Covid-19 and Tobacco Industry Interference
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Project SUN: a Study of the Illicit Cigarette Market In
Project SUN A study of the illicit cigarette market in the European Union, Norway and Switzerland 2017 Results Executive Summary kpmg.com/uk Important notice • This presentation of Project SUN key findings (the ‘Report’) has been prepared by KPMG LLP the UK member firm (“KPMG”) for the Royal United Services Institute for Defence and Security Studies (RUSI), described in this Important Notice and in this Report as ‘the Beneficiary’, on the basis set out in a private contract dated 27 April 2018 agreed separately by KPMG LLP with the Beneficiary (the ‘Contract’). • Included in the report are a number of insight boxes which are written by RUSI, as well as insights included in the text. The fieldwork and analysis undertaken and views expressed in these boxes are RUSI’s views alone and not part of KPMG’s analysis. These appear in the Foreword on page 5, the Executive Summary on page 6, on pages 11, 12, 13 and 16. • Nothing in this Report constitutes legal advice. Information sources, the scope of our work, and scope and source limitations, are set out in the Appendices to this Report. The scope of our review of the contraband and counterfeit segments of the tobacco market within the 28 EU Member States, Switzerland and Norway was fixed by agreement with the Beneficiary and is set out in the Appendices. • We have satisfied ourselves, so far as possible, that the information presented in this Report is consistent with our information sources but we have not sought to establish the reliability of the information sources by reference to other evidence. -

Iowa Directory of Certified Tobacco Product Manufacturers and Brands PLEASE NOTE Flavored Cigarettes & RYO Are Now Illegal
Iowa Directory of Certified Tobacco Product Manufacturers and Brands PLEASE NOTE Flavored Cigarettes & RYO are now illegal. Regardless of being on this List. See footnote *(3) 8/12/20 Iowa Additions to the Directory (within the last six months) PM Philip Morris USA Nat's cigarettes 8/12/20 PM Liggett Group Inc. Montego cigarettes 6/8/20 Deletions to the Directory (within the last six months) PM Sherman 1400 Broadway NYC, Ltd. Nat's cigarettes 8/12/20 PM Japan Tobacco International Wings cigarettes 5/7/20 PM King Maker Marketing Ace cigarettes 5/7/20 PM King Maker Marketing Gold Crest cigarettes 5/7/20 PM Kretek International Dreams cigarettes 5/7/20 Type of Manufacturer is for Participating (PM) or Non-Participating (NPM) with the Master Settlement Agreement. TYPE MANUFACTURER BRAND PRODUCT DATE NPM Cheyenne International, LLC Aura cigarettes 8/4/10 NPM Cheyenne International, LLC Cheyenne cigarettes 2/1/05 NPM Cheyenne International, LLC Decade cigarettes 2/1/05 PM Commonwealth Brands Inc Crowns cigarettes 5/31/11 PM Commonwealth Brands Inc Montclair cigarettes 7/22/03 PM Commonwealth Brands Inc Sonoma cigarettes 7/22/03 PM Commonwealth Brands Inc USA Gold cigarettes 7/22/03 PM Farmers Tobacco Company of Cynthiana, Inc. Baron American Blend cigarettes 9/20/05 PM Farmers Tobacco Company of Cynthiana, Inc. Kentucky's Best cigarettes 7/22/03 PM Farmers Tobacco Company of Cynthiana, Inc. Kentucky's Best roll your own 1/4/08 PM Farmers Tobacco Company of Cynthiana, Inc. VB - Made in the USA cigarettes 9/20/05 PM ITG Brands, LLC Fortuna cigarettes 12/21/18 PM ITG Brands, LLC Kool cigarettes 6/12/15 PM ITG Brands, LLC Maverick cigarettes 6/12/15 PM ITG Brands, LLC Rave cigarettes 12/12/14 PM ITG Brands, LLC Salem cigarettes 6/12/15 PM ITG Brands, LLC Winston cigarettes 6/12/15 PM Japan Tobacco International Export 'A' cigarettes 5/24/12 PM Japan Tobacco International LD cigarettes 2/22/17 PM Japan Tobacco International Wave cigarettes 7/22/03 PM King Maker Marketing Wildhorse cigarettes 12/13/18 NPM KT&G Corp. -
Cigarette Minimum Retail Price List
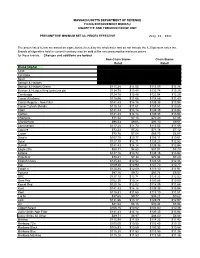
MASSACHUSETTS DEPARTMENT OF REVENUE FILING ENFORCEMENT BUREAU CIGARETTE AND TOBACCO EXCISE UNIT PRESUMPTIVE MINIMUM RETAIL PRICES EFFECTIVE July 26, 2021 The prices listed below are based on cigarettes delivered by the wholesaler and do not include the 6.25 percent sales tax. Brands of cigarettes held in current inventory may be sold at the new presumptive minimum prices for those brands. Changes and additions are bolded. Non-Chain Stores Chain Stores Retail Retail Brand (Alpha) Carton Pack Carton Pack 1839 $86.64 $8.66 $85.38 $8.54 1st Class $71.49 $7.15 $70.44 $7.04 Basic $122.21 $12.22 $120.41 $12.04 Benson & Hedges $136.55 $13.66 $134.54 $13.45 Benson & Hedges Green $115.28 $11.53 $113.59 $11.36 Benson & Hedges King (princess pk) $134.75 $13.48 $132.78 $13.28 Cambridge $124.78 $12.48 $122.94 $12.29 Camel All others $116.56 $11.66 $114.85 $11.49 Camel Regular - Non Filter $141.43 $14.14 $139.35 $13.94 Camel Turkish Blends $110.14 $11.01 $108.51 $10.85 Capri $141.43 $14.14 $139.35 $13.94 Carlton $141.43 $14.14 $139.35 $13.94 Checkers $71.54 $7.15 $70.49 $7.05 Chesterfield $96.53 $9.65 $95.10 $9.51 Commander $117.28 $11.73 $115.55 $11.56 Couture $72.23 $7.22 $71.16 $7.12 Crown $70.76 $7.08 $69.73 $6.97 Dave's $107.70 $10.77 $106.11 $10.61 Doral $127.10 $12.71 $125.23 $12.52 Dunhill $141.43 $14.14 $139.35 $13.94 Eagle 20's $88.31 $8.83 $87.01 $8.70 Eclipse $137.16 $13.72 $135.15 $13.52 Edgefield $73.41 $7.34 $72.34 $7.23 English Ovals $125.44 $12.54 $123.59 $12.36 Eve $109.30 $10.93 $107.70 $10.77 Export A $120.88 $12.09 $119.10 $11.91 -

Pub 302 WI Alcohol Beverage And
State of Wisconsin Department of Revenue Wisconsin Alcohol Beverage and Tobacco Laws for Retailers Publication 302 (12/16) Table of Contents Page I. INTRODUCTION .................................................................................................................................3 II. DEFINITIONS.......................................................................................................................................3 III. ALCOHOL BEVERAGE LAW ............................................................................................................5 A. Closing Hours ..................................................................................................................................5 B. Daylight Saving Time ......................................................................................................................5 C. Training Requirements For Completion Of The Responsible Beverage Server Training Course (Required As A Condition Of Licensing) ........................................................................................6 IV. LICENSING ..........................................................................................................................................6 V. SALE OF ALCOHOL BEVERAGES ...................................................................................................6 VI. SELLER’S PERMIT..............................................................................................................................6 VII. FEDERAL TAX STAMP .......................................................................................................................7 -
Directory for Cigarettes and Roll-Your-Own Tobacco
DEPARTMENT OF THE ATTORNEY GENERAL STATE OF HAWAI‘I DIRECTORY FOR CIGARETTES AND ROLL-YOUR-OWN TOBACCO of Certified Tobacco Product Manufacturers Brands and Brand Families (Available at: http://ag.hawaii.gov/cjd/tobacco-enforcement-unit/) DEPARTMENT OF THE ATTORNEY GENERAL TOBACCO ENFORCEMENT UNIT 425 QUEEN STREET HONOLULU, HAWAI‘I 96813 (808) 586-1203 INDEX I. Directory: Cigarettes and Roll-Your-Own Tobacco Page 1.INTRODUCTION 3 2.DEFINITIONS 3 3.NOTICES 6 II. Summary for Directory Posted December 15, 2019* III. Alphabetical Brand List IV. Compliant Participating Manufacturers List V. Compliant Non-Participating Manufacturers List Posted: December 15, 2019 (last update October 15, 2019) 2 1. INTRODUCTION Pursuant to Haw. Rev. Stat. §245-22.5(a), beginning December 1, 2003, it shall be unlawful for an entity to (1) affix a stamp to a package or other container of cigarettes belonging to a tobacco product manufacturer or brand family not included in this directory, or (2) import, sell, offer, keep, store, acquire, transport, distribute, receive, or possess for sale or distribution cigarettes1 belonging to a tobacco product manufacturer or brand family not included in this directory. Pursuant to §245-22.5(b), any entity that knowingly violates subsection (a) shall be guilty of a class C felony. Pursuant to Haw. Rev. Stat. §§245-40 and 245-41, any cigarettes unlawfully possessed, kept, stored, acquired, transported, sold, imported, offered, received, or distributed in violation of Haw. Rev. Stat. Chapter 245 may be seized, confiscated, and ordered forfeited pursuant to Haw. Rev. Stat., Chapter 712A. In addition, the attorney general may apply for a temporary or permanent injunction restraining any person from violating or continuing to violate Haw. -

DISTRICT of COLUMBIA TOBACCO DIRECTORY Last Updated 07/30/20 Page 1 of 4
DISTRICT OF COLUMBIA TOBACCO DIRECTORY Last Updated 07/30/20 Page 1 of 4 MANUFACTURER PM/NPM BRAND FAMILY Commonwealth Brands Inc. PM Crowns Commonwealth Brands Inc. PM Montclair Commonwealth Brands Inc. PM Sonoma Commonwealth Brands Inc. PM USA Gold Firebird Manufacturing, LLC NPM Cherokee Firebird Manufacturing, LLC NPM Palmetto Grand River Enterprises Six Nations, Ltd. NPM Couture Grand River Enterprises Six Nations, Ltd. NPM Opal Grand River Enterprises Six Nations, Ltd. NPM Seneca ITG Brands, LLC. PM Fortuna ITG Brands, LLC. PM Kool ITG Brands. LLC. PM Maverick ITG Brands, LLC. PM Rave ITG Brands, LLC. PM Rave (RYO) ITG Brands, LLC. PM Salem ITG Brands, LLC. PM Winston Japan Tobacco International USA, Inc. PM Export A Japan Tobacco International USA, Inc. PM LD by L. Ducat Japan Tobacco International USA, Inc. PM Wave Japan Tobacco International USA, Inc. PM Wings King Maker Marketing, Inc. PM ACE King Maker Marketing, Inc. PM Gold Crest Konci G&D Management Group (USA) Inc. PM ChungHwa Konci G&D Management Group (USA) Inc. PM Double Happiness Kretek International PM Taj Mahal KT&G Corp. NPM Carnival KT&G Corp. NPM Timeless Time KT&G Corp. NPM This Liggett Group PM Eve Liggett Group PM Grand Prix Liggett Group PM Liggett Select Liggett Group PM Montego Liggett Group PM Pyramid DISTRICT OF COLUMBIA TOBACCO DIRECTORY Last Updated 07/30/20 Page 2 of 4 MANUFACTURER PM/NPM BRAND FAMILY NASCO PM SF Ohserase Manufacturing LLC NPM Signal Peter Stokkebye Tobaksfabrik A/S PM Amsterdam Shag (RYO) Peter Stokkebye Tobaksfabrik A/S PM Danish Export (RYO) Peter Stokkebye Tobaksfabrik A/S PM London Export (RYO) Peter Stokkebye Tobaksfabrik A/S PM Norwegian Shag (RYO) Peter Stokkebye Tobaksfabrik A/S PM Stockholm Blend (RYO) Peter Stokkebye Tobaksfabrik A/S PM Turkish Export (RYO) Philip Morris USA Inc. -

Page 1 of 15
Updated September14, 2021– 9:00 p.m. Date of Next Known Updates/Changes: *Please print this page for your own records* If there are any questions regarding pricing of brands or brands not listed, contact Heather Lynch at (317) 691-4826 or [email protected]. EMAIL is preferred. For a list of licensed wholesalers to purchase cigarettes and other tobacco products from - click here. For information on which brands can be legally sold in Indiana and those that are, or are about to be delisted - click here. *** PLEASE sign up for GovDelivery with your EMAIL and subscribe to “Tobacco Industry” (as well as any other topic you are interested in) Future lists will be pushed to you every time it is updated. *** https://public.govdelivery.com/accounts/INATC/subscriber/new RECENTLY Changed / Updated: 09/14/2021- Changes to LD Club and Tobaccoville 09/07/2021- Update to some ITG list prices and buydowns; Correction to Pall Mall buydown 09/02/2021- Change to Nasco SF pricing 08/30/2021- Changes to all Marlboro and some RJ pricing 08/18/2021- Change to Marlboro Temp. Buydown pricing 08/17/2021- PM List Price Increase and Temp buydown on all Marlboro 01/26/2021- PLEASE SUBSCRIBE TO GOVDELIVERY EMAIL LIST TO RECEIVE UPDATED PRICING SHEET 6/26/2020- ***RETAILER UNDER 21 TOBACCO***(EFF. JULY 1) (on last page after delisting) Minimum Minimum Date of Wholesale Wholesale Cigarette Retail Retail Brand List Manufacturer Website Price NOT Price Brand Price Per Price Per Update Delivered Delivered Carton Pack Premier Mfg. / U.S. 1839 Flare-Cured Tobacco 7/15/2021 $42.76 $4.28 $44.00 $44.21 Growers Premier Mfg. -

Electronic Cigarette Inhalation Alters Innate Immunity and Airway Cytokines While Increasing the Virulence of Colonizing Bacteria
UC Santa Barbara UC Santa Barbara Previously Published Works Title Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. Permalink https://escholarship.org/uc/item/12r1c8pn Journal Journal of molecular medicine (Berlin, Germany), 94(6) ISSN 0946-2716 Authors Hwang, John H Lyes, Matthew Sladewski, Katherine et al. Publication Date 2016-06-01 DOI 10.1007/s00109-016-1378-3 Peer reviewed eScholarship.org Powered by the California Digital Library University of California J Mol Med (2016) 94:667–679 DOI 10.1007/s00109-016-1378-3 ORIGINAL ARTICLE Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria John H. Hwang1,2 & Matthew Lyes1,8 & Katherine Sladewski1 & Shymaa Enany3,1 & Elisa McEachern1,7 & Denzil P. Mathew1 & Soumita Das4 & Alexander Moshensky 1 & Sagar Bapat 5 & David T. Pride 4 & Weg M. Ongkeko 6 & Laura E. Crotty Alexander 1,2 Received: 10 August 2015 /Revised: 27 November 2015 /Accepted: 7 December 2015 /Published online: 25 January 2016 # Springer-Verlag Berlin Heidelberg (outside the USA) 2016 Abstract cells, suppress host defenses, and promote inflammation over Electronic (e)-cigarette use is rapidly rising, with 20 % of time, while also promoting virulence of colonizing bacteria. Americans ages 25–44 now using these drug delivery devices. E-cigarette users expose their airways, cells of host defense, Key message and colonizing bacteria to e-cigarette vapor (EV). Here, we & Acute exposure to e-cigarette vapor (EV) is cytotoxic to report that exposure of human epithelial cells at the air–liquid airway cells in vitro. -

Rotational Health Warnings for Cigarettes File No
UNITED STATES OF AMERICA FEDERAL TRADE COMMISSION WASHINGTON, D.C. 20580 Division of Advertising Practices May23,2008 MEMORANDUM TO: Public Records Office of the Secretary FROM: Sallie Schools Division of Advertising Practices SUBJECT: Rotational Health Warnings for Cigarettes File No. P854505 Please place the attached documents on the public record in the above-captioned matter. 1. August 16, 2007letter from Joseph T. Wong Esq. on behalf of Konci G & D Management Group (USA) Inc. to Sallie Schools. 2. September 4, 2007letter from Mary K. Engle to Joseph T. Wong Esq. on behalf of Konci G & D Management Group (USA) Inc. 3. August 20, 2007 letter from Hoo Tjhiang Han, Kretek International, to Sallie Schools. 4. September 5, 2007 letter from Mary K. Engle to Hoo Tjhiang Han, Kretek International. 5. September 6, 2007 letter from Hoo Tjhiang Han, Kretek International, to Sallie Schools. 6. September 7, 2007 letter from Mary K. Engle to Hoo Tjhiang Han, Kretek International. 7. August 23, 2007letter from Craig A. Koenigs on behalf of European Cigarette Imports, Inc. to Mary K. Engle. 8. September 10, 2007letter from Mary K. Engle to Craig A. Koenigs on behalf of European Cigarette Imports, Inc. 9. August 22, 2007 letter from Barry M. Boren on behalf of Tantus Tobacco, LLC to Mary K. Engle. 10. September 13, 2007 letter from Mary K. Engle to Barry M. Boren on behalf of Tantus Tobacco, LLC. 1 Public Records May23, 2008 Page 2 11. September 7, 2007 letter from Karen Kamperman, Tobacco Holdings, Inc. to Mary K. Engle. 12. September 13, 2007 letter from Mary K. -

Directory by Brand 02-27-06
3/2/2006 Brand Name Manufacturer C/RYO PM/NPM #117 National Tobacco Company RYO NPM 10/20's Dhanraj International C PM 10/20's Dhanraj International RYO PM 1st Choice R.J. Reynolds Tobacco Company C PM 4Aces Top Tobacco, LP RYO PM A Hint of Mint Sherman's 1400 Broadway NYC, Ltd. C PM A Touch of Clove Sherman's 1400 Broadway NYC, Ltd. C PM Ace King Maker Marketing C PM All Star Liberty Brands C PM All-American Value Philip Morris C PM Alpine Philip Morris C PM Always Save Liberty Brands C PM American Bison Wind River Tobacco Company C PM American Bison Wind River Tobacco Company RYO PM American Blend Mac Baren Tobacco Company RYO PM Ashford Von Eicken Group C PM Ashford Von Eicken Group RYO PM Athey Daughters & Ryan, Inc. RYO PM Austin R.J. Reynolds Tobacco Company C PM Bali Peter Stokkebye International, A/S RYO PM Barclay R.J. Reynolds Tobacco Company C PM Bargain Buy R.J. Reynolds Tobacco Company C PM Baron American Blend Farmer's Tobacco Co. of Cynthiana, Inc. C PM Basic Philip Morris C PM Beacon R.J. Reynolds Tobacco Company C PM Belair R.J. Reynolds Tobacco Company C PM Benson & Hedges Philip Morris C PM Best Buy Philip Morris C PM Best Choice Liberty Brands C PM Best Value R.J. Reynolds Tobacco Company C PM Black & Gold Sherman's 1400 Broadway NYC, Ltd. C PM Bonus Value R.J. Reynolds Tobacco Company C PM Boundary VIP Tobacco USA, Ltd. C PM Brand Marketing Liggett Group, Inc. -

Global Adult Tobacco Survey (GATS): Fact Sheet Templates
GTSS Global Adult Tobacco Survey (GATS) Tobacco Global Adult Global Adult Tobacco Survey (GATS) Analysis and Reporting Package Analysis and Reporting Package Global Adult Tobacco Survey (GATS) Fact Sheet Templates September 2020 Global Adult Tobacco Survey (GATS) Comprehensive Standard Protocol …………………………………………………………………………………………… GATS Questionnaire Core Questionnaire with Optional Questions Question by Question Specifications GATS Sample Design Sample Design Manual Sample Weights Manual GATS Fieldwork Implementation Field Interviewer Manual Field Supervisor Manual Mapping and Listing Manual GATS Data Management Programmer’s Guide to General Survey System Core Questionnaire Programming Specifications Data Management Implementation Plan Data Management Training Guide GATS Quality Assurance: Guidelines and Documentation GATS Analysis and Reporting Package Fact Sheet Templates Country Report: Tabulation Plan and Guidelines Indicator Definitions GATS Data Release and Dissemination Data Release Policy Data Dissemination: Guidance for the Initial Release of the Data Suggested Citation Global Adult Tobacco Survey Collaborative Group. Global Adult Tobacco Survey (GATS): Fact Sheet Templates. Atlanta, GA: Centers for Disease Control and Prevention, 2020. ii Acknowledgements GATS Collaborating Organizations • United States Centers for Disease Control and Prevention (CDC) • CDC Foundation • Johns Hopkins Bloomberg School of Public Health (JHSPH) • RTI International • World Health Organization (WHO) Financial Support Financial support was provided -

AHA Policy Statement Electronic Cigarettes
AHA Policy Statement Electronic Cigarettes A Policy Statement From the American Heart Association Aruni Bhatnagar, PhD, FAHA, Chair;·Laurie P. Whitsel, PhD; Kurt M. Ribisl, PhD; Chris Bullen, MBChB, PhD; Frank Chaloupka, PhD; Mariann R. Piano, PhD; Rose Marie Robertson, MD, FAHA; Timothy McAuley, PhD; David Goff, MD, PhD, FAHA; Neal Benowitz, MD; on behalf of the American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research or decades, advocacy for tobacco control has been a prior the current evidence, we provide policy recommendations in Fity of the American Heart Association (AHA). In partner key areas of tobacco control such as clean indoor air laws, ship with major public health organizations, the association taxation, regulation, preventing youth access, marketing and has made major strides in tobacco use prevention and cessa advertising to youth, counseling for cessation, surveillance, tion by prioritizing evidence-based strategies such as increas and defining e-cigarettes in state laws. The statement con ing excise taxes; passing comprehensive smoke-free air laws; cludes by outlining a future research agenda to further our facilitating US Food and Drug Administration (FDA) author understanding of this emerging area of tobacco control and ity to regulate tobacco, including comprehensive tobacco the impact of e-cigarettes on public health. cessation treatment within healthcare plans; and supporting adequate funding of comprehensive tobacco control programs E-Cigarettes or ENDS in different states. These tobacco control efforts have cut in The first concept of an electric•clgarette was patented in 1965 half the youth smoking rate from 1997 to 2007 and have saved by Herbert A Gilbert.4 Subsequently, an aerosolized, high >8 million lives in the past 50 years.