Malaria Epidemiology and Key Control Interventions in the Democratic Republic of Congo
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Deforestation and Forest Degradation Activities in the DRC
E4838 V5 DEMOCRATIC REPUBLIC OF THE CONGO MINISTRY FOR THE ENVIRONMENT, NATURE CONSERVATION AND TOURISM Public Disclosure Authorized STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ PROCESS Public Disclosure Authorized BASELINE REPORT STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ Public Disclosure Authorized PROCESS Public Disclosure Authorized October 2014 STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ PROCESS in the DRC INDEX OF REPORTS Environmental Analysis Document Assessment of Risks and Challenges REDD+ National Strategy of the DRC Strategic Environmental and Social Assessment Report (SESA) Framework Document Environmental and Social Management Framework (ESMF) O.P. 4.01, 4.04, 4.37 Policies and Sector Planning Documents Pest and Pesticide Cultural Heritage Indigenous Peoples Process Framework Management Management Planning Framework (FF) Resettlement Framework Framework (IPPF) O.P.4.12 Policy Framework (PPMF) (CHMF) O.P.4.10 (RPF) O.P.4.09 O.P 4.11 O.P. 4.12 Consultation Reports Survey Report Provincial Consultation Report National Consultation of June 2013 Report Reference and Analysis Documents REDD+ National Strategy Framework of the DRC Terms of Reference of the SESA October 2014 Strategic Environmental and Social Assessment SESA Report TABLE OF CONTENTS Introductory Note ........................................................................................................................................ 9 1. Preface ............................................................................................................................................ -
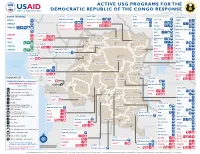
ACTIVE USG PROGRAMS for the DEMOCRATIC REPUBLIC of the CONGO RESPONSE Last Updated 07/27/20
ACTIVE USG PROGRAMS FOR THE DEMOCRATIC REPUBLIC OF THE CONGO RESPONSE Last Updated 07/27/20 BAS-UELE HAUT-UELE ITURI S O U T H S U D A N COUNTRYWIDE NORTH KIVU OCHA IMA World Health Samaritan’s Purse AIRD Internews CARE C.A.R. Samaritan’s Purse Samaritan’s Purse IMA World Health IOM UNHAS CAMEROON DCA ACTED WFP INSO Medair FHI 360 UNICEF Samaritan’s Purse Mercy Corps IMA World Health NRC NORD-UBANGI IMC UNICEF Gbadolite Oxfam ACTED INSO NORD-UBANGI Samaritan’s WFP WFP Gemena BAS-UELE Internews HAUT-UELE Purse ICRC Buta SCF IOM SUD-UBANGI SUD-UBANGI UNHAS MONGALA Isiro Tearfund IRC WFP Lisala ACF Medair UNHCR MONGALA ITURI U Bunia Mercy Corps Mercy Corps IMA World Health G A EQUATEUR Samaritan’s NRC EQUATEUR Kisangani N Purse WFP D WFPaa Oxfam Boende A REPUBLIC OF Mbandaka TSHOPO Samaritan’s ATLANTIC NORTH GABON THE CONGO TSHUAPA Purse TSHOPO KIVU Lake OCEAN Tearfund IMA World Health Goma Victoria Inongo WHH Samaritan’s Purse RWANDA Mercy Corps BURUNDI Samaritan’s Purse MAI-NDOMBE Kindu Bukavu Samaritan’s Purse PROGRAM KEY KINSHASA SOUTH MANIEMA SANKURU MANIEMA KIVU WFP USAID/BHA Non-Food Assistance* WFP ACTED USAID/BHA Food Assistance** SA ! A IMA World Health TA N Z A N I A Kinshasa SH State/PRM KIN KASAÏ Lusambo KWILU Oxfam Kenge TANGANYIKA Agriculture and Food Security KONGO CENTRAL Kananga ACTED CRS Cash Transfers For Food Matadi LOMAMI Kalemie KASAÏ- Kabinda WFP Concern Economic Recovery and Market Tshikapa ORIENTAL Systems KWANGO Mbuji T IMA World Health KWANGO Mayi TANGANYIKA a KASAÏ- n Food Vouchers g WFP a n IMC CENTRAL y i k -

UNJHRO) MONUSCO – OHCHR March 2021 REPORTED HUMAN RIGHTS VIOLATIONS in DEMOCRATIC REPUBLIC of the CONGO (DRC)
Protection of civilians: Human rights violations documented in provinces affected by conflict United Nations Joint Human Rights Office in the DRC (UNJHRO) MONUSCO – OHCHR March 2021 REPORTED HUMAN RIGHTS VIOLATIONS IN DEMOCRATIC REPUBLIC OF THE CONGO (DRC) Figure 1. Percentage of violations per territory Figure 2. Number of violations per province in DRC SOUTH CENTRAL AFRICAN REPUBLIC SUDAN North Kivu Tanganyika Bas-Uele Haut-Uele Masisi 79% 21 Kalemie 36% 65 North-Ubangi Beni 64 36 Manono0 100 2 UGANDA CAMEROON South-Ubangi Rutshuru 69 31 Moba0 100 Ituri Mongala Lubero 29 71 77 Nyiragongo 86 14 Maniema Tshopo Walikale 90 10 Kabambare 63% 395 CONGO Equateur North Butembo0 100 Kasongo0 100 Kivu Kibombo0 100 GABON Tshuapa 359 South Kivu RWANDA Kasai Shabunda 82% 18 Mai-Ndombe Kamonia (Kas.)0 100% Kinshasa Uvira 33 67 5 BURUNDI Llebo (Kas.)0 100 Sankuru 15 63 Fizi 33 67 Kasai South Tshikapa (Kas.)0 100 Maniema Kivu Kabare 100 0 Luebo (Kas.)0 100 Kwilu 23 TANZANIA Walungu 29 71 Kananga (Kas. C)0 100 Lomami Bukavu0 100 22 4 Demba (Kas. C)0 100 Kongo 46 Mwenga 67 33 Central Luiza (Kas. C)0 100 Kwango Tanganyika Kalehe0 100 Kasai Dimbelenge (Kas. C)0 100 Central Haut-Lomami Ituri Miabi (Kas. O)0 100 Kasai 0 100 ANGOLA Oriental Irumu 88% 12 Mbuji-Mayi (Kas. O) Haut- Djugu 64 36 Lualaba Bas-Uele Katanga Mambasa 30 70 Buta0 100% Mahagi 100 0 % by armed groups % by State agents The boundaries and names shown and designations ZAMBIA used on this map do not imply official endorsement or acceptance by the United Nations. -

Emergency Telecommunications Cluster (ETC) in the Democratic Republic of Congo Was Activated on 20 November 2017
Democratic Republic of Congo (DRC) – Conflict ETC Situation Report #3 Reporting period 24/01/18 to 15/06/18 The Emergency Telecommunications Cluster (ETC) in the Democratic Republic of Congo was activated on 20 November 2017. Under the global leadership of the World Food Programme (WFP), the ETC is coordinating the ICT response with government, the private sector and humanitarian partners on the ground. Highlights The Emergency Telecommunications Cluster (ETC) is providing shared security telecommunications services to support humanitarian operations in the Kasai region, South Kivu and Tanganyika. These services are available in Kananga and Tshikapa (Kasai-Occidental), Mbuji-Mayi (Kasai-Oriental), Bukavu (South Kivu) and in Kalemie (Tanganyika). The ETC carried out assessment missions in Sud Kivu and Tanganika provinces in May 2018 to evaluate evolving needs and adjust plans Healthcare worker disinfects areas where cases of deaths from Ebola have been reported. accordingly. Photo: WHO Due to the Ebola outbreak in May 2018, the ETC has submitted a funding application to the United States Agency for International Development (USAID) to provide services in the affected areas in the North-West part of DRC. Situation Overview On 8 May 2018, the Ministry of Health of the Democratic Republic of the Congo notified the World Health Organization (WHO) of an Ebola outbreak in Bikoro Health Zone, Equateur Province. According to the Office for the Coordination of Humanitarian Affairs (OCHA), the epidemic seems to be stabilizing with zero deaths and zero new cases since 21 May. Bikoro, Iboko, Wangata and Itipo, are affected health zones located in a dense forest intertwined by rivers and lakes in Équateur province. -
From Resource War to ‘Violent Peace’ Transition in the Democratic Republic of the Congo (DRC) from Resource War to ‘Violent Peace’
paper 50 From Resource War to ‘Violent Peace’ Transition in the Democratic Republic of the Congo (DRC) From Resource War to ‘Violent Peace’ Transition in the Democratic Republic of Congo (DRC) by Björn Aust and Willem Jaspers Published by ©BICC, Bonn 2006 Bonn International Center for Conversion Director: Peter J. Croll An der Elisabethkirche 25 D-53113 Bonn Germany Phone: +49-228-911960 Fax: +49-228-241215 E-mail: [email protected] Internet: www.bicc.de Cover Photo: Willem Jaspers From Resource War to ‘Violent Peace’ Table of contents Summary 4 List of Acronyms 6 Introduction 8 War and war economy in the DRC (1998–2002) 10 Post-war economy and transition in the DRC 12 Aim and structure of the paper 14 1. The Congolese peace process 16 1.1 Power shifts and developments leading to the peace agreement 17 Prologue: Africa’s ‘First World War’ and its war economy 18 Power shifts and the spoils of (formal) peace 24 1.2 Political transition: Structural challenges and spoiler problems 29 Humanitarian Situation and International Assistance 30 ‘Spoiler problems’ and political stalemate in the TNG 34 Systemic Corruption and its Impact on Transition 40 1.3 ‘Violent peace’ and security-related liabilities to transition 56 MONUC and its contribution to peace in the DRC 57 Security-related developments in different parts of the DRC since 2002 60 1.4 Fragility of security sector reform 70 Power struggles between institutions and parallel command structures 76 2. A Tale of two cities: Goma and Bukavu as case studies of the transition in North and South Kivu -

UNHAS DRC Weekly Flight Schedule
UNHAS DRC Weekly Flight Schedule Effective from 09th June 2021 AIRCRAFT MONDAY TUESDAY WEDNESDAY THURSDAY FRIDAY SATURDAY KINSHASA ETD From To ETA ETD From To ETA ETD From To ETA ETD From To ETA ETD From To ETA ETD From To ETA 08:00 KINSHASA MBANDAKA 09:00 08:00 KINSHASA MBANDAKA 09:30 08:30 KINSHASA BRAZZAVILLE 08:45 08:00 KINSHASA MBANDAKA 09:30 08:00 KINSHASA MBANDAKA 09:30 UNO-234H 09:30 MBANDAKA GBADOLITE 10:55 10:00 MBANDAKA YAKOMA 11:40 09:30 BRAZZAVILLE MBANDAKA 11:00 10:00 MBANDAKA GBADOLITE 11:25 10:00 MBANDAKA LIBENGE 11:00 5Y-VVI 11:25 GBADOLITE BANGUI 12:10 12:10 YAKOMA MBANDAKA 13:50 11:30 MBANDAKA IMPFONDO 12:00 11:55 GBADOLITE MBANDAKA 13:20 11:30 LIBENGE BANGUI 11:50 DHC-8-Q400 13:00 BANGUI MBANDAKA 14:20 14:20 MBANDAKA KINSHASA 15:50 12:30 IMPFONDO MBANDAKA 13:00 13:50 MBANDAKA KINSHASA 15:20 12:40 BANGUI MBANDAKA 14:00 SPECIAL FLIGHTS OR MAINTENANCE 14:50 MBANDAKA KINSHASA 16:20 13:30 MBANDAKA BRAZZAVILLE 15:00 14:30 MBANDAKA KINSHASA 16:00 15:30 BRAZZAVILLE KINSHASA 15:45 AD HOC CARGO FLIGHT TSA WITH UNHCR KINSHASA ETD From To ETA ETD From To ETA ETD From To ETA ETD From To ETA ETD From To ETA ETD From To ETA 09:00 KINSHASA KANANGA 11:15 08:00 KINSHASA KALEMIE 11:15 09:00 KINSHASA KANANGA 11:15 UNO-207H 11:45 KANANGA GOMA 13:10 11:45 KALEMIE GOMA 12:35 11:45 KANANGA GOMA 13:10 5Y-CRZ SPECIAL FLIGHTS OR MAINTENANCE SPECIAL FLIGHTS OR MAINTENANCE SPECIAL FLIGHTS OR MAINTENANCE EMB-145 LR 14:10 GOMA KANANGA 15:35 13:35 GOMA KINSHASA 14:50 14:10 GOMA KANANGA 15:35 16:05 KANANGA KINSHASA 16:20 16:05 KANANGA KINSHASA 16:20 -

An Estimated Dynamic Model of African Agricultural Storage and Trade
High Trade Costs and Their Consequences: An Estimated Dynamic Model of African Agricultural Storage and Trade Obie Porteous Online Appendix A1 Data: Market Selection Table A1, which begins on the next page, includes two lists of markets by country and town population (in thousands). Population data is from the most recent available national censuses as reported in various online databases (e.g. citypopulation.de) and should be taken as approximate as census years vary by country. The \ideal" list starts with the 178 towns with a population of at least 100,000 that are at least 200 kilometers apart1 (plain font). When two towns of over 100,000 population are closer than 200 kilometers the larger is chosen. An additional 85 towns (italics) on this list are either located at important transport hubs (road junctions or ports) or are additional major towns in countries with high initial population-to-market ratios. The \actual" list is my final network of 230 markets. This includes 218 of the 263 markets on my ideal list for which I was able to obtain price data (plain font) as well as an additional 12 markets with price data which are located close to 12 of the missing markets and which I therefore use as substitutes (italics). Table A2, which follows table A1, shows the population-to-market ratios by country for the two sets of markets. In the ideal list of markets, only Nigeria and Ethiopia | the two most populous countries | have population-to-market ratios above 4 million. In the final network, the three countries with more than two missing markets (Angola, Cameroon, and Uganda) are the only ones besides Nigeria and Ethiopia that are significantly above this threshold. -

Democratic Republic of the Congo
DEMOCRATIC REPUBLIC OF THE CONGO MONTHLY REFUGEE STATISTICS Situation as of November 30, 2020 Type Age 0-4 5-11 12-17 18-59 60+ Total % Total Rural (out of camp) 75,821 105,155 62,321 131,723 9,121 384,141 73.3% Total Camps/Sites 23,501 39,046 20,860 47,419 2,981 133,807 25.5% Total 524,302 Total Urban 620 1,487 1,132 2,939 176 6,354 1.2% Grand Total 99,942 145,688 84,313 182,081 12,278 524,302 Refugee Population in DRC Refugee Population by Province in DRC Country Female Male Total % Province Main Location Type Female Male Total Angola** 179 235 414 0.08% Bas Uele Ango & Bondo Rural 22,519 17,697 40,216 Burundi* 25,022 23,530 48,552 9.26% Equateur Disperced Rural 143 213 356 CAR* 91,469 79,582 171,051 32.62% Haut Katanga Lubumbashi & Urb. & Rur. 1,742 Arounds 808 934 Rep.Congo 251 386 637 0.12% Haut Uele Dungu, Doruma Rural 22,311 19,394 41,705 Rwanda*** 107,534 106,440 213,974 40.81% Ituri Aru & Ariwara Rural 25,506 22,351 47,857 S. Sudan* 47,837 41,737 89,574 17.08% Kasai Oriental Tshiala Rural 2 6 8 Kinshasa & Sudan 8 24 32 0.01% Kinshasa Urb. & Rur. 790 outskirts 375 415 Bas Fleuve, Uganda 13 10 23 0.004% Kongo Central Rural 817 MbanzaNg. & Kimaza 328 489 Somalia 7 7 14 0.003% Lomami Luila &MweneDitu Rural 430 456 886 Ivory Coast 4 3 7 0.001% Lualaba Dilolo,Sandoa &Kolwezi Rural 590 596 1,186 Other 10 14 24 0.005% Maniema Pangi, Kailo&Lukolo Rural 203 269 472 Lubero, Masisi, Total 272,334 251,968 524,302 100% Nord Kivu Urb. -

Urban Population Map Gis Unit, Monuc 12°E 14°E 16°E 18°E 20°E 22°E 24°E 26°E 28°E 30°E
DEMOCRATIC REPUBLIC OF CONGO Map No- KINSUB1614 AFRICA URBAN POPULATION MAP GIS UNIT, MONUC 12°E 14°E 16°E 18°E 20°E 22°E 24°E 26°E 28°E 30°E CENTRAL AFRICAN REPUBLIC SUDAN CAMEROON Mobayi-Mbongo Zongo Bosobolo Ango N Gbadolite N ° ° 4 Yakoma 4 Niangara Libenge Bondo Dungu Gemena Mombombo Bambesa Poko Isiro Aketi Bokungu Buta Watsa Aru r e v i Kungu R i g Dimba n a b Binga U Lisala Bumba Mahagi Wamba Nioka N N ° C ° 2 o 2 ng o Djugu R i v Lake Albert Bongandanga er Irumu Bomongo Bunia Basankusu Basoko Bafwasende Yahuma Kituku Yangambi Bolomba K ii s a n g a n ii Beni Befale Lubero UGANDA Katwa N M b a n d a k a N ° ° 0 0 Butembo Ingende Ubundu Lake Edward Kayna GABON Bikoro Opala Lubutu Kanyabayonga CONGO Isangi Boende Kirumba Lukolela Rutshuru Ikela Masisi Punia Kiri WalikaleKairenge Monkoto G o m a Inongo S S ° Lake Kivu ° 2 RWANDA 2 Bolobo Lomela Kamisuku Shabunda B u k a v u Walungu Kutu Mushie B a n d u n d u Kamituga Ilebo K ii n d u Oshwe Dekese Lodja BURUNDI Kas Katako-Kombe ai R Uvira iver Lokila Bagata Mangai S Kibombo S ° ° 4 4 K ii n s h a s a Dibaya-Lubwe Budja Fizi Bulungu Kasongo Kasangulu Masi-Manimba Luhatahata Tshela Lubefu Kenge Mweka Kabambare TANZANIA Idiofa Lusambo Mbanza-Ngungu Inkisi ANGOLA Seke-Banza Luebo Lukula Kinzau-Vuete Lubao Kongolo Kikwit Demba Inga Kimpese Boma Popokabaka Gungu M b u j i - M a y i Songololo M b u j i - M a y i Nyunzu S S ° M a tt a d ii ° 6 K a n a n g a 6 K a n a n g a Tshilenge Kabinda Kabalo Muanda Feshi Miabi Kalemie Kazumba Dibaya Katanda Kasongo-Lunda Tshimbulu Lake Tanganyika Tshikapa -

Republique Democratique Du Congo Ministere Des
REPUBLIQUE DEMOCRATIQUE DU CONGO MINISTERE DES FINANCES DIRECTION GENERALE DES IMPÔTS DIRECTION DE L'ASSIETTE FISCALE REPERTOIRE DES CONTRIBUABLES ASSUJETTIS A LA TVA, ARRETE AU 28 FEVRIER 2019 FORME SIEGE OU ANCIEN SERVICE NOUVEAU SERVICE N NIF NOMS OU RAISON SOCIALE SIGLE ADRESSE SECTEUR DACTIVITE ETAT SOCIETE JURIDIQUE SUCCURSALE GESTIONNAIRE GESTIONNAIRE Commerce Général et 1 A1200188T PM 3 G SERVICES SPRL SIEGE SOCIAL Q/MAINDOMBE N°35/C MATETE Import-Export EN ACTIVITE CDI / KINSHASA CDI / KINSHASA AV. NZOBE N°128 Q/BISENGO Commerce Général et 2 A1300881Y PM 3 rd YES SPRL SIEGE SOCIAL C/BANDALUNGWA Import-Export EN ACTIVITE CDI / KINSHASA CDI / KINSHASA Prestation de services 3 A1610526K PM 360° COMMUNICATIONS SARL SIEGE SOCIAL AV. DE LA JUSTICE N°44 C/GOMBE et travaux immobiliers EN ACTIVITE CDI / KINSHASA CDI / KINSHASA Commerce Général et 4 A1505996K PM 3MC SARL SIEGE SOCIAL AV.DEAV. LUKUSA LA VALLEE N°2 Q/GOLF N°4B APP. C/GOMBE RESIDENCE Import-Export EN ACTIVITE CDI / KINSHASA CDI / KINSHASA PRESTIGE C/GOMBE D/LUKUNGA Prestation de services 5 A1419266H PM 4CIT SOFTWARE SOLUTIONS LIMITED SIEGE SOCIAL V/KINSHASA et travaux immobiliers EN ACTIVITE CDI / KINSHASA CDI / KINSHASA 4K PYRAMIDE DE CONSTRUCTIONS ET Prestation de services 6 A1515786B PM TRAVAUX SARL SIEGE SOCIAL AV. KABAYIDI N°68 Q/NDANU C/LIMETE Télécom.et travaux et immobiliers nouvelles EN ACTIVITE CDI / KINSHASA CDI / KINSHASA AV.BAKONGO N°644 C/GOMBE technologies 7 A1408818B PM 7 SUR 7.CD SIEGE SOCIAL D/LUKUNGA V/KINSHASA d'information EN ACTIVITE CDI / KINSHASA CDI / KINSHASA Commerce Général et 8 A1515519L PM A CASA MIA SARL SIEGE SOCIAL AV. -

Perpetuation of Instability in the Democratic Republic of the Congo: When the Kivus Sneeze, Kinshasa Catches a Cold
Perpetuation of instability in the Democratic Republic of the Congo: When the Kivus sneeze, Kinshasa catches a cold By Joyce Muraya and John Ahere 22 YEARS OF CONTRIBUTING TO PEACE ISSUE 1, 2014 Perpetuation of instability in the Democratic Republic of the Congo: When the Kivus sneeze, Kinshasa catches a cold By Joyce Muraya and John Ahere Occasional Paper Series: Issue 1, 2014 About ACCORD The African Centre for the Constructive Resolution of Disputes (ACCORD) is a non-governmental organisation working throughout Africa to bring creative solutions to the challenges posed by conflict on the continent. ACCORD’s primary aim is to influence political developments by bringing conflict resolution, dialogue and institutional development to the forefront as alternatives to armed violence and protracted conflict. Acknowledgements The authors extend their appreciation to all colleagues who supported the development and finalisation of this paper, including Daniel Forti, Charles Nyuykonge and Sabrina Ensenbach for their invaluable contributions to the paper’s structure and content and to Petronella Mugoni for her assistance in formatting the paper. The authors also appreciate the cooperation of colleagues in ACCORD’s Peacebuilding and Peacemaking units, for affording them the time and space to conduct the research necessary for writing this publication. About the authors Joyce Muraya holds a Master of Arts degree in International Relations from the United States International University in Nairobi, Kenya. Muraya served in Kenya’s Ministry of Foreign Affairs for a year and a half and participated in a nine-month internship programme in the Peacebuilding Unit at ACCORD. She has published on gender and women’s issues, with a focus on women’s reproductive rights. -

Implanter Une Institution De Microfinance Ou Une Banque Dans Le Grand Kasaï
IMPLANTER UNE INSTITUTION DE MICROFINANCE OU UNE BANQUE DANS LE GRAND KASAÏ MBUJI-MAYI - KANANGA -TSHIKAPA Décembre 2013 www.fpm.cd IMPLANTER UNE INSTITUTION DE MICROFINANCE OU UNE BANQUE LA PROVINCE DANS LE GRAND KASAÏ KASAÏ ORIENTAL MBUJI-MAYI - KANANGA - TSHIKAPA Décembre 2013 www.fpm.cd LA PROVINCE DU KASAÏ OCCIDENTAL KANANGA IMPLANTER UNE INSTITUTION LA PROVINCE DE MICROFINANCE OU UNE BANQUE DU KASAÏ ORIENTAL DANS LE GRAND KASAÏ MBUJI-MAYI – KANANGA - TSHIKAPA Décembre 2013 www.fpm.cd MBUJI-MAYI IMPLANTER UNE INSTITUTION DE MICROFINANCE OU UNE BANQUE DANS LE GRAND KASAI TABLE DES MATIERES Synthèse ................................................................................................................................ 6 Contexte et méthodologie .............................................................................................................. 10 Données socio – économiques ..................................................................................................... 12 Des MPME en recherche de produits et services financiers classiques ..................................... 23 Quelques structures financières formelles qui n’absorbent pas la demande ............................. 27 Analyse des écarts et scénarios .................................................................................................... 29 Annexe 1 : Synthèse des coûts d’investissement et de fonctionnement .................................... 35 Annexe 2 : Coût d’installation d’une agence bancaire ................................................................