Vitamin B12 Deficiency : Management of During Pregnancy This Document Should Be Read in Conjunction with the Disclaimer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recent Insights Into the Role of Vitamin B12 and Vitamin D Upon Cardiovascular Mortality: a Systematic Review
Acta Scientific Pharmaceutical Sciences (ISSN: 2581-5423) Volume 2 Issue 12 December 2018 Review Article Recent Insights into the Role of Vitamin B12 and Vitamin D upon Cardiovascular Mortality: A Systematic Review Raja Chakraverty1 and Pranabesh Chakraborty2* 1Assistant Professor, Bengal School of Technology (A College of Pharmacy), Sugandha, Hooghly, West Bengal, India 2Director (Academic), Bengal School of Technology (A College of Pharmacy),Sugandha, Hooghly, West Bengal, India *Corresponding Author: Pranabesh Chakraborty, Director (Academic), Bengal School of Technology (A College of Pharmacy), Sugandha, Hooghly, West Bengal, India. Received: October 17, 2018; Published: November 22, 2018 Abstract since the pathogenesis of several chronic diseases have been attributed to low concentrations of this vitamin. The present study Vitamin B12 and Vitamin D insufficiency has been observed worldwide at all stages of life. It is a major public health problem, throws light on the causal association of Vitamin B12 to cardiovascular disorders. Several evidences suggested that vitamin D has an effect in cardiovascular diseases thereby reducing the risk. It may happen in case of gene regulation and gene expression the vitamin D receptors in various cells helps in regulation of blood pressure (through renin-angiotensin system), and henceforth modulating the cell growth and proliferation which includes vascular smooth muscle cells and cardiomyocytes functioning. The present review article is based on identifying correct mechanisms and relationships between Vitamin D and such diseases that could be important in future understanding in patient and healthcare policies. There is some reported literature about the causative association between disease (CAD). Numerous retrospective and prospective studies have revealed a consistent, independent relationship of mild hyper- Vitamin B12 deficiency and homocysteinemia, or its role in the development of atherosclerosis and other groups of Coronary artery homocysteinemia with cardiovascular disease and all-cause mortality. -

Family Practice
THE JOURNAL OF FAMILY PRACTICE Emmanuel Andrès, MD, B12 deficiency: A look beyond Laure Federici, MD, Stéphan Affenberger, MD pernicious anemia Department of Internal Medicine, Diabetes and Metabolic Diseases, Food-B12 malabsorption—not pernicious anemia—is the Hôpitaux Universitaires de Strasbourg, leading cause of B12 malabsorption. It’s also very subtle Strasbourg, France emmanuel.andres @chru-strasbourg.fr Practice recommendations such as its link to Helicobacter pylori • Mild, preclinical B deficiency infection and long-term antacid and bi- Josep Vidal-Alaball, MD 12 Department of General is associated with food-B12 guanide use. It also requires that you Practice, Cardiff University, malabsorption more often than consider not only a patient’s serum B12 United Kingdom with pernicious anemia. (C) ® Dowdenlevels, but his Health homocysteine Media and meth - Noureddine Henoun ylmalonic acid levels, since they are con- Loukili, PhD • The classic treatment for B 12 Department of Hygiene and deficiency—particularly when the sidered more sensitive indicators of co- 6 Fight against Nosocomial cause is not a dietaryCopyright deficiency—isFor personalbalamin deficiency. use Keyingonly in on these Infections, Hôpital Calmette, 100 to 1000 mcg per month of indicators early will ensure prompt treat- CHRU de Lille, Lille, France cyanocobalamin, IM. (B) ment, which typically includes intramus- cular injections of the vitamin, but which Jacques Zimmer, MD, PhD • Oral crystalline cyanocobalamin could revolve around a more convenient Laboratoire is an effective treatment for food- d’Immunogénétique- option: oral B12. Allergologie, Centre de B12 malabsorption, though it’s Recherche Public de la Santé effectiveness in the long term has (CRP-Santé) de Luxembourg, not been demonstrated. -

Nutrition 102 – Class 3
Nutrition 102 – Class 3 Angel Woolever, RD, CD 1 Nutrition 102 “Introduction to Human Nutrition” second edition Edited by Michael J. Gibney, Susan A. Lanham-New, Aedin Cassidy, and Hester H. Vorster May be purchased online but is not required for the class. 2 Technical Difficulties Contact: Erin Deichman 574.753.1706 [email protected] 3 Questions You may raise your hand and type your question. All questions will be answered at the end of the webinar to save time. 4 Review from Last Week Vitamins E, K, and C What it is Source Function Requirement Absorption Deficiency Toxicity Non-essential compounds Bioflavonoids: Carnitine, Choline, Inositol, Taurine, and Ubiquinone Phytoceuticals 5 Priorities for Today’s Session B Vitamins What they are Source Function Requirement Absorption Deficiency Toxicity 6 7 What Is Vitamin B1 First B Vitamin to be discovered 8 Vitamin B1 Sources Pork – rich source Potatoes Whole-grain cereals Meat Fish 9 Functions of Vitamin B1 Converts carbohydrates into glucose for energy metabolism Strengthens immune system Improves body’s ability to withstand stressful conditions 10 Thiamine Requirements Groups: RDA (mg/day): Infants 0.4 Children 0.7-1.2 Males 1.5 Females 1 Pregnancy 2 Lactation 2 11 Thiamine Absorption Absorbed in the duodenum and proximal jejunum Alcoholics are especially susceptible to thiamine deficiency Excreted in urine, diuresis, and sweat Little storage of thiamine in the body 12 Barriers to Thiamine Absorption Lost into cooking water Unstable to light Exposure to sunlight Destroyed -
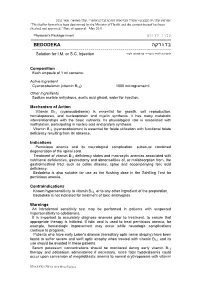
בדודקה BEDODEKA ------להזרקה לתוך השריר או מתחת לעור Solution for I.M
"פורמט עלון זה נקבע ע"י משרד הבריאות ותוכנו נבדק ואושר". עלון מאושר: מאי 2011. “This leaflet format has been determined by the Ministry of Health and the content thereof has been checked and approved.” Date of approval: May 2011. עלון לרופא Physician's Package Insert ========================================================================== בדודקה BEDODEKA --------------------------------------------------------------------- להזרקה לתוך השריר או מתחת לעור Solution for I.M. or S.C. Injection Composition Each ampoule of 1 ml contains: Active Ingredient Cyanocobalamin (vitamin B12) 1000 micrograms/ml Other Ingredients Sodium acetate anhydrous, acetic acid glacial, water for injection. Mechanism of Action Vitamin B12 (cyanocobalamin) is essential for growth, cell reproduction, hematopoiesis, and nucleoprotein and myelin synthesis. It has many metabolic interrelationships with the basic nutrients. Its physiological role is associated with methylation, participating in nucleic acid and protein synthesis. Vitamin B12 (cyanocobalamin) is essential for folate utilization with functional folate deficiency resulting from its absence. Indications Pernicious anemia and its neurological complication, subacute combined degeneration of the spinal cord. Treatment of vitamin B12 deficiency states and macrocytic anemias associated with nutritional deficiencies, gastrectomy and abnormalities of, or malabsorption from, the gastrointestinal tract such as celiac disease, sprue and accompanying folic acid deficiency. Bedodeka is also suitable for use as the flushing dose in the Schilling Test for pernicious anemia. Contraindications Known hypersensitivity to vitamin B12, or to any other ingredient of the preparation. Bedodeka is not indicated for treatment of toxic amblyopias. Warnings An intradermal sensitivity test may be performed in patients with suspected hypersensitivity to cobalamins. It is important to accurately diagnose anemias prior to treatment, to ensure that appropriate therapy is initiated. -

VI.2 Elements for a Public Summary VI.2.1 Overview of Disease Epidemiology Vitamin B12 Deficiency Can Have a Number of Possible
VI.2 Elements for a public summary VI.2.1 Overview of disease epidemiology Vitamin B12 deficiency can have a number of possible causes. Typically it occurs in people whose digestive systems do not adequately absorb the vitamin from the foods they eat. This can be caused by: Pernicious anemia, a condition in where there is a lack of a protein called intrinsic factor. The protein, which is made in the stomach, is necessary for vitamin B12 absorption. Other causes can be gastritis, surgery in which part of the stomach and/or small intestine is removed or conditions affecting the small intestine. Vitamin B12 deficiency can also occur in pregnancy and with long- term use of acid-reducing drugs. VI.2.2 Summary of treatment benefits A deficiency of vitamin B12 (cobalamin) is manifested by fatigue, weakness, mood fluctuations, memory loss, limb weakness, difficulty walking, tingling, and paralysis. Drug treatment involves the administration of vitamin B12 by injection. If the deficiency of vitamin B12 (cobalamin) depends on the underlying disease being resolved, the vitamin supplementation continues until normal levels of vitamin B12 are achieved. If the deficiency state cannot be resolved (e.g. inadequate secretion of intrinsic factor, genetic abnormalities related to the site absorption, etc.) therapy should be continued for life. VI.2.3 Unknowns relating to treatment benefits None. VI.2.4 Summary of safety concerns Risk What is known Preventability Damage to the optic nerve Optic nerve atrophy/blindness The product should be used (atrophy)/blindness in is a risk associated with with caution. patients with Leber´s disease treatment with (a disease that affects the hydroxocobalamin in patients optic nerve and often causes with Leber´s disease. -

Vitamin B12 Deficiency ROBERT C
Vitamin B12 Deficiency ROBERT C. OH, CPT, MC, USA, U.S. Army Health Clinic, Darmstadt, Germany DAVID L. BROWN, MAJ, MC, USA, Madigan Army Medical Center, Fort Lewis, Washington Vitamin B12 (cobalamin) deficiency is a common cause of macrocytic anemia and has been implicated in a spectrum of neuropsychiatric disorders. The role of B12 deficiency O A patient informa- in hyperhomocysteinemia and the promotion of atherosclerosis is only now being tion handout on vita- min B12 deficiency, explored. Diagnosis of vitamin B12 deficiency is typically based on measurement of written by the authors serum vitamin B12 levels; however, about 50 percent of patients with subclinical dis- of this article, is pro- ease have normal B12 levels. A more sensitive method of screening for vitamin B12 defi- vided on page 993. ciency is measurement of serum methylmalonic acid and homocysteine levels, which are increased early in vitamin B12 deficiency. Use of the Schilling test for detection of pernicious anemia has been supplanted for the most part by serologic testing for pari- etal cell and intrinsic factor antibodies. Contrary to prevailing medical practice, studies show that supplementation with oral vitamin B12 is a safe and effective treatment for the B12 deficiency state. Even when intrinsic factor is not present to aid in the absorp- tion of vitamin B12 (pernicious anemia) or in other diseases that affect the usual absorption sites in the terminal ileum, oral therapy remains effective. (Am Fam Physi- cian 2003;67:979-86,993-4. Copyright© 2003 American Academy of Family Physicians.) itamin B12 (cobalamin) plays manifestations (Table 1).It is a common cause an important role in DNA of macrocytic (megaloblastic) anemia and, in synthesis and neurologic func- advanced cases, pancytopenia. -

Nutritional Dermatoses in the Hospitalized Patient
HOSPITAL CONSULT IN PARTNERSHIP WITH THE SOCIETY FOR DERMATOLOGY HOSPITALISTS Nutritional Dermatoses in the Hospitalized Patient Melissa Hoffman, MS; Robert G. Micheletti, MD; Bridget E. Shields, MD Nutritional deficiencies may arise from inadequate nutrient intake, abnormal nutrient absorption, or improper nutrient PRACTICE POINTS utilization.4 Unfortunately, no standardized algorithm for • Nutritional deficiencies are common in hospitalized screening and diagnosing patients with malnutrition exists, patients and often go unrecognized. making early physical examination findings of utmost • Awareness of the risk factors predisposing patients importance. Herein, we present a review of acquired nutri- to nutritional deficiencies and the cutaneous manifes- tional deficiency dermatoses in the inpatient setting. tations associated with undernutrition can promote copy early diagnosis. Protein-Energy Malnutrition • When investigating cutaneous findings, undernutri- tion should be considered in patients with chronic Protein-energy malnutrition (PEM) refers to a set of infections, malabsorptive states, psychiatric illness, related disorders that include marasmus, kwashiorkor and strict dietary practices, as well as in those using (KW), and marasmic KW. These conditions frequently are certain medications. seen in developing countries but also have been reported 5 • Prompt nutritional supplementation can prevent patient in developed nations. Marasmus occurs from a chronic morbidity and mortality and reverse skin disease. deficiencynot of protein and calories. Decreased insulin pro- duction and unopposed catabolism result in sarcopenia and loss of bone and subcutaneous fat.6 Affected patients include children who are less than 60% ideal body weight Cutaneous disease may be the first manifestation of an underlying nutri- 7 tional deficiency, highlighting the importance of early recognition by der- (IBW) without edema or hypoproteinemia. -

Prevalence and Indicators of Vitamin B12 Insufficiency Among Young
International Journal of Environmental Research and Public Health Article Prevalence and Indicators of Vitamin B12 Insufficiency among Young Women of Childbearing Age Sara Al-Musharaf 1,2,* , Philip G. McTernan 3,*, Syed Danish Hussain 2, Khalid Abdullah Aleisa 4 , Abdullah M. Alnaami 2, Kaiser Wani 2 , Ponnusamy Saravanan 5,6 and Nasser Al-Daghri 2 1 Department of Community Health Sciences, College of Applied Medical Sciences, King Saud University, Riyadh 11451, Saudi Arabia 2 Chair for Biomarkers of Chronic Diseases, Riyadh Biochemistry Department, College of Science, King Saud University, Riyadh 11451, Saudi Arabia; [email protected] (S.D.H.); [email protected] (A.M.A.); [email protected] (K.W.); [email protected] (N.A.-D.) 3 Department of Biosciences, School of Science and Technology, Nottingham Trent University, Nottingham NG1 8NS, UK 4 College of Medicine, King Saud University, Riyadh 11451, Saudi Arabia; [email protected] 5 Population, Evidence & Technologies, Division of Health Sciences, Warwick Medical School, University of Warwick, Coventry CV2 2DX, UK; [email protected] 6 Academic Department of Diabetes, Endocrinology & Metabolism, George Eliot Hospital, Nuneaton CV10 7DJ, UK * Correspondence: [email protected] (S.A.-M.); [email protected] (P.G.M.); Tel.: +44-(0)115-848-3477 (S.A.-M.); +966-55-424-3033 (P.G.M.) Abstract: Vitamin B12 insufficiency is a global health issue among women of childbearing age, yet few studies have investigated its prevalence and risk factors among healthy Middle Eastern populations. This cross-sectional study included 346 Saudi women aged 19–30 years and enrolled at King Saud University, Riyadh, Saudi Arabia. -

Serum and Red Cell Folates, and Serum Vitamin B12 in Protein Calorie Malnutrition
Arch Dis Child: first published as 10.1136/adc.48.5.366 on 1 May 1973. Downloaded from Archives of Disease in Childhood, 1973, 48, 366. Serum and red cell folates, and serum vitamin B12 in protein calorie malnutrition M. KHALIL, A. TANIOS, M. MOGHAZY, M. K. AREF, S. MAHMOUD, and M. EL LOZY From the Departments of Paediatrics, Clinical Pathology, and Physiology, Faculty of Medicine, University of Alexandria, Alexandria, Egypt Khalil, M., Tanios, A., Moghazy, M., Aref, M. K., Mahmoud, S., and el Lozy, M. (1973). Archives of Disease in Childhood, 48, 366. Serum and red cell folates, and serum vitamin B12 in protein calorie malnutrition. In 22 cases of kwashiorkor, 19 cases of marasmus, and 16 normal controls, red cell folate, serum folate, and serum vitamin B1, were estimated, and the bone marrow and peripheral blood examined. Erythrocyte folate deficiency was shown in 9 cases of kwashiorkor and 7 cases of marasmus. Serum folate deficiency was present in 14 cases of kwashi- orkor and 7 cases of marasmus. Megaloblastosis was found in 45% of cases of kwashiorkor and 37% of cases of marasmus. Megaloblastosis and macrocytosis correlated more with erythrocyte than with serum folate deficiency. Serum vitamin B1, levels in children with kwashiorkor or marasmus did not differ from those of normal controls. The role of folate deficiency in the pathogenesis of megaloblastosis in protein calorie malnutrition was confirmed. copyright. A hypochromic anaemia of iron deficiency is a Material and methods salient finding in patients with protein calorie The study was carried out on 22 infants (12 males and malnutrition (Khalil, Awwad, and Hafez, 1968). -

WHO Technical Consultation on Folate and Vitamin B12 Deficiencies
Conclusions of a WHO Technical Consultation on folate and vitamin B12 deficiencies All participants in the Consultation Key words: Folate, vitamin B12 The consultation agreed on conclusions in four areas: » Indicators for assessing the prevalence of folate and Preamble vitamin B12 deficiencies » Health consequences of folate and vitamin B12 defi- Folate and vitamin B12 deficiencies occur primarily as ciencies a result of insufficient dietary intake or, especially in » Approaches to monitoring the effectiveness of inter- the case of vitamin B12 deficiency in the elderly, poor ventions absorption. Folate is present in high concentrations » Strategies to improve intakes of folate and vitamin B12 in legumes, leafy green vegetables, and some fruits, so lower intakes can be expected where the staple diet consists of unfortified wheat, maize, or rice, and when Indicators for assessing and monitoring the intake of legumes and folate-rich vegetables and vitamin status fruits is low. This situation can occur in both wealthy and poorer countries. Animal-source foods are the only Prevalence of deficiencies natural source of vitamin B12, so deficiency is prevalent when intake of these foods is low due to their high The recent review by WHO showed that the majority cost, lack of availability, or cultural or religious beliefs. of data on the prevalence of folate and vitamin B12 Deficiency is certainly more prevalent in strict vegetar- deficiencies are derived from relatively small, local ians, but lacto-ovo vegetarians are also at higher risk surveys, but these and national survey data from a for inadequate intakes. If the mother is folate-depleted few countries suggest that deficiencies of both of these during lactation, breastmilk concentrations of the vitamins may be a public health problem that could vitamin are maintained while the mother becomes affect many millions of people throughout the world. -

Folate Rescues Vitamin B12 Depletion-Induced Inhibition of Nuclear Thymidylate Biosynthesis and Genome Instability
PNAS PLUS Folate rescues vitamin B12 depletion-induced inhibition of nuclear thymidylate biosynthesis and genome instability Ashley M. Palmera, Elena Kamyninaa, Martha S. Fielda, and Patrick J. Stovera,b,1 aDivision of Nutritional Sciences, Cornell University, Ithaca, NY 14853; and bGraduate Field of Biochemistry, Molecular, and Cell Biology, Cornell University, Ithaca, NY 14853 Contributed by Patrick J. Stover, April 5, 2017 (sent for review November 30, 2016; reviewed by Lawrence Brody and Ralph Green) Clinical vitamin B12 deficiency can result in megaloblastic ane- group from 5-methyltetrahydrofolate (5-methylTHF) is transferred mia, which results from the inhibition of DNA synthesis by trap- to cobalamin, thereby creating methylcobalamin and releasing ping folate cofactors in the form of 5-methyltetrahydrofolate THF. In the second step, the methyl group from methylcobalamin (5-methylTHF) and subsequent inhibition of de novo thymidylate is transferred to homocysteine for methionine synthesis (4). Con- (dTMP) biosynthesis. In the cytosol, vitamin B12 functions in the sequences of reduced MTR activity include elevated homocysteine remethylation of homocysteine to methionine, which regenerates in tissue and plasma, a biomarker associated with adverse health THF from 5-methylTHF. In the nucleus, THF is required for de novo outcomes, including risk for neural tube defects (NTDs) (9) and dTMP biosynthesis, but it is not understood how 5-methylTHF ac- impaired methylation status, as methionine is required for the cumulation in the cytosol impairs nuclear dTMP biosynthesis. The synthesis of S-adenosylmethionine (AdoMet), the universal impact of vitamin B12 depletion on nuclear de novo dTMP biosyn- methyl donor required for over 100 cellular methylation reac- thesis was investigated in methionine synthase-null human fibro- tions (10). -

How Do We Evaluate a Marginally Low B12 Level?
From the CLINIcAL InQUiRiES Family Physicians Inquiries Network David D. Cravens, MD, MSPH, CMD How do we evaluate Department of Family and Community Medicine, University of Missouri–Columbia School a marginally low B12 level? of Medicine Joan Nashelsky, MLS EVIDENCE - BASED ANSWER WISE—Women in Science and Engineering, University of Iowa The best way to evaluate a low-normal 1 or 2 mg of oral vitamin B12 a day B12 level is to check serum methylmalonic if levels are marginally low and either acid and homocysteine levels1 (strength of methylmalonic acid or both methylmalonic recommendation [SOR]: B, based acid and homocysteine are elevated on consistent level 2 or 3 studies). Give (SOR: A). CLINICAL ®COMMENTARYDowden Health Media When faced with low-normal serum B12, Once deficiency is confirmed, search for Copyrighteither further evaluation a cause. Since 1000 mcg of oral B treats For personal use only 12 or empiric treatment is warranted nearly all causes of B12 deficiency (includ- With the advent of methylmalonic acid, ing pernicious anemia and deficiency from homocysteine testing, and the proven gastric bypass surgery), empiric treatment efficacy of oral 12B , medicine has come a is a reasonable alternative as long as long way from Shilling tests and monthly serum B12 and symptoms are monitored intramuscular shots in the diagnosis and for therapeutic response. Bottom line: management of B12 deficiency. “Normal” since early detection and treatment could serum B12 may not accurately reflect true potentially prevent permanent neurologic tissue B12 stores. Therefore, if serum B12 is sequelae, when faced with a low-normal borderline low, I routinely get methylma- serum B12, it should not be dismissed as lonic acid and homocysteine for patients “normal”—either further evaluation or in whom I need to “prove” deficiency (for empiric treatment is warranted.