Download PDF (Inglês)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Case of Steroid Induced Mania
Case Report International Journal of Psychiatry A Case of Steroid Induced Mania 1* 1 Maryam M Alnasser , Yasser M Alanzi and Amena H * 2 Corresponding author Alhemyari Maryam M Alnasse, MBBS from University of Dammam, Saudi Arabia, E-mail: [email protected]. 1 MBBS from University of Dammam, Saudi Arabia. Submitted: 14 Dec 2016; Accepted: 26 Dec 2016; Published: 30 Dec 2016 2MBBS from King Faisal University, Saudi Arabia. Abstract Background: Steroids have been widely used and prescribed for a variety of systemic diseases. Although they prove to be highly effective, they have many physical and psychiatric adverse effects. The systemic side effects of these medications are well known and well studied, in contrast to the psychiatric adverse effects which its phenomenology needs to be the focus of more clinical studies. However, the incidence of diagnosable psychiatric disorders due to steroid therapy is reported to be 3-6%. Affective reactions such as depression, mania, and hypomania are the most common adverse effects, along with psychosis, anxiety and delirium. Aim: We describe a case of corticosteroid induced mania, its unusual clinical picture, its course and management. Case description: A 14-year-old female intermediate school student, with a recent diagnosis of Chron’s disease was brought to A&E department due to acute behavioral disturbance in form of confusion, visual hallucinations, psychomotor agitation, irritability, hyperactivity, talkativeness, lack of sleep, and physical aggression. Those symptoms have started few days following corticosteroid therapy which was Prednisolone 40mg PO OD. And she was diagnosed with steroid induced mania. Discussion: This case illustrates the need for more understanding of the phenomenology and diversity of corticosteroids induced psychiatric syndromes. -

Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the Use of Antiemetics Author(S): Dr Annette Edwards (Chai
Yorkshire Palliative Medicine Clinical Guidelines Group Guidelines on the use of Antiemetics Author(s): Dr Annette Edwards (Chair) and Deborah Royle on behalf of the Yorkshire Palliative Medicine Clinical Guidelines Group Overall objective : To provide guidance on the evidence for the use of antiemetics in specialist palliative care. Search Strategy: Search strategy: Medline, Embase and Cinahl databases were searched using the words nausea, vomit$, emesis, antiemetic and drug name. Review Date: March 2008 Competing interests: None declared Disclaimer: These guidelines are the property of the Yorkshire Palliative Medicine Clinical Guidelines Group. They are intended to be used by qualified, specialist palliative care professionals as an information resource. They should be used in the clinical context of each individual patient’s needs. The clinical guidelines group takes no responsibility for any consequences of any actions taken as a result of using these guidelines. Contact Details: Dr Annette Edwards, Macmillan Consultant in Palliative Medicine, Department of Palliative Medicine, Pinderfields General Hospital, Aberford Road, Wakefield, WF1 4DG Tel: 01924 212290 E-mail: [email protected] 1 Introduction: Nausea and vomiting are common symptoms in patients with advanced cancer. A careful history, examination and appropriate investigations may help to infer the pathophysiological mechanism involved. Where possible and clinically appropriate aetiological factors should be corrected. Antiemetics are chosen based on the likely mechanism and the neurotransmitters involved in the emetic pathway. However, a recent systematic review has highlighted that evidence for the management of nausea and vomiting in advanced cancer is sparse. (Glare 2004) The following drug and non-drug treatments were reviewed to assess the strength of evidence for their use as antiemetics with particular emphasis on their use in the palliative care population. -

The Effects of Antipsychotic Treatment on Metabolic Function: a Systematic Review and Network Meta-Analysis
The effects of antipsychotic treatment on metabolic function: a systematic review and network meta-analysis Toby Pillinger, Robert McCutcheon, Luke Vano, Katherine Beck, Guy Hindley, Atheeshaan Arumuham, Yuya Mizuno, Sridhar Natesan, Orestis Efthimiou, Andrea Cipriani, Oliver Howes ****PROTOCOL**** Review questions 1. What is the magnitude of metabolic dysregulation (defined as alterations in fasting glucose, total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and triglyceride levels) and alterations in body weight and body mass index associated with short-term (‘acute’) antipsychotic treatment in individuals with schizophrenia? 2. Does baseline physiology (e.g. body weight) and demographics (e.g. age) of patients predict magnitude of antipsychotic-associated metabolic dysregulation? 3. Are alterations in metabolic parameters over time associated with alterations in degree of psychopathology? 1 Searches We plan to search EMBASE, PsycINFO, and MEDLINE from inception using the following terms: 1 (Acepromazine or Acetophenazine or Amisulpride or Aripiprazole or Asenapine or Benperidol or Blonanserin or Bromperidol or Butaperazine or Carpipramine or Chlorproethazine or Chlorpromazine or Chlorprothixene or Clocapramine or Clopenthixol or Clopentixol or Clothiapine or Clotiapine or Clozapine or Cyamemazine or Cyamepromazine or Dixyrazine or Droperidol or Fluanisone or Flupehenazine or Flupenthixol or Flupentixol or Fluphenazine or Fluspirilen or Fluspirilene or Haloperidol or Iloperidone -

Management of Major Depressive Disorder Clinical Practice Guidelines May 2014
Federal Bureau of Prisons Management of Major Depressive Disorder Clinical Practice Guidelines May 2014 Table of Contents 1. Purpose ............................................................................................................................................. 1 2. Introduction ...................................................................................................................................... 1 Natural History ................................................................................................................................. 2 Special Considerations ...................................................................................................................... 2 3. Screening ........................................................................................................................................... 3 Screening Questions .......................................................................................................................... 3 Further Screening Methods................................................................................................................ 4 4. Diagnosis ........................................................................................................................................... 4 Depression: Three Levels of Severity ............................................................................................... 4 Clinical Interview and Documentation of Risk Assessment............................................................... -

Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com
Hallucinogens And Dissociative Drug Use And Addiction Introduction Hallucinogens are a diverse group of drugs that cause alterations in perception, thought, or mood. This heterogeneous group has compounds with different chemical structures, different mechanisms of action, and different adverse effects. Despite their description, most hallucinogens do not consistently cause hallucinations. The drugs are more likely to cause changes in mood or in thought than actual hallucinations. Hallucinogenic substances that form naturally have been used worldwide for millennia to induce altered states for religious or spiritual purposes. While these practices still exist, the more common use of hallucinogens today involves the recreational use of synthetic hallucinogens. Hallucinogen And Dissociative Drug Toxicity Hallucinogens comprise a collection of compounds that are used to induce hallucinations or alterations of consciousness. Hallucinogens are drugs that cause alteration of visual, auditory, or tactile perceptions; they are also referred to as a class of drugs that cause alteration of thought and emotion. Hallucinogens disrupt a person’s ability to think and communicate effectively. Hallucinations are defined as false sensations that have no basis in reality: The sensory experience is not actually there. The term “hallucinogen” is slightly misleading because hallucinogens do not consistently cause hallucinations. 1 ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com How hallucinogens cause alterations in a person’s sensory experience is not entirely understood. Hallucinogens work, at least in part, by disrupting communication between neurotransmitter systems throughout the body including those that regulate sleep, hunger, sexual behavior and muscle control. Patients under the influence of hallucinogens may show a wide range of unusual and often sudden, volatile behaviors with the potential to rapidly fluctuate from a relaxed, euphoric state to one of extreme agitation and aggression. -

The ICD-10 Classification of Mental and Behavioural Disorders : Clinical Descriptions and Diagnostic Guidelines
ICD-10 ThelCD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines | World Health Organization I Geneva I 1992 Reprinted 1993, 1994, 1995, 1998, 2000, 2002, 2004 WHO Library Cataloguing in Publication Data The ICD-10 classification of mental and behavioural disorders : clinical descriptions and diagnostic guidelines. 1.Mental disorders — classification 2.Mental disorders — diagnosis ISBN 92 4 154422 8 (NLM Classification: WM 15) © World Health Organization 1992 All rights reserved. Publications of the World Health Organization can be obtained from Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications — whether for sale or for noncommercial distribution — should be addressed to Publications, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Emea/666243/2009
European Medicines Agency London, 29 October 2009 EMEA/666243/2009 ISSUE NUMBER: 0910 MONTHLY REPORT PHARMACOVIGILANCE WORKING PARTY (PHVWP) OCTOBER 2009 PLENARY MEETING The CHMP Pharmacovigilance Working Party (PhVWP) held its October 2009 plenary meeting on 19-21 October 2009. PhVWP DISCUSSIONS ON SAFETY CONCERNS Below is a summary of the discussions regarding non-centrally authorised medicinal products in accordance with the PhVWP publication policy (see under http://www.emea.europa.eu/htms/human/phv/reports.htm). Positions agreed by the PhVWP for non- centrally authorised products are recommendations to Member States. For safety updates concerning centrally authorised products and products subject to ongoing CHMP procedures, readers are referred to the CHMP Monthly Report (see under http://www.emea.europa.eu/pressoffice/presshome.htm). The PhVWP provides advice on these products to the Committee of Medicinal Products for Human Use (CHMP) upon its request. Antipsychotics - risk of venous thromboembolism (VTE) Identify risk factors for VTE for preventive action before and during treatment with antipsychotics The PhVWP completed their review on the risk of VTE of antipsychotics1. The review was triggered by and based on data from the UK spontaneous adverse drug reactions reporting system and the published literature. The PhVWP carefully considered the data, including the limitations of both information sources, such as the lack of randomised controlled trial data, the heterogeneity of published studies and the potential confounding factors such as sedation and weight gain, commonly present in antipsychotic users. The PhVWP concluded that an association between VTE and antipsychotics cannot be excluded. Distinguishing different risk levels between the various active substances was not possible. -

The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research
The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic criteria for research World Health Organization Geneva The World Health Organization is a specialized agency of the United Nations with primary responsibility for international health matters and public health. Through this organization, which was created in 1948, the health professions of some 180 countries exchange their knowledge and experience with the aim of making possible the attainment by all citizens of the world by the year 2000 of a level of health that will permit them to lead a socially and economically productive life. By means of direct technical cooperation with its Member States, and by stimulating such cooperation among them, WHO promotes the development of comprehensive health services, the prevention and control of diseases, the improvement of environmental conditions, the development of human resources for health, the coordination and development of biomedical and health services research, and the planning and implementation of health programmes. These broad fields of endeavour encompass a wide variety of activities, such as developing systems of primary health care that reach the whole population of Member countries; promoting the health of mothers and children; combating malnutrition; controlling malaria and other communicable diseases including tuberculosis and leprosy; coordinating the global strategy for the prevention and control of AIDS; having achieved the eradication of smallpox, promoting mass immunization against a number of other -
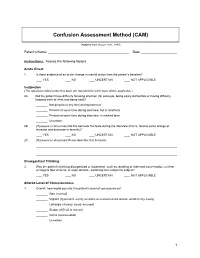
Confusion Assessment Method (CAM)
Confusion Assessment Method (CAM) (Adapted from Inouye et al., 1990) Patient’s Name: Date: Instructions: Assess the following factors. Acute Onset 1. Is there evidence of an acute change in mental status from the patient’s baseline? YES NO UNCERTAIN NOT APPLICABLE Inattention (The questions listed under this topic are repeated for each topic where applicable.) 2A. Did the patient have difficulty focusing attention (for example, being easily distractible or having difficulty keeping track of what was being said)? Not present at any time during interview Present at some time during interview, but in mild form Present at some time during interview, in marked form Uncertain 2B. (If present or abnormal) Did this behavior fluctuate during the interview (that is, tend to come and go or increase and decrease in severity)? YES NO UNCERTAIN NOT APPLICABLE 2C. (If present or abnormal) Please describe this behavior. Disorganized Thinking 3. Was the patient’s thinking disorganized or incoherent, such as rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable, switching from subject to subject? YES NO UNCERTAIN NOT APPLICABLE Altered Level of Consciousness 4. Overall, how would you rate this patient’s level of consciousness? Alert (normal) Vigilant (hyperalert, overly sensitive to environmental stimuli, startled very easily) Lethargic (drowsy, easily aroused) Stupor (difficult to arouse) Coma (unarousable) Uncertain 1 Disorientation 5. Was the patient disoriented at any time during the interview, such as thinking that he or she was somewhere other than the hospital, using the wrong bed, or misjudging the time of day? YES NO UNCERTAIN NOT APPLICABLE Memory Impairment 6. -

Perphenazine-151548-PI.Pdf
PRESCRIBING INFORMATION PERPHENAZINE Perphenazine Tablets USP 2 mg , 4 mg, 8mg, and 16 mg Antipsychotic/Antiemetic AA Pharma Inc. DATE OF REVISION: April 12, 2012 1165 Creditsone Road, Unit #1 Vaughan, Ontario L4K 4N7 Control Number: 151548 PRESCRIBING INFORMATION PERPHENAZINE Perphenazine Tablets USP 2 mg, 4 mg, 8 mg and 16 mg THERAPEUTIC CLASSIFICATION Antipsychotic/Antiemetic ACTIONS AND CLINICAL PHARMACOLOGY Perphenazine is a piperazine phenothiazine derivative with antipsychotic, antiemetic and weak sedative activity. Perphenazine has actions similar to those of other phenothiazine derivatives but appears to be less sedating and to have a weak propensity for causing hypotension or potentiating the effects of CNS depressants and anesthetics. However, it produces a high incidence of extrapyramidal reactions. Perphenazine is well absorbed from the gastrointestinal tract. Onset of action following oral administration is 30 to 40 minutes. Duration of action is 3 to 4 hours. Perphenazine distributes to most body tissues with high concentrations being distributed into liver and spleen. Perphenazine enters the enterohepatic circulation and is excreted chiefly in the feces. INDICATIONS AND CLINICAL USE Perphenazine is indicated in the management of manifestations of psychotic disorders. It is also effective in controlling nausea and vomiting due to stimulation of the chemoreceptor trigger zone. 1 Perphenazine has not been shown effective for the management of behavioral complications in patients with mental retardation. CONTRAINDICATIONS Should not be administered in the presence of circulatory collapse, altered states of consciousness or comatose states, particularly when these are due to intoxication with central depressant drugs (alcohol, hypnotics, narcotics). It is contraindicated in severely depressed patients, in the presence of blood dyscrasias, liver disease, renal insufficiency, pheochromocytoma, or in patients with severe cardiovascular disorders or a history of hypersensitivity to phenothiazine derivatives. -

Lamotrigine As a Treatment of Agitation in Dementia F
Lamotrigine as a treatment of agitation in Dementia F. Godinho1, A. Valverde2. 1Hospital Espirito Santo de Évora, Department of Psychiatry and Mental Health, Évora, Portugal. 2Hospital Professor Doutor Fernando da Fonseca, Neurology Service, Amadora, Portugal. Background: • Psychomotor agitation is common in patients with dementia but there are no well-established or evidenced-based effective treatments. • Non-pharmacological interventions remain the mainstay of treatment but are not always feasible or sufficient. • Antipsychotic are the most commonly used drugs but concerns regarding tolerability limit their use. • Anticonvulsants are receiving growing attention due to their better safety profile. Objective: Methods: We report a case of a patient with dementia and behavioral disturbance Retrospective review of the clinical chart and literature review on the treated with lamotrigine, and make a brief review of the literature of topic. anticonvulsants use in the treatment of agitation and aggression in dementia. RESULTS Clinical case • A 69 years-old woman with behavioral variant Frontotemporal Dementia, severe stage, totally dependent on activities of daily living and with severe speech difficulties, developed progressive aggressive behavior. • In the following 6 months, quetiapine until 200mg/daily and then risperidone until 1mg/daily was tried, with no success. • Lamotrigine was then introduced and titrated until 100mg/daily. • Since this dosage and in the 2 next consultations, no more aggressive behavior were observed Literature Review -

A Retrospective Review of the Use and Safety of Droperidol in a Large, High-Risk, Inner-City Emergency Department Patient Populaton
1402 Chase, Biros · DROPERIDOL USE IN THE ED A Retrospective Review of the Use and Safety of Droperidol in a Large, High-risk, Inner-city Emergency Department Patient Populaton Peter B. Chase, MD, PhD, Michelle H. Biros, MD, MS Abstract Droperidol (DROP) is used in the emergency department teria for high risk. There were 622 pts with head trauma (ED) for sedation, analgesia, and its antiemetic effect. Its (401 with alcohol use), including 47 with computed to- ED safety pro®le has not yet been reported in patients mography (CT) scans positive for brain injury, 64 with (pts). Objectives: To document the use of DROP in high- cocaine use, and 197 with recent or remote seizures (137 risk pts (those with head injury, alcohol or cocaine intox- with alcohol use). Minor AEs such as transient hypoten- ication, and/or remote or recent seizures), and to deter- sion occurred in 96 pts after DROP (73 with alcohol use); mine the number of serious and minor adverse events 20 received intravenous ¯uids, while an additonal 28 pts (AEs)Ðseizures, hypotension, extrapyramidal side ef- (8 with alcohol use) received rescue medications for fects (EPSEs)Ðafter DROP. Methods: The ED database EPSEs. Six possible serious AEs occurred in pts with se- (EmSTAT) was queried to determine who received intra- rious comorbidities; 2 cases of respiratory depression, 3 muscular or intravenous DROP in the ED in 1998; further post-DROP seizures, and 1 cardiac arrest (resuscitated) 11 chart review was done if the patient was considered high hours after DROP in a cocaine-intoxicated pt (normal QT risk for or had experienced an AE.