Overview of Sexually Transmitted Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Trichomonas Vaginalis
Trichomonas Vaginalis Trichomonas Vaginalis - the basics It is a curable sexually transmitted infection (STI) caused by a protozoon called Trichomonas vaginalis, or ‘TV’. Protozoa are tiny germs similar to bacteria. TV can infect the vagina, urethra (water passage), and underneath the foreskin. Women may notice a change in vaginal discharge, and may have vulval itching or pain on passing urine. Men may notice a discharge from the tip of the penis, pain on passing urine or soreness of the foreskin. Testing is available at any specialised sexual health or Genitourinary Medicine (GUM) clinic and in some GP surgeries and contraceptive services. If you have TV we recommend that you have tests for other STIs including chlamydia, gonorrhoea, syphilis and HIV. How common is TV? In 2011 just over 6,000 cases were diagnosed in England. In contrast, more than 186,000 cases of chlamydia were reported in the same year. Over 90% of TV cases are diagnosed in women. How do you catch TV? TV is passed on- through unprotected vaginal sex, insertion of fingers into the vagina or sharing sex toys with someone who has TV from an infected mother to her baby during normal childbirth (vaginal delivery) TV cannot be caught from hugging, sharing baths or towels, swimming pools or toilet seats What would I notice if I had TV? Women may not notice anything wrong but they can still pass on TV to their sexual partner. Some women may notice one or more of the following: increased vaginal discharge an unpleasant vaginal smell ‘cystitis’ or burning pain when passing urine vulval itching or soreness pain in the vagina during sex Most men will not feel anything wrong but they can still pass TV on to their sexual partner. -

Trichomoniasis — “Trich” for Short — Is an Infection That Is Most Common in Sexually Active Women Age 16 to 35
FACT SHEET FOR PATIENTS AND FAMILIES Trichomoniasis What is trichomoniasis? Trichomoniasis — “trich” for short — is an infection that is most common in sexually active women age 16 to 35. (Men can have trich, too, but usually have fewer symptoms and often don’t need treatment to clear up the infection.) If you have trich, you need medication to stop your symptoms and prevent spreading the infection to sex partners. This handout gives you basic information on trichomoniasis, how it’s treated, and what you can do to prevent it. What causes it? Trichomoniasis is caused by a parasite, a tiny organism called Trichomonas vaginalis. Trich is passed from one person to another through sexual contact. Trich is one of the most common sexually transmitted infections or diseases (STIs or STDs) among young, sexually active women. Recent studies suggest that more Most common in young women, than 2 million women in the U.S. currently have trichomoniasis is a curable infection. trichomoniasis. Why is it a concern? What are the symptoms? Trich is completely curable, but you shouldn’t ignore A woman with trichomoniasis may have one or it. Trich can cause annoying and painful symptoms more of these common symptoms, which may (see the list at right) and may make it easier to catch come and go: another STI such as HIV, the virus that causes AIDS. • Vaginal discharge. The discharge may be gray, If you’re pregnant, trich brings these additional risks: yellow, or green. It may be thin or foamy and may • Your baby may be born too soon smell bad. -
Trichomoniasis (Trich)
health information Trichomoniasis (Trich) Trich is a sexually transmitted infection (STI) caused by a parasite called Trichomonas vaginalis. How do I get trich? Trich is passed between people through unprotected sex (sexual contact without a condom). How can I prevent trich? When you’re sexually active, the best way to prevent trich and other STIs is to use condoms for oral, vaginal, and anal sex. Don’t have any sexual contact if you or your partner(s) have symptoms of an STI, or may have been exposed to an STI. See a doctor or go to an STI Clinic for testing. Get STI testing every 3 to 6 months and when you have symptoms. How do I know if I have trich? The infection is most common in females in the vagina and in males in the tube that carries urine and semen (urethra). Many women with trich have no symptoms, but trich can cause: • vaginal discharge that smells musty • itching in and around the vagina • pain or burning when you pee • pain during intercourse Most males with trich have no symptoms, but they can still spread it. The best way to find out if you have trich is to get tested. Your nurse or doctor can test you by taking a swab. Is trich harmful? If not treated, trich may cause: • infertility or low sperm count in males • increased risk of pelvic infections in females • increased risk of getting other STIs and HIV 608183 © Alberta Health Services, (2014/04) What if I’m pregnant? If not treated, trich may cause premature rupture of the membranes, early delivery, and low birth weight. -

Chlamydia, Gonorrhoea, Trichomoniasis and Syphilis
Research Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016 Jane Rowley,a Stephen Vander Hoorn,b Eline Korenromp,c Nicola Low,d Magnus Unemo,e Laith J Abu- Raddad,f R Matthew Chico,g Alex Smolak,f Lori Newman,h Sami Gottlieb,a Soe Soe Thwin,a Nathalie Brouteta & Melanie M Taylora Objective To generate estimates of the global prevalence and incidence of urogenital infection with chlamydia, gonorrhoea, trichomoniasis and syphilis in women and men, aged 15–49 years, in 2016. Methods For chlamydia, gonorrhoea and trichomoniasis, we systematically searched for studies conducted between 2009 and 2016 reporting prevalence. We also consulted regional experts. To generate estimates, we used Bayesian meta-analysis. For syphilis, we aggregated the national estimates generated by using Spectrum-STI. Findings For chlamydia, gonorrhoea and/or trichomoniasis, 130 studies were eligible. For syphilis, the Spectrum-STI database contained 978 data points for the same period. The 2016 global prevalence estimates in women were: chlamydia 3.8% (95% uncertainty interval, UI: 3.3–4.5); gonorrhoea 0.9% (95% UI: 0.7–1.1); trichomoniasis 5.3% (95% UI:4.0–7.2); and syphilis 0.5% (95% UI: 0.4–0.6). In men prevalence estimates were: chlamydia 2.7% (95% UI: 1.9–3.7); gonorrhoea 0.7% (95% UI: 0.5–1.1); trichomoniasis 0.6% (95% UI: 0.4–0.9); and syphilis 0.5% (95% UI: 0.4–0.6). Total estimated incident cases were 376.4 million: 127.2 million (95% UI: 95.1–165.9 million) chlamydia cases; 86.9 million (95% UI: 58.6–123.4 million) gonorrhoea cases; 156.0 million (95% UI: 103.4–231.2 million) trichomoniasis cases; and 6.3 million (95% UI: 5.5–7.1 million) syphilis cases. -

Real-Time PCR Detection of Vaginal Microbiota and Sexually Transmitted Pathogens
Real-time PCR detection of vaginal microbiota and sexually transmitted pathogens A flexible, scalable, and low-cost solution for your laboratory We’ve combined the sensitivity and specificity of Applied Biosystems™ TaqMan ® Assays with the flexibility and scalability of the Applied Biosystems™ QuantStudio™ 12K Flex Real-Time PCR System, to offer you a new, low-cost solution for vaginal and urogenital microbiota investigations. Features include: • The ability to detect the broadest range of both commensal and pathogenic microbes compared to other currently available molecular tests • Qualified content, including positive controls, user guide, and analytical testing • Higher specificity, accuracy, and precision compared to traditional culture and microscopy methods • Flexible formats—choose from four assay formats, including single-tube assays, preloaded 96- or 384-well plates, and nanofluidic OpenArray™ plates • Lowest cost per sample compared to other commercially available solutions See other side for a list of TaqMan Assay targets included in this solution. The right testing solutions for your needs Offering the widest coverage of commensal and Download a complete list of Applied Biosystems™ TaqMan ® pathogenic microbes compared with other currently Vaginal Microbiota Assays at thermofisher.com/vm, or available molecular tests, our range of TaqMan Assays contact your sales representative. gives you the flexibility and freedom to configure a low- cost, high-throughput testing solution that’s right for you. Organism type Organism name -

Detection of Kaposi's Sarcoma–Associated Herpesvirus in Oral
1785 CONCISE COMMUNICATION Detection of Kaposi's Sarcoma±Associated Herpesvirus in Oral and Genital Secretions of Zimbabwean Women Thomas M. Lampinen,1,3 Shalini Kulasingam,1 1Departments of Epidemiology and 2Pathobiology and 3Center for AIDS Juno Min,4 Margaret Borok,6 Lovemore Gwanzura,7 and STD, University of Washington, Seattle; 4Department of Medicine 5 Downloaded from https://academic.oup.com/jid/article/181/5/1785/2191825 by guest on 29 September 2021 4 8 9 and Center for AIDS Research, Stanford University, Stanford, Julie Lamb, Kassam Mahomed, Godfrey B. Woelk, 6 7 2 2 California; Departments of Medicine, Medical Laboratory Sciences, Kurt B. Strand, Marnix L. Bosch, 8Obstetrics and Gynecology, and 9Community Medicine, 10 10,11 Daniel C. Edelman, Niel T. Constantine, University of Zimbabwe, Harare; 10Department of Pathology, David Katzenstein,4,5 and Michelle A. Williams1 University of Maryland and 11Institute of Human Virology, Baltimore, Maryland Kaposi's sarcoma±associated herpesvirus (KSHV) in oral and genital secretions of women may be involved in horizontal and vertical transmission in endemic regions. Nested polymerase chain reaction assays were used to detect KSHV DNA sequences in one-third of oral, vaginal, and cervical specimens and in 42% of peripheral blood mononuclear cell (PBMC) specimens collected from 41 women infected with human immunode®ciency virus type 1 who had Ka- posi's sarcoma (KS). KSHV DNA was not detected in specimens from 100 women without KS, 9 of whom were seropositive for KSHV. A positive association was observed between KSHV DNA detection in oral and genital mucosa, neither of which was associated with KSHV DNA detection in PBMC. -
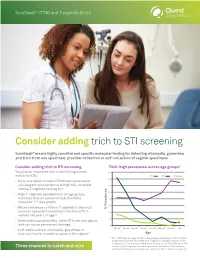
Consider Adding Trich to STI Screening
SureSwab® CT/NG and T. vaginalis (trich) Consider adding trich to STI screening SureSwab® means highly sensitive and specific molecular testing for detecting chlamydia, gonorrhea and trich from one specimen: provider collection or self-collection of vaginal specimens Consider adding trich to STI screening Trich: high prevalence across age groups2 You play an important role in identifying women 16 at risk for STIs. TV CT NG 14 • If you are about to order CT/NG testing because you suspect your patient is at high risk, consider 12 adding T. vaginalis testing too1 10 • High T. vaginalis prevalence in all age groups indicates that all women at risk should be 8 screened1,2,3,4 (see graph) 6 • Recent evidence confirms T. vaginalis is the most % Prevalence common sexually transmitted infection (STI) in 4 women >40 years of age1,2 2 • Even when asymptomatic, these STIs are contagious 1 and can cause permanent damage 0 18–19 20–24 25–29 30–34 35–39 40–44 45–49 >50 • Left undiscovered, chlamydia, gonorrhea or trich can live for months or years in the vagina1 Age * N = 7,593. Women aged 18–89 undergoing screening for C. trachomatis/ N. gonorrhoeae were also tested for T. vaginalis. Overall, prevalence for T. vaginalis, C. trachomatis and N. gonorrhoeae was 8.7%, 6.7% and 1.7% Three chances to catch and cure respectively. T. vaginalis was more prevalent than both C. trachomatis and N. gonorrhoeae in all age groups except the 18- to 19-year-old group.2 SureSwab® CT/NG and T. -

Trichomoniasis - CDC Fact Sheet
Trichomoniasis - CDC Fact Sheet What is trichomoniasis? Trichomoniasis (or “trich”) is a very common sexually transmitted disease (STD) that is caused by infection with a protozoan parasite called Trichomonas vaginalis. Although symptoms of the disease vary, most women and men who have the parasite cannot tell they are infected. How common is trichomoniasis? Trichomoniasis is considered the most common curable STD. In the United States, an estimated 3.7 million people have the infection, but only about 30% develop any symptoms of trichomoniasis. Infection is more common in women than in men, and older women are more likely than younger women to have been infected. How do people get trichomoniasis? The parasite is passed from an infected person to an uninfected person during sex. In women, the most commonly infected part of the body is the lower genital tract (vulva, vagina, or urethra), and in men, the most commonly infected body part is the inside of the penis (urethra). During sex, the parasite is usually transmitted from a penis to a vagina, or from a vagina to a penis, but it can also be passed from a vagina to another vagina. It is not common for the parasite to infect other body parts, like the hands, mouth, or anus. It is unclear why some people with the infection get symptoms while others do not, but it probably depends on factors like the person’s age and overall health. Infected people without symptoms can still pass the infection on to others. What are the signs and symptoms of trichomoniasis? About 70% of infected people do not have any signs or symptoms. -

Patient-Delivered Partner Therapy (PDPT) For
Patient-Delivered Partner Therapy (PDPT) for Chlamydia, Gonorrhea, and Trichomoniasis: Guidance for Medical Providers in California These guidelines were developed by the California Department of Public Health Sexually Transmitted Diseases (STD) Control Branch in collaboration with the California STD Controllers Association, the California STD/HIV Prevention Training Center, and the California Chlamydia Action Coalition August 2012 Patient-Delivered Partner Therapy (PDPT) for Chlamydia, Gonorrhea, and Trichomoniasis: Guidance for Medical Providers in California Organization This document is organized into the following sections and subsections: Introduction Summary Clinical Guidelines Background and Rationale Public health importance of chlamydia, gonorrhea, and trichomoniasis Barriers to effective partner management California legislation allowing PDPT Healthcare provider responsibilities for ensuring partner treatment Evidence for the effectiveness of PDPT Implementation and use of PDPT Liability issues Potential pitfalls in using PDPT Guidelines for Using PDPT for Chlamydia, Gonorrhea, and Trichomoniasis Selecting appropriate patients for PDPT Recommended treatment regimens Risk of adverse reactions to medications Risk of under-treating complicated infections and pharyngeal gonorrhea, and missing concurrent STD/HIV PDPT and pregnancy Key education and counseling Patient follow-up and retesting at three months Resources California PDPT resources California STD clinical practice guidelines CDC STD guidelines References cited Examples -

The Role of Mycoplasma Genitalium and Trichomonas Vaginalis
Research Etiology of urethral discharge in West Africa: the role of Mycoplasma genitalium and Trichomonas vaginalis Jacques Pe´ pin,1 Franc¸ois Sobe´la,2 Sylvie Deslandes,3 Michel Alary,4 Karsten Wegner,5 Nzambi Khonde,6 Fre´de´ric Kintin,7 Aloys Kamuragiye,8 Mohammed Sylla,9 Petit-Jean Zerbo,10 E´ nias Baganizi,11 Alassane Kone´,12 Fadel Kane,13 Benoit Maˆ sse,14 Pierre Viens,15 & Eric Frost16 Objective To determine the etiological role of pathogens other than Neisseria gonorrhoeae and Chlamydia trachomatis in urethral discharge in West African men. Methods Urethral swabs were obtained from 659 male patients presenting with urethral discharge in 72 primary health care facilities in seven West African countries, and in 339 controls presenting for complaints unrelated to the genitourinary tract. Polymerase chain reaction analysis was used to detect the presence of N. gonorrhoeae, C. trachomatis, Trichomonas vaginalis, Mycoplasma genitalium, and Ureaplasma urealyticum. Findings N. gonorrhoeae, T. vaginalis, C. trachomatis, and M. genitalium — but not U. urealyticum — were found more frequently in men with urethral discharge than in asymptomatic controls, being present in 61.9%, 13.8%, 13.4% and 10.0%, respectively, of cases of urethral discharge. Multiple infections were common. Among patients with gonococcal infection, T. vaginalis was as frequent a coinfection as C. trachomatis. M. genitalium, T. vaginalis, and C. trachomatis caused a similar clinical syndrome to that associated with gonococcal infection, but with a less severe urethral discharge. Conclusions M. genitalium and T. vaginalis are important etiological agents of urethral discharge in West Africa. The frequent occurrence of multiple infections with any combination of four pathogens strongly supports the syndromic approach. -

Trichomoniasis 20.Pdf
Trichomoniasis Brown Health Services Patient Education Series ejaculation. The infection in people with penises is What is trichomoniasis? usually transient and lasts less than 10 days. Trichomoniasis is a sexually transmitted infection Are there medical complications? (STI) that affects people of all genders. although symptoms are more common in people with Trichomoniasis in pregnant women is associated vaginas. It is caused by a protozoan parasite called with premature rupture of the membranes and Trichomonas vaginalis and is a cause of vaginal preterm delivery. The genital inflammation caused infections and urethral infections in people with by trichomoniasis may also increase a woman’s risk penises. of acquiring HIV infection if she is exposed to HIV. How do people get it? How is it diagnosed? As with other STIs, trichomoniasis is spread through To diagnose trichomoniasis, a medical provider sexual contact. People with vulvas contract performs a physical exam and laboratory test. trichomoniasis from infected partners with vulvas A pelvic exam can reveal small red ulcerations on or penises while people with penises usually the vaginal wall or cervix. A sample of vaginal fluid contract it only from partners with vulvas or urethral fluid is examined under the microscope to look for the disease- causing parasite. In difficult What are signs and symptoms? to treat cases, other laboratory testing is available. Many people with vaginas with trichomoniasis have The parasite is harder to detect in people with symptoms. In these people, it causes a frothy, penises. Partners with penises of infected people yellow-green vaginal discharge with a strong odor. with vaginas should be treated without testing. -

PROTOZOAN GENITAL INVASIONS CAUSED by the REPRESENTATIVES of TRICHOMONAS and GIARDIA DOI: 10.36740/Wlek202002133
Wiadomości Lekarskie 2020, tom LXXIII, nr 2 © Wydawnictwo Aluna REVIEW ARTICLE PRACA POGLĄDOWA PROTOZOAN GENITAL INVASIONS CAUSED BY THE REPRESENTATIVES OF TRICHOMONAS AND GIARDIA DOI: 10.36740/WLek202002133 Pavlo V. Fedorych1, Gennadiy I. Mavrov2, Tetiana V. Osinska2, Yuliia V. Shcherbakova2 1UKRAINIAN MILITARY MEDICAL ACADEMY, KYIV, UKRAINE 2 STATE ЕSTABLISHMENT “INSTITUTE OF DERMATOLOGY AND VENEREOLOGY OF THE NATIONAL ACADEMY OF MEDICAL SCIENCES OF UKRAINE”, KHARKIV, UKRAINE ABSTRACT The aim was to perform systematic review of genitourinary protozoan invasion and analyze their pathogenicity and the ability to influence the genitourinary infections. Materials and methods: For systematic review of papers the EMBASE and PubMed databases were searched. We also reviewed our own pilot studies using real-time polymerase chain reaction (PCR) to determine Trichomonas tenax, Pentatrichomonas hominis and Giardia lamblia. Conclusions: Trichomonas tenax, Pentatrichomonas hominis, Giardia lamblia can cause genitourinary invasion in addition to Trichomonas vaginalis. Their eradication is obligatory at least for not keeping intact pathogenic microorganisms phagocyted by Trichomonas spp. Defining the protozoan forms is important in preventing of genital infections recurrences and reinfections. KEY WORDS: Trichomonas vaginalis, Trichomonas tenax, Pentatrichomonas hominis, Giardia lamblia Wiad Lek. 2020;73(2):380-383 INTRODUCTION the results were discordant significantly. Moreover, con- Parasitic invasion is a medical and biological notion that trary