e.V. Grafenhorststr. 5 · 49377 Vechta · Germany Telephone: 04441 -9355 -0 Fax: 04441 -9355 -99 [email protected] www.oldenburger-pferde.com Breeding Programme for Oldenburg Horses Breeding Programme for Oldenburg Horses 1. Information on the Studbook.....................................................................................................3 2. Geographical area ....................................................................................................................3 3. Size of the breeding population ................................................................................................3 4. Breeding goal ...........................................................................................................................3 5. Characteristic features and qualities .........................................................................................3 5.1. Exterior .....................................................................................................................................3 5.2. Movement incl. jumping ............................................................................................................4 5.3 Interior qualities .........................................................................................................................5 6. Selection characteristics ...........................................................................................................5 -
Stallions Dates 2016
STALLIONS DATES 2016 Saturday, February 13th, 6:00 p.m. July 15th to 17th August 31st to September 4th Westphalian Private Stallion Show DLZ information stand at LVM German DLZ information stand at German in Münster-Handorf Foal Championships in Lienen Championships in Warendorf Sunday, February 21st, 2:00 p.m. July 19th to 24th Sunday, December 11th, 11:00 a.m. Stallion Show with Ludger Beerbaum DLZ information stand at Oldenburg Breeders Advent in Lodbergen Stables, Stallion Station Ahlers and Championships in Rastede Stallion Station Holtwiesche in Vechta Saturday, February 27th, 7:00 p.m. Stallion Show DLZ Riding Hall at Dobrock in Wingst Friday, March 4th, 7:00 p.m. Stallion Show in Timmel Mid-/end of March Private Stallion Show Rhineland Horse Center in Wickrath Sunday, April 10th, 11:00 a.m. Breeders Spring in Lodbergen Monday, April 25th Oldenburger and OS Early-Branding Date in Lodbergen Thursday, June 23rd Oldenburger and OS Branding Date in Lodbergen Thursday, June 30th, 9:00 a.m. LVM qualifier for the German Foal Championships in Lodbergen WELCOME BACK TO OUR BREEDING STATION IN LODBERGEN! 2015 was a year of growth and consistency and available for breeding. The latter ranks The DLZ was able to deploy five self- for Dressurpferde Leistungszentrum Lod- eighth in the list of world’s most successful prepared and licensed stallions at several bergen (Performance Center for Dressage dressage sires. licensing events last year, among them Horses in Lodbergen; DLZ). Due to our stal- the 2nd reserve-winner Federico Fellini lions’ quality and to our breeder-orientated Dante Weltino OLD, who managed to enter (by For Romance) in Westphalia and the service, we were able to increase our number the longlist for the Olympic Games in Rio premium stallion For Final (by For Romance) of coverings by 10 percent. -

Ocular Manifestations of Systemic Disease in the Horse
OCULAR MANIFESTATIONS OF SYSTEMIC DISEASE IN THE HORSE L. Chris Sanchez, DVM, PhD, DACVIM Caryn Plummer, DVM, DACVO University of Florida College of Veterinary Medicine, Gainesville, FL USA Overview Many systemic inflammatory diseases in horses have ocular signs, and many ophthalmic diseases (or their treatment) can have or result in systemic signs. Thus, it is important to look at the whole horse when considering treatment plans or prognoses. Though the proceedings are organized by specific manifestations, the talk will be entirely case-based. Ocular Manifestations of Systemic Disease Neonatal sepsis/SIRS The septic foal may seed bacteria to various organs, including the eye. The first sign of septic uveitis is usually a green hue to the iris and anterior chamber as fibrin seeps out of the uveal vasculature. Additional signs of uveitis follow and typically include miosis, globe hypotony (low IOP), aqueous flare, conjunctival and episcleral injection. Occasionally hypopyon and hyphema may develop. Ocular signs may be unilateral or bilateral. Systemic antimicrobial therapy and generalized support are critical to survival. The uveitis must be addressed with symptomatic anti- inflammatory therapy if intraocular scarring is to be avoided. As long as no corneal ulcer is present, topical medical treatment should consist of corticosteroids and atropine. If tolerable, systemic flunixin will benefit the eyes. Occasionally, fibrin will completely fill the anterior chamber and be slow to resorb. If it does not improve rapidly, intracameral tissue plasminogen activator (TPA) may be very helpful to hasten its dissolution. Rhodococcus equi Ocular manifestations of R. equi include uveitis and occasionally hyphema. Signs of uveitis typically include epihora, blepharospasm, photophobia, corneal edema, miosis, aqueous flare and significant accumulations of fibrin in the anterior chamber. -
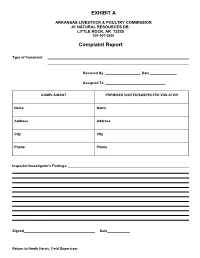
Complaint Report
EXHIBIT A ARKANSAS LIVESTOCK & POULTRY COMMISSION #1 NATURAL RESOURCES DR. LITTLE ROCK, AR 72205 501-907-2400 Complaint Report Type of Complaint Received By Date Assigned To COMPLAINANT PREMISES VISITED/SUSPECTED VIOLATOR Name Name Address Address City City Phone Phone Inspector/Investigator's Findings: Signed Date Return to Heath Harris, Field Supervisor DP-7/DP-46 SPECIAL MATERIALS & MARKETPLACE SAMPLE REPORT ARKANSAS STATE PLANT BOARD Pesticide Division #1 Natural Resources Drive Little Rock, Arkansas 72205 Insp. # Case # Lab # DATE: Sampled: Received: Reported: Sampled At Address GPS Coordinates: N W This block to be used for Marketplace Samples only Manufacturer Address City/State/Zip Brand Name: EPA Reg. #: EPA Est. #: Lot #: Container Type: # on Hand Wt./Size #Sampled Circle appropriate description: [Non-Slurry Liquid] [Slurry Liquid] [Dust] [Granular] [Other] Other Sample Soil Vegetation (describe) Description: (Place check in Water Clothing (describe) appropriate square) Use Dilution Other (describe) Formulation Dilution Rate as mixed Analysis Requested: (Use common pesticide name) Guarantee in Tank (if use dilution) Chain of Custody Date Received by (Received for Lab) Inspector Name Inspector (Print) Signature Check box if Dealer desires copy of completed analysis 9 ARKANSAS LIVESTOCK AND POULTRY COMMISSION #1 Natural Resources Drive Little Rock, Arkansas 72205 (501) 225-1598 REPORT ON FLEA MARKETS OR SALES CHECKED Poultry to be tested for pullorum typhoid are: exotic chickens, upland birds (chickens, pheasants, pea fowl, and backyard chickens). Must be identified with a leg band, wing band, or tattoo. Exemptions are those from a certified free NPIP flock or 90-day certificate test for pullorum typhoid. Water fowl need not test for pullorum typhoid unless they originate from out of state.