Apparent Density, Trypanosome Infection Rates and Host Preference of Tsetse Fies in the Sleeping Sickness Endemic Focus of Northwestern Uganda
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human African Trypanosomiasis Transmission, Kinshasa
DISPATCHES healthy inhabitants of Leopoldville (6). In 1960, the Human African Kinshasa focus was considered extinct, and no tsetse flies were found in the city. Until 1995, an average of 50 new Trypanosomiasis cases of HAT were reported annually. However, >200 new cases have been reported annually since 1996 (e.g., 443 of Transmission, 6,205 persons examined in 1998 and 912 of 42,746 per- sons examined in 1999) (7). Ebeja et al. reported that 39% Kinshasa, of new cases were urban residents; 60% of them in the first stage of the disease (3). Democratic To understand the epidemiology of HAT in this context, several investigations have been undertaken (3,5,8). On Republic of Congo the basis of epidemiologic data, some investigators (3,5) have suggested that urban or periurban transmission of Gustave Simo,*† Philemon Mansinsa HAT occurs in Kinshasa. However, in a case-control study, Diabakana,‡ Victor Kande Betu Ku Mesu,‡ Robays et al. concluded that HAT in urban residents of Emile Zola Manzambi,§ Gaelle Ollivier,¶ Kinshasa was linked to disease transmission in Bandundu Tazoacha Asonganyi,† Gerard Cuny,# and rural Kinshasa (8). To investigate the epidemiology of and Pascal Grébaut# HAT transmission in Kinshasa, we identified and evaluat- ed contact between humans and flies. The prevalence of To investigate the epidemiology of human African try- Trypanosoma brucei gambiense in tsetse fly midguts was panosomiasis (sleeping sickness) in Kinshasa, Democratic determined to identify circulation of this trypanosome Republic of Congo, 2 entomologic surveys were conducted between humans and tsetse flies. in 2005. Trypanosoma brucei gambiense and human-blood meals were found in tsetse fly midguts, which suggested The Study active disease transmission. -

Tororo Profile.Indd
Tororo District Hazard, Risk and Vulnerability Profi le 2016 TORORO DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE a Acknowledgment On behalf of Office of the Prime Minister, I wish to express my sincere appreciation to all of the key stakeholders who provided their valuable inputs and support to this Multi-Hazard, Risk and Vulnerability mapping exercise that led to the production of a comprehensive district Hazard, Risk and Vulnerability (HRV) profiles. I extend my sincere thanks to the Department of Relief, Disaster Preparedness and Management, under the leadership of the Commissioner, Mr. Martin Owor, for the oversight and management of the entire exercise. The HRV assessment team was led by Ms. Ahimbisibwe Catherine, Senior Disaster Preparedness Officer supported by Odong Martin, DisasterM anagement Officer and the team of consultants (GIS/ DRR specialists); Dr. Bernard Barasa, and Mr. Nsiimire Peter, who provided technical support. Our gratitude goes to UNDP for providing funds to support the Hazard, Risk and Vulnerability Mapping. The team comprised of Mr. Steven Goldfinch – Disaster Risk Management Advisor, Mr. Gilbert Anguyo - Disaster Risk Reduction Analyst, and Mr. Ongom Alfred-Early Warning system Programmer. My appreciation also goes to the Tororo District team. The entire body of stakeholders who in one way or another yielded valuable ideas and time to support the completion of this exercise. Hon. Hilary O. Onek Minister for Relief, Disaster Preparedness and Refugees TORORO DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE i EXECUTIVE SUMMARY The multi-hazard vulnerability profile output from this assessment was a combination of spatial modeling using socio-ecological spatial layers (i.e. DEM, Slope, Aspect, Flow Accumulation, Land use, vegetation cover, hydrology, soil types and soil moisture content, population, socio-economic, health facilities, accessibility, and meteorological data) and information captured from District Key Informant interviews and sub-county FGDs using a participatory approach. -

33 Years of Development 1986 – 2019
UGANDA BUREAU OF STATISTICS ENHANCING DATA QUALITY AND USE LIBERATION DAY CELEBRATIONS JANUARY 26, 2019, TORORO DISTRICT National Theme: Victory Day Anniversary: A Moment of Glory that set a new Chapter for a United, Peaceful and Prosperous Uganda 33 YEARS OF DEVELOPMENT 1986 – 2019 Understanding the Journey through Statistics ugstats @statisticsug Uganda Bureau of Statistics www.ubos.org LIBERATION DAY CELEBRATIONS JANUARY 26, 2019, TORORO DISTRICT GUEST OF HONOUR: H.E. Yoweri Kaguta Museveni, President of the Republic of Uganda Preamble “The Liberation Day is celebrated country-wide every January 26, of the year. The day commemorates and salutes the contribution of selfless citizens who engineered the Country’s Liberation Movement climaxing into a new Government in 1986 and the progress made ever since to date. ” It is therefore our pleasure to share with you the selected statistical indicators across sectors highlighting the nation’s growth & recovery paths over the years since 1986. H.E Yoweri Kaguta Museveni President of the Republic of Uganda Congratulatory message The Board of Directors, Management and Staff of the Uganda Bureau of Statistics congratulate His Excellency the President of the Republic of Uganda Yoweri Kaguta Museveni and the entire people of Uganda on this occasion of celebrating the 33rd Liberation Day anniversary. As we join the rest of the country in the celebration, we take the honour to salute all patriotic Ugandans in their desirous and selfless efforts geared towards sustaining the victory and gains of the Liberation Movement. In the same spirit, we commit ourselves to continuously deliver on our mandate of producing and disseminating quality official statistics for continuous and sustainable national Development. -

Documenting and Disseminating Agricultural Indigenous Knowledge for Sustainable Food Security in Uganda
Documenting and disseminating agricultural indigenous knowledge for sustainable food security in Uganda Eric Nelson Haumba [email protected] and Sarah Kaddu, PhD [email protected] Abstract There is a wealth of agricultural indigenous knowledge (AIK) in Uganda, which is useful in livestock keeping, crop management and food processing and storage as well as soil and water management. Unfortunately, this AIK is becoming less visible and irrelevant in some communities because of the adoption of modern methods of farming. In fact, a lot of AIK has remained largely undocumented which threatens its sustained utilisation. One of the bottlenecks of the effective utilisation of AIK is access to relevant and usable indigenous knowledge for the diverse stakeholders in the agricultural sector including farmers. It seems farmers in Uganda are adopting modern methods of agriculture at the expense of the AIK because of the less perceived benefits that AIK promises because crops planted using AIK have often faced pests and diseases and not yielded much. The problem is perhaps compounded because of increasing population growth, land fragmentation as well as migration to urban areas. This phenomenon raises the question of how AIK can be conserved. This paper is based on a study that investigated how Agricultural Indigenous Knowledge (AIK) is documented and disseminated in addition to identifying the challenges faced in its management for sustainable food security in Uganda’s district of Soroti. Data in this study was collected through interviews, focus group discussions, document reviews and participant observation. The study findings revealed that despite the advent of modern farming methods, many small-scale farmers in the Soroti district continue to embrace indigenous knowledge in farming such as in managing soil fertility, controlling pests and diseases, controlling weeds, soil preparation, planting materials, harvesting and storage of indigenous root crops and animals. -

WHO UGANDA BULLETIN February 2016 Ehealth MONTHLY BULLETIN
WHO UGANDA BULLETIN February 2016 eHEALTH MONTHLY BULLETIN Welcome to this 1st issue of the eHealth Bulletin, a production 2015 of the WHO Country Office. Disease October November December This monthly bulletin is intended to bridge the gap between the Cholera existing weekly and quarterly bulletins; focus on a one or two disease/event that featured prominently in a given month; pro- Typhoid fever mote data utilization and information sharing. Malaria This issue focuses on cholera, typhoid and malaria during the Source: Health Facility Outpatient Monthly Reports, Month of December 2015. Completeness of monthly reporting DHIS2, MoH for December 2015 was above 90% across all the four regions. Typhoid fever Distribution of Typhoid Fever During the month of December 2015, typhoid cases were reported by nearly all districts. Central region reported the highest number, with Kampala, Wakiso, Mubende and Luweero contributing to the bulk of these numbers. In the north, high numbers were reported by Gulu, Arua and Koti- do. Cholera Outbreaks of cholera were also reported by several districts, across the country. 1 Visit our website www.whouganda.org and follow us on World Health Organization, Uganda @WHOUganda WHO UGANDA eHEALTH BULLETIN February 2016 Typhoid District Cholera Kisoro District 12 Fever Kitgum District 4 169 Abim District 43 Koboko District 26 Adjumani District 5 Kole District Agago District 26 85 Kotido District 347 Alebtong District 1 Kumi District 6 502 Amolatar District 58 Kween District 45 Amudat District 11 Kyankwanzi District -

1. Introduction
1. Introduction 1.1 Background to the Case Study This report presents a case study on bicycles, women and rural transport in Uganda. It is the result of field work carried out in the Mbale and Tororo districts of eastern Uganda during a three-week visit in September 1991. The case study forms part of the Rural Travel and Transport Project (RTTP) of the World Bank- financed Sub-Saharan Africa Transport Program (SSATP), a major research program covering transport in SSA. One aspect of this program is the RTTP, which is designed to focus on transport at the level where it has the most direct influence on economic (particularly agricultural) and social development in rural areas of SSA. One of the key aims of the RTTP is to recommend approaches to the improvement of rural transport services, and to the adoption of intermediate technologies to increase personal mobility and agricultural production. This research is being conducted through Village-Level Transport and Travel Surveys (VLTTS) and related case studies. The World Bank has commissioned the International Labor Organization, in collaboration with I.T. Transport, to execute the VLTTS and the related case studies under the RTTP. 1.2 General Objectives of the Case Study The objective of the case study is to investigate two key aspects of rural mobility and accessibility focusing on: (i) The role of intermediate means of transport (IMT) in improving mobility, and the institutional and implementation policy requirements necessary for developing the use of IMT; and (ii) The role of transport in women's daily lives, - given that a major part of the transport burden falls on women in addition to their substantial agricultural and domestic responsibilities, and the impact of improvements in mobility and accessibility upon women. -

Structure of Some East African Glossina Fuscipes Fuscipes Populations E
Entomology Publications Entomology 9-2008 Structure of some East African Glossina fuscipes fuscipes populations E. S. Krafsur Iowa State University, [email protected] J. G. Marquez Iowa State University J. O. Ouma Iowa State University Follow this and additional works at: http://lib.dr.iastate.edu/ent_pubs Part of the Entomology Commons, Evolution Commons, and the Population Biology Commons The ompc lete bibliographic information for this item can be found at http://lib.dr.iastate.edu/ ent_pubs/416. For information on how to cite this item, please visit http://lib.dr.iastate.edu/ howtocite.html. This Article is brought to you for free and open access by the Entomology at Iowa State University Digital Repository. It has been accepted for inclusion in Entomology Publications by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Structure of some East African Glossina fuscipes fuscipes populations Abstract Glossina fuscipes fuscipes Newstead 1910 (Diptera: Glossinidae) is the primary vector of human sleeping sickness in Kenya and Uganda. This is the first report on its population structure. A total of 688 nucleotides of mitochondrial ribosomal 16S2 and cytochrome oxidase I genes were sequenced. Twenty-one variants were scored in 79 flies from three geographically diverse natural populations. Four haplotypes were shared among populations, eight were private and nine were singletons. The mean haplotype and nucleotide diversities were 0.84 and 0.009, respectively. All populations were genetically differentiated and were at demographic equilibrium. In addition, a longstanding laboratory culture originating from the Central African Republic (CAR-lab) in 1986 (or before) was examined. -

Tsetse Flies (Glossina) As Vectors of Human African Trypanosomiasis: a Review
Hindawi Publishing Corporation BioMed Research International Volume 2016, Article ID 6201350, 8 pages http://dx.doi.org/10.1155/2016/6201350 Review Article Tsetse Flies (Glossina) as Vectors of Human African Trypanosomiasis: A Review Florence Njeri Wamwiri and Robert Emojong Changasi Kenya Agricultural and Livestock Research Organisation, Biotechnology Research Institute, P.O. Box 362, Muguga 00902, Kenya Correspondence should be addressed to Florence Njeri Wamwiri; [email protected] Received 5 November 2015; Revised 2 February 2016; Accepted 4 February 2016 Academic Editor: Carlos E. Almeida Copyright © 2016 F. N. Wamwiri and R. E. Changasi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Human African Trypanosomiasis (HAT) transmitted by the tsetse fly continues to be a public health issue, despite more than a century of research. There are two types of the disease, the chronic gambiense and the acute rhodesiense-HAT. Fly abundance and distribution have been affected by changes in land-use patterns and climate. However, disease transmission still continues. Here, we review some aspects of HAT ecoepidemiology in the context of altered infestation patterns and maintenance of the transmission cycle as well as emerging options in disease and vector control. 1. Introduction 24 countries in west and central Africa and accounts for about 98% of reported cases (WHO Technical Report 2012). The African trypanosomiasis is one of a diverse range of neglected Democratic Republic of Congo (DRC) continues to report tropical diseases. The tsetse fly, Glossina sp.isthemainvector the highest number of gHATcases,contributingupto84% for trypanosomes, the parasites that cause trypanosomiasis. -

The Glossina Genome Cluster: Comparative Genomic Analysis of the Vectors of African
bioRxiv preprint doi: https://doi.org/10.1101/531749; this version posted January 27, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 The Glossina Genome Cluster: Comparative Genomic Analysis of the Vectors of African 2 Trypanosomes 3 Authorship: 4 Geoffrey M. Attardo, ([email protected]) *22; Adly M.M. Abd-Alla, (a.m.m.abd- 5 [email protected])13; Alvaro Acosta-Serrano, ([email protected])16; James E. 6 Allen, ([email protected])6; Rosemary Bateta, ([email protected])2; Joshua B. Benoit, 7 ([email protected])24; Kostas Bourtzis, ([email protected])13; Jelle Caers, 8 ([email protected])15; Guy Caljon, ([email protected])21; Mikkel B. Christensen, 9 ([email protected])6; David W. Farrow, ([email protected])24; Markus Friedrich, 10 ([email protected])33; Aurélie Hua-Van, ([email protected])5; Emily C. 11 Jennings, ([email protected])24; Denis M. Larkin, ([email protected])19; Daniel Lawson, 12 ([email protected])10; Michael J. Lehane, ([email protected])16; Vasileios 13 P. Lenis, ([email protected])30; Ernesto Lowy-Gallego, ([email protected])6; 14 Rosaline W. Macharia, ([email protected], [email protected])27,12; Anna R. Malacrida, 15 ([email protected])29; Heather G. Marco, ([email protected])23; Daniel Masiga, 16 ([email protected])12; Gareth L. Maslen, ([email protected])6; Irina Matetovici, 17 ([email protected])11; Richard P. -
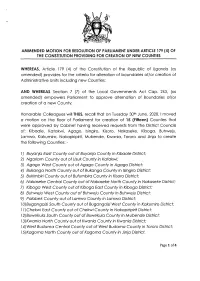
(4) of the Constitution Providing for Creation of New Counties
AMMENDED MOTTON FOR RESOLUTTON OF PARLTAMENT UNDER ARTTCLE 179 (4) OF THE CONSTITUTION PROVIDING FOR CREATION OF NEW COUNTIES WHEREAS, Ariicle 179 (a) of the Constitution of the Republic of Ugondo (os omended) provides for the criterio for olterotion of boundories oflor creotion of Administrotive Units including new Counties; AND WHEREAS Section 7 (7) of the Locql Governments Act Cop. 243, (os omended) empowers Porlioment to opprove olternotion of Boundories of/or creotion of o new County; Honoroble Colleogues willTHUS, recoll thot on Tuesdoy 30rn June, 2020,1 moved o motion on the floor of Porlioment for creotion of I5 (Fitteen) Counties thot were opproved by Cobinet hoving received requests from the District Councils of; Kiboole, Kotokwi, Agogo, lsingiro, Kisoro, Nokoseke, Kibogo, Buhweju, Lomwo, Kokumiro, Nokopiripirit, Mubende, Kwonio, Tororo ond Jinjo to creote the following Counties: - l) Buyanja Eost County out of Buyanjo County in Kibaale Distric[ 2) Ngoriom Covnty out of Usuk County in Kotakwi; 3) Agago Wesf County out of Agogo County in Agogo District; 4) Bukonga Norfh County out of Bukongo County in lsingiro District; 5) Bukimbiri County out of Bufumbira County in Kisoro District; 6) Nokoseke Centrol County out of Nokoseke Norfh County in Nokoseke Disfricf 7) Kibogo Wesf County out of Kibogo Eost County in Kbogo District; B) Buhweju West County aut of Buhweju County in Buhweju District; 9) Palobek County out of Lamwo County in Lamwo District; lA)BugongoiziSouth County out of BugongoiziWest County in Kokumiro Districf; I l)Chekwi Eosf County out of Chekwi County in Nokopiripirit District; l2)Buweku/o Soufh County out of Buweku/o County in Mubende Disfricf, l3)Kwanio Norfh County out of Kwonio Counfy in Kwonio Dislricf l )West Budomo Central County out of Wesf Budomo County inTororo Districf; l5)Kogomo Norfh County out of Kogomo County in Jinjo Districf. -

Intestinal Bacterial Communities of Trypanosome-Infected and Uninfected Glossina Palpalis Palpalis from Three Human African Trypanomiasis Foci in Cameroon
ORIGINAL RESEARCH published: 03 August 2017 doi: 10.3389/fmicb.2017.01464 Intestinal Bacterial Communities of Trypanosome-Infected and Uninfected Glossina palpalis palpalis from Three Human African Trypanomiasis Foci in Cameroon Franck Jacob 1, Trésor T. Melachio 2, Guy R. Njitchouang 2, Geoffrey Gimonneau 1, Flobert Njiokou 2, Luc Abate 3, Richard Christen 4, Julie Reveillaud 5, 6 and Anne Geiger 1* 1 UMR INTERTRYP, Institut de Recherche pour le Développement-CIRAD, CIRAD TA A-17/G, Montpellier, France, 2 Parasitology and Ecology Laboratory, Department of Animal Biology and Physiology, Faculty of Science, University of Yaounde 1, Yaounde, Cameroon, 3 UMR MIVEGEC, Institut de Recherche pour le Développement 224-Centre National de la Recherche Scientifique 5290, Montpellier, France, 4 UMR 7138, Systématique Adaptation Evolution, Université de Edited by: Nice-Sophia Antipolis, Nice, France, 5 Institut National de la Recherche Agronomique, UMR 1309 ASTRE, Montpellier, Alexandre Morrot, France, 6 CIRAD, UMR ASTRE, Montpellier, France Federal University of Rio de Janeiro, Brazil Glossina sp. the tsetse fly that transmits trypanosomes causing the Human or the Animal Reviewed by: Brice Rotureau, African Trypanosomiasis (HAT or AAT) can harbor symbiotic bacteria that are known to Institut Pasteur, France play a crucial role in the fly’s vector competence. We hypothesized that other bacteria Frédéric Mahé, could be present, and that some of them could also influence the fly’svector competence. Centre de Coopération Internationale en Recherche Agronomique Pour le In this context the objectives of our work were: (a) to characterize the bacteria that Développement (CIRAD), France compose the G. palpalis palpalis midgut bacteriome, (b) to evidence possible bacterial *Correspondence: community differences between trypanosome-infected and non-infected fly individuals Anne Geiger [email protected] from a given AAT and HAT focus or from different foci using barcoded Illumina sequencing of the hypervariable V3-V4 region of the 16S rRNA gene. -

Elgon Investment Profile 2018
ELGON INVESTMENT PROFILE 2018 BULAMBULI KWEEN KAPCHORWA BUKWO SIRONKO BUDUDA MBALE KENYA MANAFWA Elgon Investment Profile A Sipi Falls in Kapchorwa B Elgon Investment Profile Background Information This is an Economic region The two sub regions have deriving its name from the dominant cooperative unions Mt. Elgon on whose slopes through which most of their the region is situated and is economic activities are comprised of the Bugisu districts centered, that is, the Bugisu of Mbale, Sironko, Manafwa, Cooperative Union and the Bududa and Bulambuli and the Sebei Cooperative Union. Sebei districts of Kapchorwa, The region is well known for Kween and Bukwo. The region its Arabica Coffee which is is located in Eastern Uganda mainly grown, processed and with Mbale the principal town marketed through these two located about 245 km from cooperative unions. Kampala. The region borders Kenya which can be accessed The region has a unique climate through Suam border post in pattern which favors special Bukwo district and Lwakhaka crops such as wheat, barley and border post in Manafwa. It other cereals like maize, and neighbors the Karamoja, Teso sorghum used in commercial and Bukedi regions internally. beer production. This plus the high tourism potential Three groups populate the derived from the Mountain Mount Elgon region, all highly and its associated ecosystems dependent on the forest make the Elgon region a high ecosystem: the Bagisu, the economic potential region. Sabiny, and a small group of The main town Mbale has historically forest-dwelling a gazetted industrial and and forest dependent upland business park whose activities Sabiny known as the Benet.