COVID-19 International Research Update
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Official Transcript
Under the Microscope Expert Webinar on COVID-19 Vaccine Research in Australia & Germany Official Transcript On 30 June 2020, the Australian Embassy Berlin hosted an expert webinar to discuss the race for a COVID-19 vaccine. The event was was supported by the German Embassy Canberra, the Australian Academy of Science, and the Australia- Germany Research Network (AGRN). Ambassador H.E. Laureate Professor Professor Doctor Emeritus Professor Paul Richards Lynette Wood Peter Doherty Marylyn Addo Hans Bachor This live webinar took place on 30 June 2020, when the world had just crossed over 10 million infections and 500,000 deaths due to COVID-19. The date was on the eve of the six month mark since WHO received the first reports of a cluster of cases of pneumonia of unknown cause in China. Due to technical issues with the recording, we are not able to provide a high-quality audio or video recording of the webinar. Instead, we provide below a transcript of the webinar. We hope you find it useful and informative. 2 Panellists Laureate Professor Peter Doherty is one of Australia’s leading immunologists. Professor Doherty is the patron of the eponymous Doherty Institute, which has been at the forefront of Australia’s response to the COVID-19 pandemic. The Institute is currently investigating two protein-based and two viral vector vaccines. Professor Doherty and Swiss researcher Rolf Zinkernagel were awarded the Nobel Prize in Physiology or Medicine in 1996 for their discoveries of how the immune system recognises virus-infected cells, a discovery which has had practical implications for cancer treatments. -

German Center for Infection Research
GERMAN CENTER FOR INFECTION RESEARCH Annual Report 2018 Cover image: This image shows a scanning electron microscope image of thread-like Ebola viruses (in blue) protruding from an infected cell. ANNUAL REPORT 2018 The DZIF at a glance The German Center for Infection Research (DZIF) coordinates and oversees the strategic planning of translational infection research within Germany. Its mission is to translate results from basic biomedical research into clinical research. 35 DZIF research centres work concertedly against the global threat of infectious diseases. Table of contents Editorial ............................................................................................................................................................................. 3 About the DZIF ............................................................................................................................................................. 4 Science – Translation in focus Emerging Infections ................................................................................................................................................. 6 Tuberculosis ................................................................................................................................................................... 8 Malaria .............................................................................................................................................................................. 10 HIV ....................................................................................................................................................................................... -

Do Clades Matter for HIV Vaccines?
IAVI Report THE NEWSLETTER ON INTERNATIONAL AIDS VACCINE RESEARCH VOL 7/NUM 2 MAY–AUGUST 2003 Do Clades Matter for HIV Vaccines? As thousands of people prepare to gather in Nairobi and New York for September’s AIDS meetings, a key question for vaccine developers is how to contend with the huge diversity of HIV strains circulating worldwide BY PATRICIA KAHN is famously the most genetically diverse than anything the public health field has ever attempt- HIVviral pathogen known—nowhere more so ed. Doing it with many different formulations, or with than in Africa—as well as one of the most rapidly repeated updates, would be even more challenging. mutating. That, plus the uneven global distribution of Nailing down the impact of HIV diversity on vac- its nine genetic subtypes, or clades, poses one of the cine responses is difficult, for several reasons. One is biggest scientific unknowns facing AIDS vaccine devel- that the current system for classifying HIV diversity is opers: is a single, “universal” vaccine against all strains based on genetic sequence, not immune properties, possible? Or will it be necessary to make a slew of dif- and hasn’t been translated into distinct “immuno- ferent vaccine formulations, each tailored to the most types”—which is what really matters for vaccines. common strains in a given region? Even worse, could it While that task is slowly being tackled for epitopes tar- Inside: mean that new formulations might be needed regular- geting cellular immunity, it may be impossible for neu- ly, as with flu vaccines? tralizing antibodies (NAbs), where clades don’t seem to In Memoriam: The answer will be key to how quickly, and at correlate with immune recognition. -
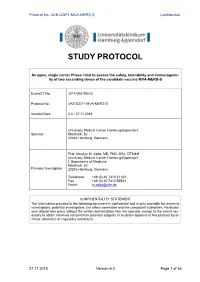
Study Protocol
Protocol No. UKE-DZIF1-MVA-MERS-S Confidential STUDY PROTOCOL An open, single center Phase I trial to assess the safety, tolerability and immunogenic- ity of two ascending doses of the candidate vaccine MVA-MERS-S EudraCT No. 2014-003195-23 Protocol No. UKE-DZIF1-MVA-MERS-S Version/Date 6.0 / 27.11.2018 University Medical Center Hamburg-Eppendorf Sponsor Martinistr. 52 20246 Hamburg, Germany Prof. Marylyn M. Addo, MD, PhD, MSc, DTM&H University Medical Center Hamburg-Eppendorf I. Department of Medicine Martinistr. 52 Principal Investigator 20246 Hamburg, Germany Telephone: +49 (0) 40 7410 51102 Fax: +49 (0) 40 7410 58531 Email: [email protected] CONFIDENTIALITY STATEMENT The information provided in the following document is confidential and is only available for review to investigators, potential investigators, the ethics committee and the competent authorities. No disclo- sure should take place without the written authorization from the sponsor, except to the extent nec- essary to obtain informed consent from potential subjects or to obtain approval of this protocol by an ethics committee or regulatory authorities. 27.11.2018 Version 6.0 Page 1 of 55 Protocol No. UKE-DZIF1-MVA-MERS-S Confidential Summary of Changes Summary of changes since last version of approved protocol (protocol version 3.0 to ver- sion 4.0) Amendment Number Date of Amend- Section Affected ment by Change 01 20DEC2017 2 Synopsis Brief description of change: The synopsis was updated according to the information given in the main body. 01 20DEC2017 6 Investigator and study administrative structure Brief description of change: Contact information was updated. -

COVID-19 International Research Update
COVID-19 International Research Update Compiled by: Assam Rural Infrastructure and Agricultural Services (ARIAS) Society ::::::::::::::::::::::::::::::::Team::::::::::::::::::::::::::::::::::: 1. LayaMadduri, IAS, State Project Director, ARIAS Society 2. ParijatChowdhury, Sr. ICT & Infra Specialist, ACCSDP 3. NibhaKumari, Agri Marketing Specialist, ASAMB-APART 4. Baljeet Singh, Market Analyst & Operations Specialist, APART March – April 2020 Page 1 of 43 Table of contents Sl Title Pg 1 WHO Director-General's opening remarks at the media briefing on COVID-19 04 2 UC Davis launches two clinical studies to treat COVID-19 04 3 USFDA update on COVID-19 05 4 Coronavirus: The woman behind India's first testing kit 05 5 Russian scientists take the first photo of a novel coronavirus and fully decode its genome 05 6 Russia plans to start series production of new vaccine against coronavirus in 1.5 years 05 7 Australian researchers to trial BCG vaccine for COVID-19 06 8 University of Birmingham joins COVID-19 genome sequencing alliance to map spread of coronavirus 07 9 University Of Glasgow Leads Covid-19 Research Response In Scotland 08 10 Germany : DZIF Coronavirus Researchers use “Fast Track” 09 11 WHO says early data show some drugs ‘may have an impact’ on coronavirus, but more research is 11 needed 12 USA: Study will test if hydroxychloroquine can prevent COVID-19 11 13 USA: Florida Research Company Prepares for COVID-19 Vaccine, Treatment Clinical Trials 11 14 Europe : Severe COVID-19 cases to be offered new clinical trial programme 12 15 USA -

The Transmitted HIV-1 Subtype C
The transmitted HIV-1 subtype C: Characterization of the transmitted/founder full-length virus genome and the influence of early immune selective pressure on virus replication Melissa-Rose Hilda Abrahams Univeristy of Cape Town Thesis Presented for the Degree of DOCTOR OF PHILOSOPHY in the Department of Clinical Laboratory Sciences UNIVERSITY OF CAPE TOWN October 2014 The copyright of this thesis vests in the author. No quotation from it or information derived from it is to be published without full acknowledgement of the source. The thesis is to be used for private study or non- commercial research purposes only. Published by the University of Cape Town (UCT) in terms of the non-exclusive license granted to UCT by the author. University of Cape Town Table of Contents Table of Contents ................................................................................................................... i Declaration ............................................................................................................................ iii Abstract................................................................................................................................. iv Acknowledgements ............................................................................................................... v List of Abbreviations .............................................................................................................. vi Chapter 1: Literature Review ............................................................................................. -

« Understanding Emerging Viral Diseases and Their Public Health Impact »
« Understanding Emerging Viral Diseases and their Public Health Impact » Organizers: Laurent Kaiser, Isabella Eckerle Geneva Centre for Emerging Viral Diseases, University Hospital Geneva & University Geneva Geneva, Switzerland Scientific Commitee: Marylyn Addo, Germany Amadou Sall, Senegal Olivier Engler, Switzerland Daniel Bausch, UK François Chappuis, Switzerland Antoine Flahault, Switzerland Claire-Anne Siegrist, Switzerland Volker Thiel, Switzerland Nahoko Shindo, Switzerland Pascal Cherpillod, Switzerland Noël Tordo, France/Guinea Gary Kobinger, Canada Venue: Campus Biotech, 9 Chemin des Mines, Geneva, Switzerland www.unige.ch/emerging-virus-symposium 1 Wednesday April 10, 2019 12.00 - 13.00 Registration 13.00 – 13.15 Laurent Kaiser Welcome and introduction Isabella Eckerle Geneva Centre for Emerging Viral Diseases, Geneva, Switzerland Session I: Arbovirus emergence in Europe 13.20 – 13.40 Jose Arribas Autochthonous CCHF transmission in Spain Hospital Universitario La Paz, Madrid, Spain (confirmed) 13.40 – 14.10 Tom Fletcher CCHF in Europe – Lessons from Turkey Liverpool School of Tropical Medicine, Liverpool, UK (confirmed) 14.10 – 14.30 Jonas Schmidt-Chanasit Mayaro, Usutu, West Nile - the next emerging Bernhard-Nocht-Institute arbovirus? Hamburg, Germany (confirmed) 14.30 – 15.00 Coffee Break Session II: Yellow Fever Virus – Old virus, new challenges 15.00 – 15.20 Annelies Zinkernagel Imported yellow fever case to Switzerland University Hospital Zurich, Switzerland (t.b.c.) 15.20 – 15.50 Ho Yeh-Li Severe yellow fever – clinical -

The Rare Few
22 WHAT are the oDDs? that you will never need drugs to keep your hiV in check? // that you will live longer than your doctor’s first prediction? his second? his third? // that you hold a vital clue to preventing, even curing, aiDs? The Rare Few by charles slack // PhotograPhs by gregory heisler t first Karen Pancheau figured her son whose samples showed they had been infected with HIV Tyler’s nasty rash came from friction on in the late 1970s; many had already died, but some weren’t A the mats at judo class. But when the rash even sick. Then, in 1994, Walker met a hemophiliac in Bos- began dissolving layers of flesh, his father ton named Bob Massie, who had become infected with HIV took the teenager for tests, which revealed through a blood transfusion in 1978—three years before he had HIV. Karen, too, tested positive AIDS was even identified as a disease. “People keep telling for HIV, the virus that causes AIDS, which she’d apparently me I’m going to die, and I keep living,” Massie told Walker. acquired from a blood transfusion in June 1982 and to which Walker immediately began to study his immune system. she exposed Tyler during childbirth and breast-feeding. Yet as A few years later, speaking before several hundred doctors Tyler slowly progressed to AIDS, Karen remained healthy. at an AIDS conference in New York City, Walker asked how Various drug cocktails kept AIDS from killing Tyler, but they many had run across similar patients. When at least half the left him constantly fatigued, and on Nov. -

German Center for Infection Research
GERMAN CENTER FOR INFECTION RESEARCH Annual Report 2017 Title image: This shows an electron microscope image of a cluster of rod-shaped tuberculosis bacteria visible in pink. ANNUAL REPORT 2017 The DZIF at a glance The German Center for Infection Research (DZIF) coordinates and oversees the strategic planning of translational infection research within Germany. Its mission is to translate results from basic biomedical research into clinical research. 35 DZIF research centres work concertedly against the global threat of infectious diseases. Table of contents Editorial ................................................................................................................................................. 3 About the DZIF ................................................................................................................................... 4 Science – Translation in focus Emerging Infections .......................................................................................................................... 6 Tuberculosis ......................................................................................................................................... 8 Malaria ................................................................................................................................................ 10 HIV ....................................................................................................................................................... 12 Hepatitis ............................................................................................................................................ -
MVA-SARS-2-S DZIF COVID-19 Vaccine Candidate
MVA-SARS-2-S DZIF COVID-19 vaccine candidate Marylyn M. Addo (UKE), Stephan Becker (UMR), Gerd Sutter (LMU), Andreas Neubert (IDT), Thomas Hesterkamp (PDU-DZIF) DZIF - Emerging Infections Epidemiology Public Health Virus ecology; diagnostics; Christian Drosten Outbreak surveillance Gerd Sutter DZIF infrastructures: − Clinical Trials Unit − Product Development Unit Virology TTU/TIXYZ Infection medicine − African Partner Institutions Vaccinology Clinical Trials BSL3/4 labs Marylyn Addo Antiviral Test platform Stephan Becker Portrait of vaccinia virus MVA Electron micrograph D. Spehner / G. Sutter TTU/TIXYZ Mayr & Munz Zentralbl Bakteriol Orig A 1964 Stickl et al. Dtsch Med Wochenschr 1974 MVA as vector for gene expression and vaccination • non-replicating virus in mammalian hosts, high level of biological safety • efficient production and delivery of heterologous antigens • experience with various vector vaccines in clinical testing TTU/TIXYZ Sutter & Moss, 1992, Sutter et al., 1994 MVA vectors as candidate vaccines Emerging viruses Allergies TTU/TIXYZ Persistent viruses Bacteria Parasites Tumors MVA-SARS-2-S: Design and preclinical testing • MVA platform technology based on MVA F6 LMU • Expression of full-length SARS-CoV-2 S gene sequence • Production of mature ~190 kDa spike glycoprotein • Genetic homogeneity, genetic identity, genetic stability • Full growth capacity in cell substrate for manufacturing TTU/TIXYZ • Immunizations in mice induce spike protein-specific antibodies and T cells • Protective efficacy in mice against SARS-CoV-2 -

LSN Magazine 2021 a Strong Response (PDF)
MEDTECH, BIOTECH & PHARMA | 2021 THE INDUSTRY JOURNAL OF HAMBURG & SCHLESWIG-HOLSTEIN DESTINATION DESY The DESY campus has developed into a go-to-hub for life science companies and is the nucleus of the new Science City MEDTECH AI ECOSYSTEM How the consortium KI-SIGS connects players from the North to bring artificial intelligence into clinical application A STRONG RESPONSE Life science players in the North of Germany make high impact contributions to combat the pandemic at many fronts 2 LSN MAGAZINE | LIFE SCIENCE NORD CLUSTER CLUSTER MEMBERS _> Please find our Gold and Silver members onpage 51. EDITORIAL | LSN MAGAZINE 3 Dear readers, surely some of you have missed the LSN magazine over the past year. We took some time to put our communication about the cluster and its stakeholders on a new foot- ing. We revamped our digital channels and worked on a new magazine to provide a better and more comprehensive look at the life science industry in northern Germany. From now on, the magazine will be published once a year. Hereby, we are very pleased to present you with our first issue here – with a re-design and with some fresh categories for content. What can you expect from our new-look magazine? DR. HINRICH HABECK MANAGING DIRECTOR Our main story focuses on COVID-19. We explore the broad spectrum of expertise LIFE SCIENCE NORD MANAGEMENT GMBH in the cluster and the variety of stakeholders working on solutions to help fight the pandemic – be it on new therapies, vaccines and diagnostics, or even masks and ven- tilators. -

Consultation on Potential Ebola Therapies and Vaccines 4-5 September 2014 Geneva, Starling Hotel
Consultation on potential Ebola therapies and vaccines 4‐5 September 2014 Geneva, Starling Hotel List of participants: 1. Dr Marylyn Addo, Professor of Emerging Infections, Universitätsklinikum Hamburg‐Eppendorf, German Center of Infectious Diseases Research (DZIF), Hamburg, Germany 2. Dr Clement Adebamowo, Chairman, National Health Research Ethics Committee of Nigeria, Federal Ministry of Health, Abuja, Nigeria 3. Dr Selidji Agnandji, Franceville, Gabon 4. Dr Enrica Alteri, Head of Safety and Efficacy of Medicines, Human Medicines Development and Evaluation Unit, European Medicines Agency, London, United Kingdom of Great Britain & Northern Ireland 5. Dr Sylvain Baize, Biology of Viral Emerging Infections, Institut Pasteur, Paris, France 6. Dr Younoussa Ballo, Secrétaire general, Ministère de la Santé, Conakry, Guinea 7. Dr Ripley Ballou, GlaxoSmithKline Biologicals SA, Rixensart, Belgium 8. Ms Helia Baradarani, Tekmira’s Manager of Medical Countermeasure Business Development, Vancouver, Canada 9. Dr Jarbas Barbosa, Vice Minister, Ministry of Health, Brasilia, Brazil 10. Dr Jesus Barral‐Guerin, Senior Manager, Vaccine Centre, Supply Division, UNICEF, Copenhagen, Denmark 11. Dr Daniel Bausch, Associate Professor, Department of Tropical Medicine, Tulane University School of Public Health and Tropical Medicine, New Orleans, USA 12. Dr Sina Bavari, CIV US Army Medcom USA MRIID, USA 13. Dr Stephan Becker, Direktor, Institut für Virologie, Marburg, Germany 14. Dr Laetitia Bigger, Senior Manager, Vaccines Policy, IFPMA, Geneva, Switzerland 15. Dr Fred Binka, Vice Chanceller, University of Health and Allied Sciences, Ho, Ghana 16. Dr Francisco Blanco, Chief of Medicines & Nutrition, Supply Division, UNICEF, Copenhagen, Denmark 17. Dr Luciana Borio, Director, Office of Counterterrorism and Emerging Threats (OCET) in the Office of the Chief Scientist, U.S.