Sue Ryder Sue Ryder - the Chantry Inspection Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

No.08 May 2018 Members Blog Upcoming Meetings and Events PPG Network Meeting: Putting People Firmly at the Centre of Decision
No.08 May 2018 Welcome to “PPG News”. A monthly newsletter to update you on work at the CCG and to provide the opportunity for PPG’s to share their news and successes in our PPG “members blog” section. Introducing Zoe…. Members Blog Zoe Knight (pictured) is our new Social Sue West, Chair, The Birches PPG, Prescribing and Partnerships Manager. Zoe has Kesgrave joined the CCG having spent 14 years working in The PPG at the Birches Medical the educational sector in a pastoral role for a local Centre, Kesgrave organised a Health secondary school and further education college. Fair, which was held on 10 April at the Previously, Zoe was employed in community local Kesgrave Community Centre. participation roles for a district council and a Twenty-eight local organisations and social housing provider and developed training services were invited to attend with opportunities for volunteers and organisations in their appropriate stands displaying the voluntary sector. information and One Life Suffolk was Having completed many volunteer roles herself, on hand offering personal health from Community Service Volunteering to being a checks. There were representatives of member of the Mayor’s Charity Committee, Zoe is passionate about various organisations providing volunteering and is looking forward to meeting and working with PPGs and services for the elderly, transport, data hearing views and ideas for service engagement, delivery and management, mental health and improvement. sports facilities. The event was open In her spare time, Zoe is a keen racket sports player and enjoys playing to any resident of Kesgrave and tennis, squash and racket ball for local teams and spending time on her surrounding area, not just patients of allotment. -

Wildlife Rangers
Megabashers in full swing – see page 19 © Lydia Woods © Lydia January - April 2019 A news and events Produced by the diary from wildlife and conservation groups in the Ipswich area Skulduggery in the park SnippetsThis ‘skull’ was discovered by Yvonne Westley among autumn leaves in Holywells Park. Yvonne, a member of the Friends of Holywells Park, was with the weekly work party group based in the orchard when she made the discovery. Closer inspection of the find revealed that it was not a human skull after all but in fact, a Parasol mushroom that had been partly chewed, probably by mice. It’s not only mice who enjoy Parasols, they are delicious fried in butter and served on toast - the mushrooms not the mice! The Friends meet in the Leaf-yard at 10am every Wednesday, then make their way to the Holywells Orchard to carry out conservation tasks. Over the winter months, this will include coppicing, pruning and building dead hedges. An Owl Box to remember Lucky little hog Martin Cant of Ipswich Wildlife Group has David Dowding responded to an unusual request to build At the end of October I was alerted by one an owl box. of the Ipswich Borough Council gardeners to a small hedgehog he had seen in the toilets on Bourne Park, so went to have a look. The box is to serve as a memorial in remembrance of a regular visitor to Chantry Park. After consultation with the people concerned, Martin built a Tawny Owl box and attached a memorial plate to it. The box was installed by an Ipswich Borough Council parks team and can now be seen high up in an oak close to the Sue Ryder Home. -

Ed: It All Started with the Angle!See Page 10
BRINGING YOU ALL THE LATEST NEWS ABOUT YOUR COUNCIL | WWW.IPSWICH.GOV.UK | JUNE 2019 PICTURE BY JEN O’NEIL ED: IT ALL STARTED IT’S ALL SMILES AT THE SWITCH-ON WITH THE ANGLE! SEE PAGE 10 Peace of mind for you and your family - 24 hours a day Home Emergency Alarm Response Service Our 24-hour monitoring and responding service, covering Ipswich and surrounding towns and villages, helps you feel safe, reassured and 01473 433236 independent in your own home. www.hearsalarm.co.uk ALEXANDRA PARK IPSWICH IP4 1NY BSCENTRE PRESENTS... SUNDAY 1st SEPTEMBER 2019 12.00 - 6.00pm WORLD MUSIC & FOOD • INFORMATION STALLS • SPORTS CHILDREN’S ENTERTAINMENT • FAIRGROUND RIDES FREE • FUN FOR ALL THE FAMILY • ENTRY www.bscsuffolk.org.uk CONTACTS The Angle is published by Ipswich Borough Council and delivered to households in Ipswich. It is also published in the Ipswich Star and is available online at www.ipswich.gov.uk Contact Angle: [email protected] 01473 432031 Want to get in touch with a Councillor? Find out their details at www.ipswich.gov.uk/councillors Angle 2 GREAT MUSICALS COMING TO REGENT THEATRE Musical lovers of all ages will appreciate followed by the glorious revival of the drama, sounds and spectacle of Tim Annie, starring Lesley Joseph for a Rice and Andrew Lloyd Webber’s week-long run in November. Joseph and the Amazing Technicolour Dreamcoat. This stars Union J’s Jaymi Consider yourself at home at the Regent Hensley as Joseph in a show the Sunday Theatre – the fabulous Lionel Bart Times describes as “Brilliant! It explodes musical Oliver is coming to Ipswich from th th like glittering fireworks”. -
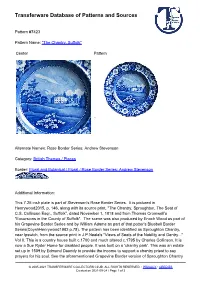
Transferware Database of Patterns and Sources
Transferware Database of Patterns and Sources Pattern #7423 Pattern Name: "The Chantry, Suffolk" Center Pattern Alternate Names: Rose Border Series: Andrew Stevenson Category: British Themes / Places Border: Floral and Botanical / Floral / Rose Border Series: Andrew Stevenson Additional Information: This 7.25 inch plate is part of Stevenson's Rose Border Series. It is pictured in Henrywood2015, p. 146, along with its source print, "The Chantry, Sproughton, The Seat of C.S. Collinson Esqr., Suffolk", dated November 1, 1818 and from Thomas Cromwell's "Excursions in the County of Suffolk". The scene was also produced by Enoch Wood as part of his Grapevine Border Series and by William Adams as part of that potter's Bluebell Border Series(CoyshHenrywood1982 p.78). The pattern has been identified as Sproughton Chantry, near Ipswich, from the source print in J.P.Neale's "Views of Seats of the Nobility and Gentry..." Vol II. This is a country house built c.1700 and much altered c.1795 by Charles Collinson. It is now a Sue Ryder Home for disabled people. It was built on a 'chantry park'. This was an estate set up in 1509 by Edmund Daundy to provide the income to support a chantry priest to say prayers for his soul. See the aforementioned Grapevine Border version of Sproughton Chantry © 2005-2021 TRANSFERWARE COLLECTORS CLUB. ALL RIGHTS RESERVED. • PRIVACY • CREDITS Created on 2021-09-24 / Page 1 of 2 Transferware Database of Patterns and Sources in the database, as well as another example by an unknown maker, for more information. Body Type: Earthenware Color: Blue Maker: Andrew Stevenson 1810–1827 Cobridge Staffordshire References: The Dictionary of Blue and White Printed Pottery 1780-1880 Vol. -

Ctc Suffolk Rides Types
CTC SUFFOLK RIDES TYPES SUNDAY RIDES - Co-ordinator: Michael Scott on 01473 613311 All rides start at 09:30 from St Margarets Green Ipswich and led by an experienced CTC member. Food & Drink- It is advisable to carry a drink and a packed lunch as food is not always assured at lunch stops. All attendees are required to have cycles in sound mechanical condition and carry a spare tube and means to fit it. Mudguards with rear mud flaps during the winter is respectfully preferred. PU - Pick-Up Points:(The time is a guide, based on a 9:30 start). A - St. Augustines Church, 9:45 B - Bourne Bridge, 9.40 Br - Bramford Picnic Site, 9:50 C - Hadleigh Rd, Chantry Park entrance 9:40 S - Sproughton Wild Man, 9:45 W - Washbrook, Bus stop,top of old A12 (NGR 115415). Wh - Whitton Church Lane, junction with Old Norwich Road, 9.45. Trr- Tuddenham road roundabout,9:35 GRADES E (Easy) Our most popular group rides. These are undertaken as a group at a leisurely pace and are rides suited to newcomers or members returning to cycling after long absence. Speed is typically 10 - 12 mph average, over distances between 40 - 50 miles. Refreshment stops are planned at roughly 15 mile intervals for morning coffee (11's), lunch and, during BST, afternoon tea. Routes are almost invariably over the country lane network avoiding main roads in order to explore the heart of our Suffolk countryside. Picnic lunches are popular during the Spring & Summer. It is common for some attendees to come along for just the morning only, or join us at 11's. -

Written Evidence Submitted by UK Music
Written evidence submitted by UK Music May 2021 DCMS Select Committee Submission Major Sport and Cultural Events 1.0 Introduction 1.1UK Music is the umbrella body representing the collective interests of the UK’s music industry, from songwriters and composers to artists and musicians, studio producers, professional recording studios, music managers, music publishers, major and independent record labels, music licensing companies and the live music sector. UK Music exists to represent the UK’s music sector, to drive economic growth and promote the benefits of music to British society (see the Annex for a full list of members). 1.2Live music events play a vital role in the life of the United Kingdom. A three- person band playing the Ironworks music venue in Inverness and Adele headlining Glastonbury in Somerset are performing the same role in a communal ritual that is known to everyone in the United Kingdom (UK). This shared moment can bring a room of complete strangers together, captivate a fractured nation or showcase life in the UK to the entire world. 1.3The ecology of musicians, creative freelancers and businesses who make this common experience possible not only power growth at a macro level but also nourish communities and businesses across the entire UK. 1.4This will lay out how live music events can: - Boost the UK economy. - Support the “levelling up” agenda. - Bring the UK together. - Promote the UK to the world. 1.5 To support this activity a number of policy steps should be taken: 1. Extension of 5% VAT level for culture tickets to the end of the 2021/22 financial year. -

HGGIS Vision Projects Spreadsheet Final Reva
Figure 23 - Haven Gateway Green Infrastructure Strategy - Schedule of Opportunities To be read in conjunction with Opportunities Map d s t lea p itie ( wn ortun no Conce p k p e ) o oject s ld r y of GI e Number ap le wher o p r c on t b G deficiency? ote m Ti N tegic access links? ics in A a live N h ners rt ost of a C Referen to de educes oves str R r y to grap enefit e mp K otential p I B P Contributes to creation of key potential Green corridor linking Saxmundham to Westleton, via Theberton Woods. Where possible to relate to existing 1 Saxmundham to Westleton Green Corridor SCC AO ££ green corridor * public RoW. Negotiation required to create new sections of access Links existing and proposed ANG Reinforces strategic promoted walk 2 Sizewell Belts to Aldringham Green Corridor SWT/SCHU £ Enhancement of Promoted Strategic Walk to link habitats along existing RoW * Connects existing ANG Reinforces strategic promoted walk 3 North Warren to River Alde Green Corridor SCHU £ Green corridor to link habitats. No additional access proposed * Connects existing ANG Access upgrade and extension, to include: Reinforces and extends route of strategic - upgrade of Sailor's Path (Strategic Promoted Walk) SCC/EA/SCH promoted walk 4 Snape to Slaughdon Green Corridor ££ - negotiation to create new link U * Links existing and proposed access - upgrade of existing RoW along seawall, around Aldeburgh Marshes Develop cycle access Possible 50% funding from WIRED Interreg bid Proposal developed by SCHU. Potential for funding from MSF Corp Regen Fund (SCC), -
Green Infrastructure Strategy for the Haven Gateway 2008
A Green Infrastructure Study for the Haven Gateway April 2008 thelandscapepartnership Quality control Green Infrastructure Strategy for Haven Gateway Sub-region Checked by Project Manager: Approved by: Signature: Signature: Name: Name: Title: Title: Date: Date: The Landscape Partnership is registered with the Landscape Institute, the Royal Town Planning Institute, and is a member of the Institute of Environmental Management and Assessment The Landscape Partnership Registered offi ce Greenwood House 15a St Cuthberts Street Bedford MK40 3JB Registered in England No. 2709001 Contents Figures Figure 1 Location of Haven Gateway Figure 2 Rivers and EA fl ood zones Executive summary Page i Figure 3 Agricultural land classifi cation 1 Introduction Page 1 Figure 4 Countryside character 2 Vision and Principles Page 3 Figure 5 BAP habitats, designated biodiversity sites and landscape designations 3 Approach to the study Page 5 Figure 6 Essex historic landscape character 4 The Green Infrastructure Plan Page 13 Figure 7 Suffolk historic landscape character 5 Steps to delivery and further actions Page 17 Figure 8 Conservation Areas, Scheduled Ancient Monuments, Registered Parks and Gardens. Figure 9 Existing accessible natural greenspace (ANG) Figure 10 Key resources contributing to ANG Figure 11 Access: strategic links and promoted routes Figure 12 Population density and directions of strategic growth Appendices (available at www.haven-gateway.org ) Figure 13 Existing ANG – Neighbourhood Level Appendix 1 Policy context Figure 14 Existing ANG – District -

[email protected] Mr Tom Barker Assistant Dire
Our ref: Your ref: Please ask for: Martyn Fulcher Direct dial: Grafton House Email: [email protected] 15-17 Russell Road Ipswich Suffolk Mr Tom Barker IP1 2DE Assistant Director Sustainable Communities Babergh and Mid Suffolk District Councils www.ipswich.gov.uk By email: [email protected] 25th March 2021 RE: Babergh and Mid Suffolk pre-submission Joint Local Plan (Regulation 19) consultation I write with reference to our formal submission to you on 24th December 2021, and specifically to clarify our position on the duty to cooperate. It has been drawn to my attention that despite the content of our submission, we incorrectly completed Part B, Section 4 point 3 of the Paper Representations Form. I can confirm that Ipswich Borough Council raises no objection in relation to the ‘duty to cooperate’, and that all representations made within our formal response relate to ‘soundness’ matters, namely: i) Lack of Strategic Ipswich Strategic Planning Area policies within the plan - Object to soundness of the Joint Local Plan. ii) Lack of Strategic Ipswich Strategic Planning Area policies within the plan - Object to soundness of the Joint Local Plan. iii) The approach to the spatial strategy for development including approx. 30% of new housing at the Ipswich Fringe has not been identified with the appropriate weight as part of the vision and objectives - Object to soundness of the Joint Local Plan. iv) Greater emphasis on the importance of Felixstowe and Ipswich as main employment hubs and service providers in the spatial strategy of the plan - Object to soundness of the Joint Local Plan. -

January 2018 Dear Kate Welcome to the Latest Edition of the Suffolk Information Partnership Warm Handover Quarterly Newsletter
January 2018 Dear Kate Welcome to the latest edition of the Suffolk Information Partnership Warm Handover quarterly newsletter. Here you will find updates from the Warm Handover partner organisations, details of new organisations that have joined the referral form and changes to the form that you need to be aware of. Please pass on to your teams and colleagues and anyone who may find it interesting. Update on the online referral form 2017 was a very busy year for warm handover referrals. Nine new partners joined the scheme, making a total of nineteen organisations you can refer your customers to for further support and advice. The new partners are: • Disability Advice Service, East Suffolk • Fire Prevention, Suffolk Fire and Rescue Service • Ipswich Citizens Advice • Local Area Coordinators • Lofty Heights • Survivors in Transition • Total Voice Suffolk • Trading Standards • Warm Homes Healthy People If you are not aware of any of these organisations you can find out what services they offer, and how they can support your customers, on the Gliffy (What partners do and don't do). This year we look forward to welcoming Suffolk Community Services (formerly Suffolk Community Healthcare) as our latest partner. The change of encryption software from Egress to OME has caused a headache for some of the partners. We are working to sort this out, but in the meantime please be understanding if there is a delay in a referral. Remember, if you are a member of ACS or County Council staff you can find links to the referral form, Gliffy and the Hints and Tips on mySCC under Warm Handover Online Referrals. -

Annual-Report-2012-2013-2.Pdf
About ActivLives ActivLives is an independent charity working with individuals and communities, of all ages, but with a particular focus on people 45 plus who live in hard pressed areas in Ipswich and across Suffolk. The organisation has three major projects, ActivGardens, ActivAgeing and ActivSinging and has grown out of a Local Strategic Partnership initiative called the Town & Bridge Project, which started in 2006. Contents 2-3 - Contents & About Us 4 - Welcome to our first Annual Report 6 - Who are we? 7 - Our Impact 8-12 - ActivAgeing 13-19 - ActivGardens 20-23 - ActivSinging 23-29 - ActivLives Participation & Monitoring Data 30-31 - Volunteering and Employment 32 - Finance Report 32 - Future Plans for ActivLives 33 - Our Action Plan for 2014 34 - Our Supporters Our Registered Office 1, Cornhill Ipswich Suffolk IP1 1DD Tel: 01473 261112 Charity Registered Number : 1147615 Company Registered Number: 7672809 2 ActivLives Our Vision: Create stronger, healthier communities, reduce health inequalities and enable people to live full and active lives Our Mission: To provide services that engage and support individuals, families, family carers and communities to improve, maintain and sustain good health and well-being, particularly focusing in areas of deprivation and people mainly aged 45 years and over. Our Values: We deliver the mission as a team, underpinning our work with a set of agreed core values. These define ActivLives and are as follows: Honest & open - Creating trust through taking responsibility, acting ethically and encouraging -

Built Heritage Statement
Built Heritage Statement In respect of Land North of the A1071, Ipswich, Suffolk On behalf of Taylor Wimpey UK Ltd CgMs Ref: JAC24944 April 2021 FINAL cgms.co.uk /rpsgroup.com/uk CONTENTS CONTENTS Pages 1.0 Introduction 3 Prepared by: 2.0 Legislative and Planning Policy Framework Edward Hawkins BSc Econ (Hons) MSc ACIfA 2.1 Legislation and National Planning Policy 4 2.2 National Planning Guidance 5 2.3 Local Planning Policy and Guidance 7 3.0 Architectural and Historical Appraisal 3.1 Historical Development and Map Progression 8 Authorised by: 4.0 Assessment of Significance Veronica Cassin BArch, MA 4.1 Site Assessment and Identification of Assets 10 Thomas Copp BA (Hons) MA AssocIHBC Duncan Hawkins BA (hons) MSc FSA MCIfA 4.2 Statutorily Listed Buildings 14 5.0 Proposals and Assessment of Impact Report Status: 5.1 Proposed Development 22 5.2 Assessment of Impact 28 FINAL 6.0 Conclusions 29 Appendices CgMs Ref: Appendix A: Statutory List Description Appendix B: References JAC24944 Appendix C:Built Heritage Assets Plot Issue Date: APRIL 2021 COPYRIGHT © CgMs Part of RPS The material presented in this report is confidential. This report has been prepared for the exclusive use of the client and shall not be distributed or made available to any other company or person without the knowledge and written consent CgMs Heritage (part of RPS), © Ordnance Survey maps have been reproduced with the sanction of the controller of HM Stationery Office. Licence No: AL 100014723 cgms.co.uk /rpsgroup.com/uk 1.0 INTRODUCTION This Built Heritage Statement has been prepared by CgMs (part of RPS), A plot of all known Built Heritage Assets within 1.5km of the Site is given in on Behalf of Taylor Wimpey UK Ltd in relation to the proposed residential Appendix C.