Complete Trisomy of Chromosome 9: Karyotyping and Morphological Alterations in Newborn
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Causes.Pdf
1 September 2015 Genetic causes of childhood apraxia of speech: Case‐based introduction to DNA, inheritance, and clinical management Beate Peter, Ph.D., CCC‐SLP Assistant Professor Dpt. of Speech & Hearing Science Arizona State University Adjunct Assistant Professor AG Dpt. of Communication Sciences & Disorders ATAGCT Saint Louis University T TAGCT Affiliate Assistant Professor Dpt. of Speech & Hearing Sciences University of Washington 1 Disclosure Statement Disclosure Statement Dr. Peter is co‐editor of a textbook on speech development and disorders (B. Peter & A. MacLeod, Eds., 2013), for which she may receive royalty payments. If she shares information about her ongoing research study, this may result in referrals of potential research participants. She has no financial interest or related personal interest of bias in any organization whose products or services are described, reviewed, evaluated or compared in the presentation. 2 Agenda Topic Concepts Why we should care about genetics. Case 1: A sporadic case of CAS who is missing a • Cell, nucleus, chromosomes, genes gene. Introduction to the language of genetics • From genes to proteins • CAS can result when a piece of DNA is deleted or duplicated Case 2: A multigenerational family with CAS • How the FOXP2 gene was discovered and why research in genetics of speech and language disorders is challenging • Pathways from genes to proteins to brain/muscle to speech disorder Case 3: One family's quest for answers • Interprofessional teams, genetic counselors, medical geneticists, research institutes • Early signs of CAS, parent education, early intervention • What about genetic testing? Q&A 3 “Genetic Causes of CAS: Case-Based Introduction to DNA, Inheritance and Clinical Management,” Presented by: Beate Peter, PhD, CCC-SLP, September 29, 2015, Sponsored by: CASANA 2 Why should you care about genetics? 4 If you are a parent of a child with childhood apraxia of speech … 5 When she was in preschool, He doesn’t have any friends. -
Inside This Issue
Winter 2014 No. 77 Inside this issue Group News | Fundraising | Members’ Letters | One Family Living with Two Different Chromosome Disorders | Bristol Conference 2014 | Unique Leaflets | Christmas Card Order Form Sophie, Unique’s Chair of Trustees Dear Members, In the past month a few things have reminded me of why it is so important to make connections through Unique but also to draw support from other parents around us. I’ve just returned from Unique’s most recent family conference in Bristol where 150 of us parents and carers had a lovely time in workshops, meals and activities, chatting and watching our children milling around together like one big family since – although we had never met before – we have shared so many experiences in common. However in contrast I have also just met a new mum who has just moved to my area from far away with two toddlers, one with a rare joys of the internet, it is becoming easier to meet others with similar, chromosome disorder, who is starting from scratch with no even very rare, chromosome disorders around the world and to find professional, medical or social support. She reminds me of how yourself talking to them in the middle of the night about some lonely I felt when Max was newly diagnosed, when I knew no one interesting things our children share in common (obsession with with a disabled child let alone anyone with a rare chromosome catalogues, anyone?) And of course we also have an enormous disorder. Elsewhere our latest Unique Facebook group, Unique amount in common with so many parents of children with other Russia, is also just starting up – so far it includes just a small special needs or disabilities around us in our own communities who number of members sharing very different experiences to mine here will often be walking the same path as us. -

©Ferrata Storti Foundation
Haematologica 2000; 85:1207-1210 Acute Leukemias case of the month Cytogenetic characterization of acute myeloid leukemia in Shwachman's syndrome. A case report FRANCESCA R. SPIRITO, BARBARA CRESCENZI, CATERINA MATTEUCCI, MASSIMO F. MARTELLI, CRISTINA MECUCCI Hematology and Bone Marrow Transplantation Unit, University of Perugia, Italy ABSTRACT We report on a case of acute myeloid leukemia in a tion. A recent analysis of 21 patients with SDS 17-year old boy affected by Shwachman Diamond showed that the incidence of myelodysplasia syndrome (SDS). Conventional cytogenetics at diag- and transformation to acute myeloid leukemia nosis revealed an abnormal clone with complex 4 karyotypic changes including typical myeloid aber- is 33% and 24%, respectively. A few cases of rations, such as monosomy 5, tetrasomy of chro- acute lymphoblastic leukemia have also been 5-7 mosome 8, trisomy 9, and deletion of the short arm described as well as one case of a juvenile form of chromosome 12. The boy was treated with con- of chronic myeloid leukemia.8 When leukemia ventional chemotherapy and reached complete develops, due to the preceding bone marrow remission of leukemia, confirmed by cytogenetics failure, serious complications may be induced and fluorescence in situ hybridization. Nevertheless by chemotherapy and, because of the underly- he failed to regenerate normal marrow cellularity ing organ dysfunctions, these patients should and blood cell count. Cytogenetic information on be managed with extreme caution when treat- hematologic malignancies in SDS patients are dis- cussed. ed with allogeneic bone marrow transplanta- 9-13 ©2000; Ferrata Storti Foundation tion. We describe here the cytogenetic char- acterization and clinical course of an acute Key words: Shwachman’s syndrome, leukemia, cytogenetics myeloid leukemia occurring in a young patient affected by Shwachman's syndrome. -

The Cytogenetics of Hematologic Neoplasms 1 5
The Cytogenetics of Hematologic Neoplasms 1 5 Aurelia Meloni-Ehrig that errors during cell division were the basis for neoplastic Introduction growth was most likely the determining factor that inspired early researchers to take a better look at the genetics of the The knowledge that cancer is a malignant form of uncon- cell itself. Thus, the need to have cell preparations good trolled growth has existed for over a century. Several biologi- enough to be able to understand the mechanism of cell cal, chemical, and physical agents have been implicated in division became of critical importance. cancer causation. However, the mechanisms responsible for About 50 years after Boveri’s chromosome theory, the this uninhibited proliferation, following the initial insult(s), fi rst manuscripts on the chromosome makeup in normal are still object of intense investigation. human cells and in genetic disorders started to appear, fol- The fi rst documented studies of cancer were performed lowed by those describing chromosome changes in neoplas- over a century ago on domestic animals. At that time, the tic cells. A milestone of this investigation occurred in 1960 lack of both theoretical and technological knowledge with the publication of the fi rst article by Nowell and impaired the formulations of conclusions about cancer, other Hungerford on the association of chronic myelogenous leu- than the visible presence of new growth, thus the term neo- kemia with a small size chromosome, known today as the plasm (from the Greek neo = new and plasma = growth). In Philadelphia (Ph) chromosome, to honor the city where it the early 1900s, the fundamental role of chromosomes in was discovered (see also Chap. -

Bone Marrow Karyotypes of Children with Nonlymphocytic Leukemia
Pediat. Res. 13: 1247-1254 (1979) Chromosome abnormalities nonlymphotic leukemia leukemia, childhood Bone Marrow Karyotypes of Children with Nonlymphocytic Leukemia A. HAGEMEIJER, G. E. VAN ZANEN, E. M. E. SMIT, AND K. HAHLEN Department of Cell Biology and Genetics (A. H.. E. M.E. S.) and Department of Pediatric Oncology (G. E. K Z.. K H.) Sophia Children's Hospital, Erasmus University, Rotterdam, The Netherlands Summary studies with modern banding techniques. The Ph' chromosome may be found in some cases if childhbod CML, and its presence Bone marrow (BM) karyotypes from 16 consecutive children can differentiate the adult type of CML with its more protracted presenting with nonlymphocytic leukemia were established with course, from the juvenile variant. Nonrandom acquired abnor- the use of banding techniques, before therapy. The two patients malities have also been reported in a small number of children with chronic myeloid leukemia (CML) showed the Philadelphia with ANLL: monosomy 7 was reported three times in AML, (Phl) translocation (9q+;22q-). Five of the 14 patients with an AMMoL, and EL (7, 10, 17) deletion 7q22 was found twice in acute nonlymphocytic leukemia (ANLL) presented no acquired AML (9), and monosomy 9 was described once in AML (8). An cytogenetic abnormalities, but one of these five showed a high extensive report of cytogenetic abnormalities in childhood leuke- level of hypodiploidy. One patient with AML evidenced a variant mia has been published by Zuelzer et al. in 1976 (3 l), but it deals of the Phl chromosome originated as a translocation (12p+;22q-). mainly with acute lymphocytic leukemia; furthermore, this study Nonrandom abnormalities (-7; 7q-; +8; t(8;21); -21) were found started before the use of banding techniques, making the karyo- in six patients, isolated or in association with other aberrations. -

Chromosome Abnormalities Identified in 457 Spontaneous Abortions And
Original Article doi: 10.5146/tjpath.2015.01303 Chromosome Abnormalities Identified in 457 Spontaneous Abortions and Their Histopathological Findings 457 Spontan Abortus Materyalinde Tespit Edilen Kromozomal Anomaliler ve Histopatolojik Bulguları Sezin YAKUT1, Havva Serap TORU2, Zafer ÇETİN3, Deniz ÖZEL4, Mehmet ŞİMŞEK5, İnanç MENDİLCİOĞLU5, Güven LÜLECİ1 Department of 1Medical Biology and Genetics, 2Pathology, 4Biostatistics and Medical Informatics and 5Obstetrics and Gynecology, Akdeniz University, School of Medicine, ANTALYA, TURKEY 3Department of Medical Biology and Genetics, SANKO University, School of Medicine, GAZİANTEP, TURKEY ABSTRACT ÖZ Objective: About 15% of clinically recognized pregnancies result Amaç: Klinik olarak gebeliklerin yaklaşık %15’i ilk trimesterde in spontaneous abortion in the first trimester and the vast majority abortus ile sonuçlanmakta olup büyük kısmında ise neden kromozom of these are the result of chromosome abnormalities. Studies of anormallikleridir. Çalışmalar göstermiştir ki ilk trimesterda abortusla chromosomal constitutions of first trimester spontaneous abortions sonuçlanan gebeliklerin %50’sinde kromozomal olarak karyotip have revealed that at least 50% of the abortions have an abnormal anomalileri görülmüştür. Çalışmada tek merkeze ait spontan abortus karyotype. In this study we aimed to report the single centre olgularındaki anomalileri sunmak amaçlandı. experience of anomalies detected in spontaneous abortions. Gereç ve Yöntem: Çalışmada tıbbi biyoloji ve genetik bölümümüze Material and Method: -
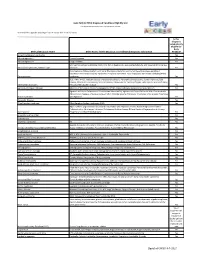
Early ACCESS Diagnosed Conditions List
Iowa Early ACCESS Diagnosed Conditions Eligibility List List adapted with permission from Early Intervention Colorado To search for a specific word type "Ctrl F" to use the "Find" function. Is this diagnosis automatically eligible for Early Medical Diagnosis Name Other Names for the Diagnosis and Additional Diagnosis Information ACCESS? 6q terminal deletion syndrome Yes Achondrogenesis I Parenti-Fraccaro Yes Achondrogenesis II Langer-Saldino Yes Schinzel Acrocallosal syndrome; ACLS; ACS; Hallux duplication, postaxial polydactyly, and absence of the corpus Acrocallosal syndrome, Schinzel Type callosum Yes Acrodysplasia; Arkless-Graham syndrome; Maroteaux-Malamut syndrome; Nasal hypoplasia-peripheral dysostosis-intellectual disability syndrome; Peripheral dysostosis-nasal hypoplasia-intellectual disability (PNM) Acrodysostosis syndrome Yes ALD; AMN; X-ALD; Addison disease and cerebral sclerosis; Adrenomyeloneuropathy; Siemerling-creutzfeldt disease; Bronze schilder disease; Schilder disease; Melanodermic Leukodystrophy; sudanophilic leukodystrophy; Adrenoleukodystrophy Pelizaeus-Merzbacher disease Yes Agenesis of Corpus Callosum Absence of the corpus callosum; Hypogenesis of the corpus callosum; Dysplastic corpus callosum Yes Agenesis of Corpus Callosum and Chorioretinal Abnormality; Agenesis of Corpus Callosum With Chorioretinitis Abnormality; Agenesis of Corpus Callosum With Infantile Spasms And Ocular Anomalies; Chorioretinal Anomalies Aicardi syndrome with Agenesis Yes Alexander Disease Yes Allan Herndon syndrome Allan-Herndon-Dudley -

Chromosomal Disorders: Background and Neuroradiology
Chromosomal Disorders: Background and Neuroradiology Ashok J. Kumar, 1 Thomas P. Naidich, Gail Stetten, Allan L. Reiss, Henry Wang, George H. Thomas, and OrestHurko From the Division of Neuroradiology (AJK, HW), Departments of Neurology (OH), Psychiatry (ALR), and Gynecology and Obstetrics (GS), The Johns Hopkins University School of Medicine; and the Kennedy Institutes, Baltimore, MD (GHT) and Baptist Hospital (TPN), Miami, FL Chromosomal aberrations, and their associated malities can be detected by neuroimaging. 2) syndromes of dysmorphism and malformations Most of the clinical syndromes associated with of multiple organ systems, have been long rec chromosomal abnormalities are notoriously vari ognized as significant causes of severe mental able, requiring individual assessment of each pa impairment. With a few major exceptions, these tient. Incompletely overlapping partial aneu clinical syndromes have only recently been cat ploidies, for example, give rise to broadly similar alogued as systematically ( 1, 2) as have been syndromes, but slight differences in their extent single-gene disorders. The neuropathologic fea may considerably alter the resultant phenotype. tures of many of these syndromes have been Neuroimaging can help to characterize the asso characterized only broadly, if at all. Not surpris ciated CNS pathology and facilitate proper man ingly, there is no detailed compendium of the agement of the patient. neuroradiologic features of the malformations of It is our purpose to introduce the chromosomal the central nervous system (CNS) associated with disorders to the general neuroradiologist by con various chromosomal aberrations. centrating on basic concepts and by giving spe Certain chromosomal aberrations, such as tri cific illustrations of some of the more commonly somy 21 and the associated Down syndrome, are encountered syndromes. -

The Clinical Utility of a SNP Microarray in Patients with Epilepsy at a Tertiary Medical Center
The Clinical Utility of a SNP Microarray in Patients with Epilepsy at a Tertiary Medical Center A thesis submitted to the Graduate School of the University of Cincinnati in partial fulfillment of the requirements for the degree of Master of Science In the College of Medicine April 2013 by Sarah A. Hrabik BS, University of Dayton, 2011 Committee Chair: Derek E. Neilson, MD Committee Members: Christine G. Spaeth, MS, CGC Valentina Pilipenko, PhD Abstract Background: Microarray testing has revolutionized clinical cytogenetics, as it provides a significantly higher resolution and greater clinical yield than karyotype analysis. Previously, microarray studies have been performed in patients with developmental delay, intellectual disability, autism, and multiple congenital anomalies. This study assessed the clinical utility of Single Nucleotide Polymorphism (SNP) microarray in patients with epilepsy. Methods: Study subjects were patients (between the ages of birth-23 years) who were diagnosed with epilepsy and had a SNP microarray performed at Cincinnati Children’s Hospital Medical Center. Chi- square test and Fisher’s exact test were employed to examine the association of microarray results and the following laboratory or clinical features: brain MRI, seizure type, and functional and structural malformations. Results: One hundred and forty seven individuals met all study criteria. Of the 147 individuals studied, 17.7% (26/147) had an abnormal microarray. However, there was no difference in frequency of abnormal brain MRI or seizure type between the abnormal and normal microarray groups. Musculoskeletal malformations occurred in 38.5% of subjects with abnormal microarray results and 14.1% of subjects with a normal microarray (p<.0035). -

Trisomy 9 Syndrome in an Infant with Ambiguous Genitalia
TITLE Trisomy 9 Syndrome in an Infant with Ambiguous Genitalia •Authors Parastoo Rostami1, Maryam Nakhaeimoghadam1, Arya Sotoudeh1, Reihaneh Mohsenipour1, Nima Rezaei2,3,4 •1 Department of Pediatric Endocrinology, 2 Research Center for Immunodeficiencies, Children's Medical Center, 3Department of Immunology, School of Medicine, Tehran University of Medical Sciences, 3Universal Scientific Education and Research Network (USERN), Tehran, Iran OBJECTIVES Case report •The pericentric inversion of •The patient is a 4-month boy who was referred to the Children’s Medical Center, the Pediatrics Center of Excellence Chromosome 9 is the most common in Iran, because of ambiguous genitalia. There was no problem abnormality of human chromosomal after in mother pregnancy, while the fetal ultrasounds was also trisomy 21 and fragile x (1), which is normal during pregnancy. Birth weight was 3200 gram, length estimated to be seen up to 1-3 percent in 49 cm, and head circumference was 34 cm. He has normal general population (1-4). Although this growth and development. On physical examination, the chromosomal abnormality might not lead to external genitalia was ambiguous. There was small phallus, any clinical presentation in the most cases while palpaple gonads in scrotom was detected. He haD (5), several signs and symptoms have perinoscerotal hypospadiasis (Figure 1). Laboratory tests, such already been reported in some cases such as DHEAS (Dihydroepiandrostrone, 17OHP (Hydroxy progesterone), Andrestandione, sodium, potassium, cortiso l, as infertility, -

Non-Invasive Prenatal Test (NIPT)+ Microdeletion Panel + Trisomies 9 and 16
E21151 Analysis Report : PrenatalSafe® Plus - Non-Invasive Prenatal Test (NIPT)+ Microdeletion panel + trisomies 9 and 16 Report date:07/07/2016 Time:18:51 Referring Centre details Referring Centre: City: Patient’s details Surname: Name: Date of birth: Place of birth: Ethnicity: Sex: F Physician: Sample’s ID: Indication: Clinical details: Sample’s details Sample Type: blood Our Sample’s ID: E21151 Acceptance Date: 29/06/2016 Acceptance Time: 14:31 Collection Date: 28/06/2016 Analysis details Analysis performed: PrenatalSafe® Plus - Non-Invasive Prenatal Test (NIPT)+ Microdeletion panel + trisomies 9 and 16 Code OMIM: Mode of Inheritance: Gene investigated: OMIM: Reference Sequence: Method of Analysis: Massive Parallel Sequencing (MPS) mediante tecnica Next Generation Sequencing (NGS) Diagnostic strategy: Sample Processing Date: 30/06/2016 Analysis completed: 07/07/2016 Page 1 / 2 E21151 Analysis Results Result: POSITIVE Test Result. Loss of chromosome 22 material in the region 22q11.2. No aneuploidy detected for chromosomes 21, 13, 18, 16, 9 and sex chromosomes. No other microdeletions detected in the regions of interest. Fetal sex consistent with Female. Fetal Fraction: 8.7% Interpretation: A loss of chromosome 22 material was observed. It is estimated to be 4 Mb in size and is suggestive of a deletion in the region 22q11.2, which is associated with DiGeorge syndrome. Genetic counseling and clinical correlation are recommended. Confirmatory testing is required if fetal confirmation and clinical interpretation of the suspected event are desired. Please refer to the “Performance” and “Limitations of the Test” sections of the enclosed technical report for additional information. Technical notes: PrenatalSafe® Plus test is designed to detect common chromosome aneuploidies and is validated for chromosomes 21, 18, 16, 13, 9, X and Y. -

Trisomy 9 Mosaicism FTNW
Trisomy 9 mosaicism rarechromo.org Trisomy 9 mosaicism (T9M) is a rare genetic condition caused by having an extra chromosome (trisomy) in some of the cells of the body. Like most other chromosome disorders, this makes developmental problems more likely. All the same, the effects of a chromosome disorder can vary very much between individuals and this is especially true of people with a mosaic form of a disorder, where cells do not all have the same chromosome or gene content. Chromosomes are made up mostly of DNA. They are structures in the nucleus of the body’s cells that carry genetic information known as genes. Chromosomes usually come in pairs, one chromosome from each pair inherited from the father and the other from the mother. They are numbered 1 to 22 approximately from largest to smallest, in addition to the sex chromosomes, X and Y, making 46 chromosomes in all. In trisomy 9 mosaicism there is an extra chromosome 9, making a total of 47 chromosomes, in some cells in the body. The remaining cells have the usual number of 46 chromosomes, with two copies of chromosome 9 in each cell. Diagnosis: the karyotype When you are told about your child’s chromosome disorder, you are often given a karyotype. This is a way of describing what the chromosomes look like. In trisomy 9 mosaicism, the karyotype usually looks something like this: 47,XY,+9[15]/46,XY[85] There are two different cell lines, separated by / In the first cell line: 47 The number of chromosomes in the cells in this cell line XY The two sex chromosomes, XY for males; XX for females +9 There is an extra chromosome 9 [15] Out of 100 cells – 15 + 85 – examined, 15 have the extra chromosome 9 In the second cell line: 46 The number of chromosomes in the cells in this cell line.