Nail-Biting and Foreign Body Embedment: a Review and Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nail Anatomy and Physiology for the Clinician 1
Nail Anatomy and Physiology for the Clinician 1 The nails have several important uses, which are as they are produced and remain stored during easily appreciable when the nails are absent or growth. they lose their function. The most evident use of It is therefore important to know how the fi ngernails is to be an ornament of the hand, but healthy nail appears and how it is formed, in we must not underestimate other important func- order to detect signs of pathology and understand tions, such as the protective value of the nail plate their pathogenesis. against trauma to the underlying distal phalanx, its counterpressure effect to the pulp important for walking and for tactile sensation, the scratch- 1.1 Nail Anatomy ing function, and the importance of fi ngernails and Physiology for manipulation of small objects. The nails can also provide information about What we call “nail” is the nail plate, the fi nal part the person’s work, habits, and health status, as of the activity of 4 epithelia that proliferate and several well-known nail features are a clue to sys- differentiate in a specifi c manner, in order to form temic diseases. Abnormal nails due to biting or and protect a healthy nail plate [1 ]. The “nail onychotillomania give clues to the person’s emo- unit” (Fig. 1.1 ) is composed by: tional/psychiatric status. Nail samples are uti- • Nail matrix: responsible for nail plate production lized for forensic and toxicology analysis, as • Nail folds: responsible for protection of the several substances are deposited in the nail plate nail matrix Proximal nail fold Nail plate Fig. -

Body-Focused Repetitive Behaviour: the Influence of Alexithymia and Impulsivity
Body-Focused Repetitive Behaviour: The influence of Alexithymia and Impulsivity Bachelor thesis Faculty of Behavioural. Management, & Social Sciences Mirjam Römer 25th of June 2019 Supervisor: Dr. Matthijs L. Noordzij Second supervisor: Drs. Youri P.M.J. Derks Department of Positive Psychology and Technology (PPT) 2 BODY FOCUSED REPETITIVE BEHAVIOUR: THE INFLUENCE OF ALEXITHYMIA AND IMPULSIVITY 3 BODY FOCUSED REPETITIVE BEHAVIOUR: THE INFLUENCE OF ALEXITHYMIA AND IMPULSIVITY Abstract Body-Focused Repetitive Behaviours (BFRBs; e.g., hair pulling, nail biting, skin picking, mouth/cheek/lip biting) can cause significant physical and psychological distress which can lead to more severe engagement in self-harming behaviors. However, data examining BFRBs among non-clinical samples is limited. As BFRBs seem to be connected to impulsivity and alexithymia, the inability to detect one’s own emotions, this study investigates the extent to which the engagement and the urge to engage in BFRBs is associated with both impulsivity and alexithymia in a non-clinical sample (N=106). The study aimed to find an answer to whether there is a moderation effect of alexithymia on the relationship between impulsivity and BFRB. The focus of this study lied on the influence on the urge, and the engagement in BFRBs, thus two models were tested. An interaction effect between impulsivity and alexithymia was assumed, as both seem to influence the engagement in BFRBs positively. The data were gathered through an online survey, including questionnaires regarding alexithymia (TAS-20), impulsivity (BIS-15 (11)) and BFRBs (adapted form of MGH-HS). For both models, one considering only the urge for BFRBs and the other one the actual engagement in BFRB did not show a significant interaction effect (b=.17, t(103)=.43, p=.67; b=.00, t(103)=.037, p=.71). -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Pedicure: Nail Enhancements
All Hair Services Include Shampoo All Services Based on Student Availability Long Hair is Extra & Senior Price Available Hair Cuts: Color: (Does Not Include Cut & Style) Hair Cut (Hood dryer) $6.50 Retouch/Tint/PM Shine $14.50 With Blowdry $13.50 Additional Application $8.00 With Blowdry & Flat Iron $21.50 Color (All over color) $20.00 Foils Each $4.00 Hair Styles: Hair Length to Collar $38.00 Shampoo/Set $6.75 Hair Length to Shoulder $48.00 Spiral Rod Set $20.00 Hair Length past Shoulder $58.00 Shampoo/ Blowdry $9.00 Frosting with Cap $17.50 With Thermal Iron $13.00 Men’s Comb Highlight with Cut $15.00 With Flat Iron $15.00 With Press & Curl $18.00 Perms & Relaxers: (Includes Cut & Style) Wrap Only $6.50 Regular or Normal Hair $20.95 Wrap with Roller Set $10.50 Resistant or Tinted Hair $26.00 Fingerwaves with Style $17.50 Spiral or Piggyback $36.00 Twists $3.00 Relaxer $35.00 Straight Back $20.00 Curled $15.00 Other Hair Services: Spiral $20.00 Shampoo Only $2.00 French Braids with Blowdry $15.00 Line-up $3.00 Under 10 Braids $20.00 Deep Condition $5.00 Over 10 Braids $25.00 Keratin Treatment $15.00 Braid Removal $15.00 Updo or French Roll $20.00 Manicure: Spa Manicure $9.50 Waxing: French Manicure $8.00 Brow $6.00 Manicure $6.42 Lip $5.00 Chin $5.00 Pedicure: Full Face $15.00 Spa Pedicure $20.00 Half Leg $15.00 French Pedicure $17.00 Full Leg $30.00 Pedicure $15.00 Underarm $15.00 Half Arm $10.00 Nail Enhancements: Full Arm $15.00 Shellac (French $2) $15.00 Mid Back & Up $15.00 Overlay (Natural Nail) $12.00 Full Back $25.00 Acrylic Full Set $16.50 Bikini $25.00 Gel Full Set $18.00 Fill-in Gel & Acrylic $12.00 Massages: Nail Repair( Per Nail) $2.00 Relaxation $15.00 Soak Off $3.00 Deep Tissue $19.95 Nail Art (Per Nail) $1.00 Other Nail Services: Nails & Waxing Services Taxable Polish Change $4.00 Nails Clipped $5.00 Paraffin Dip Wax $5.00 . -
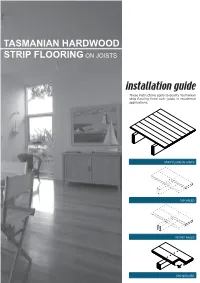
Tasmanian Hardwood Strip Flooring on Joists Guide for Installing
TASMANIAN HARDWOOD STRIP FLOORING ON JOISTS installation guide These instructions apply to quality Tasmanian strip flooring fixed over joists in residential applications. STRIP FLOOR ON JOISTS TOP NAILED SECRET NAILED END MATCHED TOOLS Simple tools are adequate in most applications. Necessary tools are: Tool Requirement Checklist Pencil, tape measure and square Hammer, punch and nail bag Stringline, spirit level and straight edge Hand saw and jig saw Safety glasses, dust mask and knee pads Spacers (about 100mm long and 2 mm thick) Rubber mallet, broom and vacuum cleaner Framing chisel For specialist applications, a drop saw, an air power staple gun, a power actuated fastener system and a cramping system may be useful. MATERIALS Use quality boards of the correct thickness. Grade descriptions for strip flooring are set out in the Australian Standard AS 2796 and are available at: www.tastimber.tas.gov.au. Boards at least 19 mm thick are needed to span 450 mm. Board width - Only secret nail boards up to 85 mm cover width. Secret nailed flooring is fixed through the tongue of specially profiled boards. Since they are only secured with one fastener per joist or batten, their width is limited to 85 mm cover. Board over 85 cover must be top nailed with two fasteners per joist. Use the correct nails for the job. The nail sizes required by Australian Standard 1684 are: Nail sizes for T & G flooring to joists* Nail sizes for T & G flooring to plywood substrate* Nailing Softwood Hardware & Strip flooring Rec. nailing (min.15mm substrate) joists cypress joists thicknes (mm) Hand 65 x 2.8 mm 50 x 2.8 mm 38 x 16 guage chisel point staples or driven bullet head bullet head 19 or 20 38 x 2.2 mm nails at 300mm spacing 32 x 16 guage chisel point staples or Machine 12,19 or 20 driven 65 x 2.5 mm 50 x 2.5 mm 30 x 2.2 mm nails at 200mm spacing *Alternative fasteners can be used for substrates types not listed subject to manufacturers’ recommendation. -

Regional Handwashing Policy
SOUTHERN CALIFORNIA GRADUATE MEDICAL EDUCATION POLICY AND PROCEDURE POLICY INFECTION PREVENTION AND CONTROL POLICIES EFFECTIVE DATE: SECTION: AND PROCEDURES 7/1/2014 TITLE: Hand Health & Hygiene Page: 1 of 8 BACKGROUND Studies have shown that handwashing causes a reduction in the carriage of potential pathogens on the hands. Microorganisms proliferate on the hands within the moist environment of gloves. Handwashing results in the reduction of patient morbidity and mortality from health care associated infections. The Centers for Disease Control and Prevention states that handwashing is the single most important procedure for preventing health-care associated infections. Artificial nails are more likely than natural nails to harbor pathogens that can lead to health care associated infections. There are four types of hand washing (see body of policy for detailed instructions): TYPE PURPOSE METHOD Routine Handwashing To remove soil and transient Wash hands with soap and microorganisms. water for at least 15 seconds. Hand antisepsis To remove soil and remove or Wash hands with antimicrobial destroy transient soap and water for at least 15 microorganisms. seconds. Hand rub/degerming To destroy transient and Rub alcohol-based hand resident microorganisms on degermer into hands vigorously UNSOILED hands. until dry. Surgical hand scrub To remove or destroy transient Wash hands and forearms with microorganisms and reduce antimicrobial soap and water resident flora. with brush to achieve friction. Or alcohol-based preparation rubbed vigorously -

White Nail As a Static Physical Finding: Revitalization of Physical Examination
Case Report White Nail as a Static Physical Finding: Revitalization of Physical Examination Ryuichi Ohta 1,* and Chiaki Sano 2 1 Community Care, Unnan City Hospital, 699-1221 96-1 Iida, Daito-cho, Unnan 699-1221, Shimane Prefecture, Japan 2 Department of Community Medicine Management, Faculty of Medicine, Shimane University, 89-1 Enya cho, Izumo 693-8501, Shimane Prefecture, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-9050605330 Abstract: Physical examinations are critical for diagnosis and should be differentiated into static and dynamic categories. One of the static findings is white nail, such as Terry’s and Lindsay’s nails. Here, we report the cases of two older patients with acute diseases who had nail changes that aided evaluation of their clinical course. Two elderly women who presented with acute conditions were initially thought to have normal serum albumin levels. They were found to have white nail with differences in nail involvement of the first finger, which subsequently revealed their hypoalbuminemia. The clinical courses were different following the distribution of nail whitening. Our findings show that examination of a white nail could indicate the previous clinical status more clearly than laboratory data. It can be useful for evaluating preclinical conditions in patients with acute diseases. Further evaluation is needed to establish the relationship between clinical outcomes and the presence of white nail in acute conditions among older patients. Citation: Ohta, R.; Sano, C. White Keywords: Lindsay’s nail; nail findings; nutritional assessment; physical examination; Terry’s nail; Nail as a Static Physical Finding: white nail Revitalization of Physical Examination. -

The ICD-10 Classification of Mental and Behavioural Disorders : Clinical Descriptions and Diagnostic Guidelines
ICD-10 ThelCD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines | World Health Organization I Geneva I 1992 Reprinted 1993, 1994, 1995, 1998, 2000, 2002, 2004 WHO Library Cataloguing in Publication Data The ICD-10 classification of mental and behavioural disorders : clinical descriptions and diagnostic guidelines. 1.Mental disorders — classification 2.Mental disorders — diagnosis ISBN 92 4 154422 8 (NLM Classification: WM 15) © World Health Organization 1992 All rights reserved. Publications of the World Health Organization can be obtained from Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications — whether for sale or for noncommercial distribution — should be addressed to Publications, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Coping with Self-Injury
COPING WITH SELF-INJURY Stephanie Larsen, Psy.D. Clinical Psychologist Palm Beach Behavioral health & wellness DISCLOSURE STATEMENT There is no conflict of interest or commercial support for this presentation. LEARNING OBJECTIVES To be able to identify types of self-injury To understand common reasons for onset of self-injurious behaviors To understand how self-injury is perceived by the injurer as helpful To be able to differentiate between self-injury and suicide attempts To identify potential ways of treating self-injurious behaviors NON-SUICIDAL SELF INJURY (NSSI) Non‐suicidal self‐injury (NSSI) has been defined as the deliberate, self‐inflicted destruction of body tissue without suicidal intent and for purposes not socially sanctioned (ISSS, 2007) DSM-5 SECTION 3: EMERGING MEASURES & MODELS (AREAS OF FURTHER STUDY) (A) In the last year, the individual has, on 5 or more days, engaged in intentional self-inflicted damage to the surface of his or her body, of a sort likely to induce bleeding or bruising or pain for purposes not socially sanctioned (e.g., body piercing, tattooing, etc.), but performed with the expectation that the injury will lead to only minor or moderate physical harm. The behavior is not a common one, such as picking at a scab or nail biting. (B)The intentional injury is associated with at least 2 of the following: (1)psychological precipitant: interpersonal difficulties or negative feelings or thoughts, such as depression, anxiety, tension, anger, generalized distress, or self-criticism, occurring in the period -

Pretty Scary 2 Unmasking Toxic Chemicals in Kids’ Makeup
Prevention October 2016 Starts Here Campaign for Safe Cosmetics Pretty Scary 2 Unmasking toxic chemicals in kids’ makeup breastcancerfund.org 1 Acknowledgements Developed and published by the Breast Cancer Fund and spearheaded by their Campaign for Safe Cosmetics, this report was written by Connie Engel, Ph.D.; Janet Nudelman, MA; Sharima Rasanayagam, Ph.D.; Maija Witte, MPH; and Katie Palmer. Editing, messaging and vision were contributed by Denise Halloran and Erika Wilhelm. Sara Schmidt, MPH, MSW, coordinated the purchasing of products reviewed in this report and worked closely with partners to share the message. Thank you to James Consolantis, our contributing content specialist and Rindal&Co for design direction. WE ARE GRATEFUL FOR THE GENEROUS CONTRIBUTIONS FROM OUR FUNDERS: As You Sow Foundation, Jacob and Hilda Blaustein Foundation, Lisa and Douglas Goldman Foundation, Park Foundation, Passport Foundation, and the Serena Foundation. breastcancerfund.org 2 Our partners in purchasing products Pam Miller, Alaska Community Action on Toxics, Alaska Brooke Sarmiento, BEE-OCH Organics, Colorado Sara Schmidt, Breast Cancer Fund, California Susan Eastwood, Clean Water Action, Connecticut Anne Hulick, Clean Water Action, Connecticut Johnathan Berard, Clean Water Action, Rhode Island Lauren Carson, Clean Water Action, Rhode Island Cindy Luppi, Clean Water Action, Massachusetts Kadineyse Ramize Peña, Clean Water Action, Massachusetts Elizabeth Saunders, Clean Water Action, Massachusetts Sara Lamond, Fig & Flower, Georgia Beverly Johnson, -

Management of Ingested Foreign Bodies in Children: a Clinical Report of the NASPGHAN Endoscopy Committee
COMMITTEE COMMENTARY Management of Ingested Foreign Bodies in Children: A Clinical Report of the NASPGHAN Endoscopy Committee ÃRobert E. Kramer, yDiana G. Lerner, zTom Lin, §Michael Manfredi, jjManoj Shah, ôThomas C. Stephen, #Troy E. Gibbons, ÃÃHarpreet Pall, yyBen Sahn, zzMark McOmber, §§George Zacur, ÃJoel Friedlander, jjjjAntonio J. Quiros, ôôDouglas S. Fishman, and ##Petar Mamula ABSTRACT ingestion. Furthermore, changes in the types of ingestions encountered, Foreign body ingestions in children are some of the most challenging clinical specifically button batteries and high-powered magnet ingestions, create scenarios facing pediatric gastroenterologists. Determining the indications an even greater potential for severe morbidity and mortality among and timing for intervention requires assessment of patient size, type of object children. As a result, clinical guidelines regarding management of these ingested, location, clinical symptoms, time since ingestion, and myriad other ingestions in children remain varied and sporadic, with little in the way of factors. Often the easiest and least anxiety-producing decision is the one to prospective data to guide their development. An expert panel of pediatric proceed to endoscopic removal, instead of observation alone. Because of endoscopists was convened and produced the present article that outlines variability in pediatric patient size, there are less firm guidelines available to practical clinical approaches to the pediatric patient with a variety of determine which type of object will safely pass, as opposed to the clearer foreign body ingestions. This guideline is intended as an educational tool guidelines in the adult population. In addition, the imprecise nature of the that may help inform pediatric endoscopists in managing foreign body ingestions in children. -

Onychophagia and Onychotillomania: Prevalence, Clinical Picture and Comorbidities
Acta Derm Venereol 2014; 94: 67–71 CLINICAL REPORT Onychophagia and Onychotillomania: Prevalence, Clinical Picture and Comorbidities Przemysław PACAN1, Magdalena GRZESIAK1, Adam REICH2, Monika Kantorska-JANIEC1 and Jacek C. Szepietowski2 1Department of Psychiatry, and 2Department of Dermatology, Venereology and Allergology, Wroclaw Medical University, Wroclaw, Poland Onychophagia is defined as chronic nail biting behaviour, younger than 3–6 years (8, 9). By the age of 18 years the which usually starts during childhood. Onychotilloma- frequency of this behaviour again decreases; however, nia results from recurrent picking and manicuring of the it may persist into adulthood in some subjects (8, 10). fingernails and/or toenails, leading to visual shortening According to the International Classification of Di- and/or estraction of nails. The aim of this study was to seases and Health Related Problems – 10th Revision assess the prevalence of onychophagia and onychotillo- (ICD-10), nail biting is classified as other specified mania in young adults, and the comorbidity of these con- behavioural and emotional disorders with onset usu- ditions with anxiety disorders and obsessive compulsive ally occurring in childhood and adolescence (F98.8), disorders (OCD), as well as to determine factors related together with excessive masturbation, nose picking, and to these behaviours. A total of 339 individuals were inter- thumb sucking (11). Diagnostic criteria have not been viewed with a structured questionnaire. Onychophagia well described for this group of disorders. was present in 46.9% of participants (including 19.2% Onychophagia seems to be a variant of compulsion, active and 27.7% past nail biters), and an additional 3 which may lead to destruction of the fingernails.