RPCN Content
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nitrate Prodrugs Able to Release Nitric Oxide in a Controlled and Selective
Europäisches Patentamt *EP001336602A1* (19) European Patent Office Office européen des brevets (11) EP 1 336 602 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.7: C07C 205/00, A61K 31/00 20.08.2003 Bulletin 2003/34 (21) Application number: 02425075.5 (22) Date of filing: 13.02.2002 (84) Designated Contracting States: (71) Applicant: Scaramuzzino, Giovanni AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU 20052 Monza (Milano) (IT) MC NL PT SE TR Designated Extension States: (72) Inventor: Scaramuzzino, Giovanni AL LT LV MK RO SI 20052 Monza (Milano) (IT) (54) Nitrate prodrugs able to release nitric oxide in a controlled and selective way and their use for prevention and treatment of inflammatory, ischemic and proliferative diseases (57) New pharmaceutical compounds of general effects and for this reason they are useful for the prep- formula (I): F-(X)q where q is an integer from 1 to 5, pref- aration of medicines for prevention and treatment of in- erably 1; -F is chosen among drugs described in the text, flammatory, ischemic, degenerative and proliferative -X is chosen among 4 groups -M, -T, -V and -Y as de- diseases of musculoskeletal, tegumental, respiratory, scribed in the text. gastrointestinal, genito-urinary and central nervous sys- The compounds of general formula (I) are nitrate tems. prodrugs which can release nitric oxide in vivo in a con- trolled and selective way and without hypotensive side EP 1 336 602 A1 Printed by Jouve, 75001 PARIS (FR) EP 1 336 602 A1 Description [0001] The present invention relates to new nitrate prodrugs which can release nitric oxide in vivo in a controlled and selective way and without the side effects typical of nitrate vasodilators drugs. -

Ayahuasca: Spiritual Pharmacology & Drug Interactions
Ayahuasca: Spiritual Pharmacology & Drug Interactions BENJAMIN MALCOLM, PHARMD, MPH [email protected] MARCH 28 TH 2017 AWARE PROJECT Can Science be Spiritual? “Science is not only compatible with spirituality; it is a profound source of spirituality. When we recognize our place in an immensity of light years and in the passage of ages, when we grasp the intricacy, beauty and subtlety of life, then that soaring feeling, that sense of elation and humility combined, is surely spiritual. The notion that science and spirituality are somehow mutually exclusive does a disservice to both.” – Carl Sagan Disclosures & Disclaimers No conflicts of interest to disclose – I don’t get paid by pharma and have no potential to profit directly from ayahuasca This presentation is for information purposes only, none of the information presented should be used in replacement of medical advice or be considered medical advice This presentation is not an endorsement of illicit activity Presentation Outline & Objectives Describe what is known regarding ayahuasca’s pharmacology Outline adverse food and drug combinations with ayahuasca as well as strategies for risk management Provide an overview of spiritual pharmacology and current clinical data supporting potential of ayahuasca for treatment of mental illness Pharmacology Terms Drug ◦ Term used synonymously with substance or medicine in this presentation and in pharmacology ◦ No offense intended if I call your medicine or madre a drug! Bioavailability ◦ The amount of a drug that enters the body and is able to have an active effect ◦ Route specific: bioavailability is different between oral, intranasal, inhalation (smoked), and injected routes of administration (IV, IM, SC) Half-life (T ½) ◦ The amount of time it takes the body to metabolize/eliminate 50% of a drug ◦ E.g. -

The Migraine Attack As a Homeostatic, Neuroprotective Response to Brain Oxidative Stress: Preliminary Evidence for a Theory
ISSN 0017-8748 Headache doi: 10.1111/head.13214 VC 2017 American Headache Society Published by Wiley Periodicals, Inc. Views and Perspectives The Migraine Attack as a Homeostatic, Neuroprotective Response to Brain Oxidative Stress: Preliminary Evidence for a Theory Jonathan M. Borkum, PhD Background.—Previous research has suggested that migraineurs show higher levels of oxidative stress (lipid peroxides) between migraine attacks and that migraine triggers may further increase brain oxidative stress. Oxidative stress is trans- duced into a neural signal by the TRPA1 ion channel on meningeal pain receptors, eliciting neurogenic inflammation, a key event in migraine. Thus, migraines may be a response to brain oxidative stress. Results.—In this article, a number of migraine components are considered: cortical spreading depression, platelet acti- vation, plasma protein extravasation, endothelial nitric oxide synthesis, and the release of serotonin, substance P, calcitonin gene-related peptide, and brain-derived neurotrophic factor. Evidence is presented from in vitro research and animal and human studies of ischemia suggesting that each component has neuroprotective functions, decreasing oxidant production, upregulating antioxidant enzymes, stimulating neurogenesis, preventing apoptosis, facilitating mitochondrial biogenesis, and/or releasing growth factors in the brain. Feedback loops between these components are described. Limitations and challenges to the model are discussed. Conclusions.—The theory is presented that migraines are an integrated -

Intramuscular Tramadol Vs. Diclofenac Sodium for The
J Headache Pain (2005) 6:143–148 DOI 10.1007/s10194-005-0169-y ORIGINAL Zulfi Engindeniz Intramuscular tramadol vs. diclofenac sodium Celaleddin Demircan Necdet Karli for the treatment of acute migraine attacks Erol Armagan in emergency department: a prospective, Mehtap Bulut Tayfun Aydin randomised, double-blind study Mehmet Zarifoglu Received: 6 February 2005 Abstract The aim of this prospec- injection in future visits. Any Accepted in revised form: 15 April 2005 tive, randomised, double-blind study adverse events, whether related to Published online: 13 May 2005 was to evaluate the efficacy of intra- the drug or not, were also recorded. muscular (IM) tramadol 100 mg in Patients were followed up by tele- emergency department treatment of phone 48 h later to check for any acute migraine attack and to com- headache recurrence. Two-hour pain pare it with that of IM diclofenac response rate, which was the prima- sodium 75 mg. Forty patients who ry endpoint, was 80% for both tra- were admitted to our emergency madol and diclofenac groups. There department with acute migraine were no statistically significant dif- attack according to the International ferences among groups in terms of Z. Engindeniz (౧) • E. Armagan • M. Bulut Headache Society criteria were 48-h pain response, rescue treat- T. Aydin Department of Emergency Medicine, included in the study. Patients were ment, associated symptoms’ Uludag University Medical Faculty, randomised to receive either tra- response, headache recurrence and Acil Tip ABD Gorukle, madol 100 mg (n=20) or diclofenac adverse event rates. Fifteen (75%) Bursa 16059, Turkey sodium 75 mg (n=20) intramuscular- patients in the tramadol group and e-mail: [email protected] ly. -
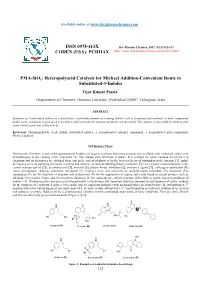
PMA-Sio2: Heteropolyacid Catalysis for Michael Addition-Convenient Route to Substituted-3-Indoles
Available online at www.derpharmachemica.com ISSN 0975-413X Der Pharma Chemica, 2017, 9(13):112-117 CODEN (USA): PCHHAX (http://www.derpharmachemica.com/archive.html) PMA-SiO2: Heteropolyacid Catalysis for Michael Addition-Convenient Route to Substituted-3-Indoles Vijay Kumar Pasala* Deapartment of Chemistry, Osmania University, Hyderabad-500007, Telangana, India ABSTRACT Synthesis of 3-substituted indoles in a hassel-free, ecofriendly manner by treating indoles with α, β-unsaturated carbonyl or nitro compounds under acidic conditions to give good to excellent yields with shorter reaction durations are described. The catalyst is recyclable for three to four times without great loss in the activity. Keywords: Phosphomolybdic Acid (PMA), Substituted indoles, α, β-unsaturated carbonyl compounds, α, β-unsaturated nitro compounds, Michael addition INTRODUCTION Heterocyclic chemistry is one of the quintessential branches of organic synthesis beaconing towards new scaffolds with medicinal values, new methodologies to the existing active principles etc. One among such skeletons is indole. It is perhaps the most common heterocycles in chemistry and its derivatives are obtained from coal pitch, variety of plants or by the bacterial decay of tryptophan in the intestine [1]. Indole derivatives serve as signaling chemicals in plants and animals, as nucleus building blocks (serotonin [2] (A) a crucial neurotransmitter in the central nervous system [3]), as antibacterial [4], antiviral [5], protein kinase inhibitors [6], anticancer agents [7], entheogens (psilocybin (B) causes perceptional changes), hormones (melatonin (C) regulates sleep and wakefulness), antidepressants (roxindole (D), bufotenin (E)), sumatriptan (F) for the treatment of migraine and ondansetron (G) for the suppression of nausea and vastly found in natural products such as alkaloids (Corynanthe, Iboga, and Aspidosperma alkaloids) [8-10], indigoids etc., which originate, either fully or partly, from bio-oxidation of indoles [11]. -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

The Serotonergic System in Migraine Andrea Rigamonti Domenico D’Amico Licia Grazzi Susanna Usai Gennaro Bussone
J Headache Pain (2001) 2:S43–S46 © Springer-Verlag 2001 MIGRAINE AND PATHOPHYSIOLOGY Massimo Leone The serotonergic system in migraine Andrea Rigamonti Domenico D’Amico Licia Grazzi Susanna Usai Gennaro Bussone Abstract Serotonin (5-HT) and induce migraine attacks. Moreover serotonin receptors play an impor- different pharmacological preventive tant role in migraine pathophysiolo- therapies (pizotifen, cyproheptadine gy. Changes in platelet 5-HT content and methysergide) are antagonist of are not casually related, but they the same receptor class. On the other may reflect similar changes at a neu- side the activation of 5-HT1B-1D ronal level. Seven different classes receptors (triptans and ergotamines) of serotoninergic receptors are induce a vasocostriction, a block of known, nevertheless only 5-HT2B-2C neurogenic inflammation and pain M. Leone • A. Rigamonti • D. D’Amico and 5HT1B-1D are related to migraine transmission. L. Grazzi • S. Usai • G. Bussone (౧) syndrome. Pharmacological evi- C. Besta National Neurological Institute, Via Celoria 11, I-20133 Milan, Italy dences suggest that migraine is due Key words Serotonin • Migraine • e-mail: [email protected] to an hypersensitivity of 5-HT2B-2C Triptans • m-Chlorophenylpiperazine • Tel.: +39-02-2394264 receptors. m-Chlorophenylpiperazine Pathogenesis Fax: +39-02-70638067 (mCPP), a 5-HT2B-2C agonist, may The 5-HT receptor family is distinguished from all other 5- Introduction 1 HT receptors by the absence of introns in the genes; in addi- tion all are inhibitors of adenylate cyclase [1]. Serotonin (5-HT) and serotonin receptors play an important The 5-HT1A receptor has a high selective affinity for 8- role in migraine pathophysiology. -

Triptans Step Therapy/Quantity Limit Criteria
Triptans Step Therapy/Quantity Limit Criteria Program may be implemented with the following options 1) step therapy 2) quantity limits or 3) step therapy with quantity limits For Blue Cross and Blue Shield of Illinois Option 1 (step therapy only) will apply. Brand Generic Dosage Form Amerge® naratriptan tablets Axert® almotriptan tablets Frova® frovatriptan tablets Imitrex® sumatriptan injection*, nasal spray, tablets* Maxalt® rizatriptan tablets Maxalt-MLT® rizatriptan tablets Relpax® eletriptan tablets Treximet™ sumatriptan and naproxen tablets Zomig® zolmitriptan tablets, nasal spray Zomig-ZMT® zolmitriptan tablets * generic available and included as target agent in quantity limit edit FDA APPROVED INDICATIONS1-7 The following information is taken from individual drug prescribing information and is provided here as background information only. Not all FDA-approved indications may be considered medically necessary. All criteria are found in the section “Prior Authorization Criteria for Approval.” Amerge® Tablets1, Axert® Tablets2, Frova® Tablets3,Imitrex® injection4, Imitrex Nasal Spray5, Imitrex Tablets6, Maxalt® Tablets7, Maxalt-MLT® Tablets7, Relpax® Tablets8, Treximet™ Tablets9, Zomig® Tablets10, Zomig-ZMT® Tablets10, and Zomig® Nasal Spray11 Amerge (naratriptan), Axert (almotriptan), Frova (frovatriptan), Imitrex (sumatriptan), Maxalt (rizatriptan), Maxalt-MLT (rizatriptan orally disintegrating), Relpax (eletriptan), Treximet (sumatriptan/naproxen), Zomig (zolmitriptan), and Zomig-ZMT (zolmitriptan orally disintegrating) tablets, and Imitrex (sumatriptan) and Zomig (zolmitriptan) nasal spray are all indicated for the acute treatment of migraine attacks with or without aura in adults. They are not intended for the prophylactic therapy of migraine or for use in the management of hemiplegic or basilar migraine. Safety and effectiveness of all of these products have not been established for cluster headache, which is present in an older, predominantly male population. -

European Patent Office of Opposition to That Patent, in Accordance with the Implementing Regulations
(19) TZZ _T (11) EP 2 666 772 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C07D 409/04 (2006.01) C07D 209/16 (2006.01) 01.03.2017 Bulletin 2017/09 C07D 209/18 (2006.01) C07D 209/38 (2006.01) (21) Application number: 13173141.6 (22) Date of filing: 12.12.2003 (54) Synthesis of amines and intermediates for the synthesis thereof Synthese von Aminen und Zwischenverbindungen für die Synthese davon Synthèse d’amines et intermédiaires pour leur synthèse (84) Designated Contracting States: • DEMERSON C A ET AL: "ETODOLIC ACID AND AT BE BG CH CY CZ DE DK EE ES FI FR GB GR RELATED COMPOUNDS CHEMISTRY AND HU IE IT LI LU MC NL PT RO SE SI SK TR ANTIINFLAMMATORY ACTIONS OF SOME POTENT DI-AND TRISUBSTITUTED (30) Priority: 20.12.2002 EP 02406128 1,3,4,9-TETRAHYDROPYRANO not 3,4-B 3/4 INDOLE-I-ACETIC ACIDS", JOURNAL OF (43) Date of publication of application: MEDICINALCHEMISTRY, AMERICAN CHEMICAL 27.11.2013 Bulletin 2013/48 SOCIETY, vol. 19, no. 3, 1 March 1976 (1976-03-01), pages391-395, XP000940626, ISSN: (62) Document number(s) of the earlier application(s) in 0022-2623, DOI: 10.1021/JM00225A010 accordance with Art. 76 EPC: • HARUYASU ET ALL: "Possible metabolic 03799560.2 / 1 572 647 Intermediatesfrom IAA to beta-acid in Rice Bran", AGR. BIOL. CHEM., vol. 40, no. 12, 1976, pages (73) Proprietor: BASF SE 2465-2470, XP002714693, 67056 Ludwigshafen am Rhein (DE) • SOLL R M ET AL: "Multigram preparation of 1,8-diethyl-7-hydroxy-1,3,4,9-tetrahydropy (72) Inventors: rano[3,4-b]indole-1-acetic acid, a phenolic • Berens, Ulrich metabolite of the analgesic and antiinflammatory 79589 Binzen (DE) agent etodolac", THE JOURNAL OF ORGANIC • Dosenbach, Oliver CHEMISTRY, AMERICAN CHEMICAL SOCIETY 79415 Bad Bellingen (DE) [NOT]ETC. -

5HT1 Receptor Agonists and Either a Cox-2 Inhibitor Or NSAID for the Treatment of Migraine
Europäisches Patentamt (19) European Patent Office Office européen des brevets (11) EP 1 051 993 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int. Cl.7: A61P 25/06, A61K 45/06 15.11.2000 Bulletin 2000/46 (21) Application number: 00303887.4 (22) Date of filing: 09.05.2000 (84) Designated Contracting States: (72) Inventor: Sands, George Harry AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU Goton, Connecticut 06340 (US) MC NL PT SE Designated Extension States: (74) Representative: AL LT LV MK RO SI Simpson, Alison Elizabeth Fraser et al Urquhart-Dykes & Lord, (30) Priority: 14.05.1999 US 134311 P 30 Welbeck Street London W1M 7PG (GB) (71) Applicant: Pfizer Products Inc. Groton, CT 06340-5146 (US) (54) 5HT1 receptor agonists and either a cox-2 inhibitor or NSAID for the treatment of migraine (57) The present invention relates to a method of treating migraine in a mammal, including a human, by administering to the mammal a 5HT1 receptor agonist in combination with either a cyclooxygenase-2 (COX-2) inhibitor or a nonsteroidal antiinflammatory drug (NSAID). It also relates to pharmaceutical compositions containing a pharmaceutically acceptable carrier, a 5HT1 receptor agonist with either a cyclooxygenase-2 (COX-2) inhibitor or a nonsteroidal antiinflammatory drug (NSAID). EP 1 051 993 A2 Printed by Xerox (UK) Business Services 2.16.7 (HRS)/3.6 EP 1 051 993 A2 Description [0001] The present invention relates to a method of treating migraine in a mammal, including a human, by admin- istering to the mammal a 5HT1 receptor agonist in combination with either a cyclooxygenase-2 (COX-2) inhibitor or a 5 nonsteroidal antiinflammatory drug (NSAID). -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Dihydroergotamine
Journal of Pre-Clinical and Clinical Research, 2018, Vol 12, No 4, 149-157 REVIEW PAPER www.jpccr.eu Dihydroergotamine (DHE) – Is there a place for its use? Agnieszka Piechal1, Kamilla Blecharz-Klin1, Dagmara Mirowska-Guzel1 1 Medical University of Warsaw, Poland Piechal A, Blecharz-Klin K, Mirowska-Guzel D. Dihydroergotamine (DHE) – Is there a place for its use? J Pre-Clin Clin Res. 2018; 12(4): 149–157. doi: 10.26444/jpccr/99878 Abstract Nowadays, dihydroergotamine (DHE) is sporadically used as a vasoconstrictor in the treatment of acute migraine. The importance of this drug in medicine has significantly decreased in the recent years. Limitations on the use of dihydroergotamine are due to the high toxicity and increased the risk of severe adverse events after prolonged theraphy. The Committee for Medicinal Products for Human Use of the European Medicines Agency recommends limiting the use of drugs that contain ergotamine derivatives due to the potential risk of ischemic vascular events, fibrosis and ergotism. However, ergot alcaloids preparations are not recommended for use in the prophylaxis of migraine pain, although it is still a good alternative for people with status migrainosus, migraine recurrence or chronic daily headache that do not respond to the classical theraphy. In clinical practice, DHE can be used as a rescue medication to treat migraine attacks involving aura or without aura, as well as for the acute treatment of cluster headache episodes. The effectiveness of DHE in alleviating migraine headache was assessed in multiple clinical studies. This review describes the pharmacodynamic and pharmacokinetic properties of DHE in an expanded view and its role in modern therapy based on available clinical trials.