Immunizations Code List 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

And Gardasil
Advisory Commission on Childhood Vaccines (ACCV) Food and Drug Administration Update March 4, 2021 CDR Valerie Marshall, MPH, PMP, GWCPM Immediate Office of the Director Office of Vaccines Research and Review (OVRR) Center for Biologics Evaluation and Research (CBER) Food and Drug Administration (FDA) 1 Emergency Use Authorization for Vaccines . An Emergency Use Authorization (EUA) is a mechanism to facilitate the availability and use of medical countermeasures, including vaccines, during public health emergencies, such as the current COVID-19 pandemic. Under an EUA, the FDA may allow the use of unapproved medical products to prevent serious or life-threatening diseases or conditions when certain statutory criteria have been met, including that there are no adequate, approved, and available alternatives. Taking into consideration input from the FDA, manufacturers decide whether and when to submit an EUA request to FDA. Once submitted, FDA will evaluate an EUA request and determine whether the relevant statutory criteria are met, and review the scientific evidence about the vaccine that is available to FDA. 2 Requirements for the EUA . FDA evaluated nonclinical, clinical, and manufacturing data submitted by a vaccine manufacturer. For an EUA to be issued for a vaccine: . Adequate manufacturing information ensures quality and consistency . Vaccine benefits outweigh its risk based on data from at least one well-designed Phase 3 clinical study that in a compelling manner demonstrates: . Safety . Efficacy 3 Continued monitoring of COVID-19 Vaccines Authorized by FDA . USG Systems: . Vaccine Adverse Event Reporting System (VAERS) . Vaccine Safety Datalink (VSD), . Biologics Effectiveness and Safety (BEST) Initiative . Medicare Claims Data 4 EUA of COVID-19 Vaccines • On December 11, 2020, the FDA issued the first emergency use authorization (EUA) for Pfizer’s COVID-19 Vaccine. -

Technical Note the Use of Oral Cholera Vaccines for International Workers and Travelers to and from Cholera-Affected Countries November 2016
Global Task Force on Cholera Control (GTFCC) Oral Cholera Vaccine Working Group Technical Note The Use of Oral Cholera Vaccines for International Workers and Travelers to and from Cholera-Affected Countries November 2016 Background Three Oral Cholera Vaccines (OCVs) are currently pre-qualified by WHO: Dukoral® – a vaccine used mainly by travelers that includes killed whole cells and a component of the cholera toxin – and Shanchol™ and Euvichol®, which contain only killed whole cells. All three vaccines have a two-dose regimen with an interval between doses of two weeks or more (three doses for Dukoral® in children aged 2–5 years). All also have a good safety profile. Shanchol™ and Euvichol® are have the same formulation and comparable safety and immunogenicity profiles and are reformulated versions of Dukoral®.1,2 Unlike Dukoral®, Shanchol™ and Euvichol® do not require a buffer to administer. Shanchol™ has demonstrated longer term protection – a rather stable 65 – 67% from Year 2 to Year 5,3,4,5 as compared to Dukoral®.6 Concerning short-term protection – of most relevance to travelers – Dukoral® has been shown to provide 79-86% for three to six months in a series of studies,4,7,8,9 while the single published study of the short-term effectiveness of Shanchol™ found a similar rate (87%) over six months.10 Dukoral® has been shown to also confer significant short-term protection against enterotoxigenic E. coli (ETEC).11 Purpose of the Technical Note Concern has been raised in the past several years about the risk of international workers and other travelers getting cholera while in an endemic country or a country affected by an outbreak. -

Multiple Choice Questions on Immunisation Against Infectious Disease
Multiple choice questions on immunisation against infectious disease The Green Book Original version issued February 2008 Updated version January 2020 Multiple choice questions on immunisation against infectious disease About Public Health England Public Health England exists to protect and improve the nation’s health and wellbeing and reduce health inequalities. We do this through world-leading science, research, knowledge and intelligence, advocacy, partnerships and the delivery of specialist public health services. We are an executive agency of the Department of Health and Social Care, and a distinct delivery organisation with operational autonomy. We provide government, local government, the NHS, Parliament, industry and the public with evidence-based professional, scientific and delivery expertise and support. Public Health England Wellington House 133-155 Waterloo Road London SE1 8UG Tel: 020 7654 8000 www.gov.uk/phe Twitter: @PHE_uk Facebook: www.facebook.com/PublicHealthEngland Prepared by Drs Amelia Cummins, David Irwin, Sally Millership and Sultan Salimee, Consultants in Communicable Disease Control For queries relating to this document, please contact: Health Protection Team, Second Floor, Goodman House, Station Approach, Harlow, Essex CM20 2ET, Tel: 0300 303 8537, Fax: 0300 303 8541 [email protected] © Crown copyright 2020 You may re-use this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence v3.0. To view this licence, visit OGL. Where we have identified -
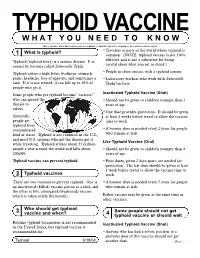
Typhoid Vaccine W H a T Y O U N E E D T O K N O W
TYPHOID VACCINE W H A T Y O U N E E D T O K N O W Many Vaccine Information Statements are available in Spanish and other languages. See www.immunize.org/vis. What is typhoid? •Travelers to parts of the world where typhoid is 1 common. (NOTE: typhoid vaccine is not 100% Typhoid (typhoid fever) is a serious disease. It is effective and is not a substitute for being caused by bacteria called Salmonella Typhi. careful about what you eat or drink.) Typhoid causes a high fever, weakness, stomach •People in close contact with a typhoid carrier. pains, headache, loss of appetite, and sometimes a •Laboratory workers who work with Salmonella rash. If it is not treated, it can kill up to 30% of Typhi bacteria. people who get it. Some people who get typhoid become “carriers,” Inactivated Typhoid Vaccine (Shot) who can spread the •Should not be given to children younger than 2 disease to years of age. others. •One dose provides protection. It should be given Generally, at least 2 weeks before travel to allow the vaccine people get time to work. typhoid from contaminated •A booster dose is needed every 2 years for people food or water. Typhoid is not common in the U.S., who remain at risk. and most U.S. citizens who get the disease get it Live Typhoid Vaccine (Oral) while traveling. Typhoid strikes about 21 million people a year around the world and kills about •Should not be given to children younger than 6 200,000. years of age. -

Vaccine Adjuvants Derived from Marine Organisms
biomolecules Review Vaccine Adjuvants Derived from Marine Organisms Nina Sanina Department of Biochemistry, Microbiology and Biotechnology, School of Natural Sciences, Far Eastern, Federal University, Sukhanov Str., 8, Vladivostok 690091, Russia; [email protected]; Tel.: +7-423-265-2429 Received: 10 July 2019; Accepted: 1 August 2019; Published: 3 August 2019 Abstract: Vaccine adjuvants help to enhance the immunogenicity of weak antigens. The adjuvant effect of certain substances was noted long ago (the 40s of the last century), and since then a large number of adjuvants belonging to different groups of chemicals have been studied. This review presents research data on the nonspecific action of substances originated from marine organisms, their derivatives and complexes, united by the name ‘adjuvants’. There are covered the mechanisms of their action, safety, as well as the practical use of adjuvants derived from marine hydrobionts in medical immunology and veterinary medicine to create modern vaccines that should be non-toxic and efficient. The present review is intended to briefly describe some important achievements in the use of marine resources to solve this important problem. Keywords: squalene; cucumariosides; chitosan; fucoidans; carrageenans; laminarin; alginate 1. Introduction The oil-in-water-based complete Freund’s adjuvant developed by Jules Freund and Katherine McDermott in 40s of last century is the first vaccine adjuvant. The basis of immune stimulation and provide immunologists with a way to stimulate the production of antibodies and cellular immune responses to weak antigens. This elaboration allowed to establish the basis of immune stimulation and provide immunologists with an instrument to stimulate the production of antibody and cellular immune responses to weak antigens. -

2021 Medicare Vaccine Coverage Part B Vs Part D
CDPHP® Medicare Advantage Vaccine Coverage Guide Part B (Medical) vs. Part D (Pharmacy) Medicare Part B (Medical): Medicare Part D (Pharmacy): Vaccinations or inoculations Vaccinations or inoculations are included when the administration is (except influenza, pneumococcal, reasonable and necessary for the prevention of illness. and hepatitis B for members at risk) are excluded unless they are directly related to the treatment of an injury or direct exposure to a disease or condition. • Influenza Vaccine (Flu) • BCG Vaccine • Pneumococcal Vaccine • Diphtheria/Tetanus/Acellular Pertussis Vaccine (ADACEL, (Pneumovax, Prevnar 13) BOOSTRIX, DAPTACEL, INFANRIX) • Hepatitis B Vaccine • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus (Recombivax, Engerix-B) Vaccine (KINRIX, QUADRACEL) for members at moderate • Diphtheria/Tetanus Vaccine (DT, Td, TDVAX, TENIVAC) to high risk • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus Vac • Other vaccines when directly cine/ Haemophilus Influenzae Type B Conjugate Vaccine (PENTACEL) related to the treatment of an • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus injury or direct exposure to a Vaccine/Hepatitis B Vaccine (PEDIARIX) disease or condition, such as: • Haemophilus Influenzae Type B Conjugate Vaccine (ActHIB, PedvaxHIB, • Antivenom Sera Hiberix) • Diphtheria/Tetanus Vaccine • Hepatitis A Vaccine, Inactivated (VAQTA) (DT, Td, TDVAX, TENIVAC) • Hepatitis B Vaccine, Recombinant (ENGERIX-B, RECOMBIVAX HB) • Rabies Virus Vaccine for members at low risk (RabAvert, -

Optimizing Vaccine Allocation for COVID-19 Vaccines Shows The
ARTICLE https://doi.org/10.1038/s41467-021-23761-1 OPEN Optimizing vaccine allocation for COVID-19 vaccines shows the potential role of single-dose vaccination ✉ Laura Matrajt 1 , Julia Eaton 2, Tiffany Leung 1, Dobromir Dimitrov1,3, Joshua T. Schiffer1,4,5, David A. Swan1 & Holly Janes1 1234567890():,; Most COVID-19 vaccines require two doses, however with limited vaccine supply, policy- makers are considering single-dose vaccination as an alternative strategy. Using a mathe- matical model combined with optimization algorithms, we determined optimal allocation strategies with one and two doses of vaccine under various degrees of viral transmission. Under low transmission, we show that the optimal allocation of vaccine vitally depends on the single-dose efficacy. With high single-dose efficacy, single-dose vaccination is optimal, preventing up to 22% more deaths than a strategy prioritizing two-dose vaccination for older adults. With low or moderate single-dose efficacy, mixed vaccination campaigns with com- plete coverage of older adults are optimal. However, with modest or high transmission, vaccinating older adults first with two doses is best, preventing up to 41% more deaths than a single-dose vaccination given across all adult populations. Our work suggests that it is imperative to determine the efficacy and durability of single-dose vaccines, as mixed or single-dose vaccination campaigns may have the potential to contain the pandemic much more quickly. 1 Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Research Center, Seattle, WA, USA. 2 School of Interdisciplinary Arts and Sciences, University of Washington, Tacoma, WA, USA. 3 Department of Applied Mathematics, University of Washington, Seattle, WA, USA. -

Routine Immunizations
Drug and Biologic Coverage Policy Effective Date ............................................... 7/1/2021 Next Review Date ......................................... 4/1/2022 Coverage Policy Number .................................. 9001 Routine Immunizations Table of Contents Related Coverage Resources Coverage Policy ................................................... 1 Preventive Care Services General Background ............................................ 2 Covid-19 Vaccine Coding/Billing Information .................................... 3 References .......................................................... 7 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event -
Integration of Typhoid Conjugate Vaccine in National Immunization Schedules: Opportunities and Challenges
Integration of typhoid conjugate vaccine in national immunization schedules: Opportunities and Challenges. Integration of typhoid9th conjugateInternational vaccine Conferencein national immunization on Typhoid schedules: and Opportunities and invasiveChallenges. NTS Disease 30/04 – 3/05, 2015. Nusa Dua, Bali Objective Review the existing clinical data on Vi conjugate vaccines, based on literature and our experience with Typbar-TCV to ascertain data sufficiency to assist global policy formualtion. Presentation Outline • Need for typhoid vaccine – Disease burden • Typhoid conjugate vaccines – Key considerations • Available data from typhoid conjugate vaccines (TCV) • Programmatic considerations • Integration of TCV into childhood immunization programs Typhoid epidemiology Disease Burden This disease is endemic in most developing countries. Cases/100,00 persons Highly Endemic >100 Endemic 10-100 Sporadic <10 21 million cases worldwide, mortality estimates of 216,000 to 600,000. http://www.who.int/immunization/topics/en/ http://www3.chu-rouen.fr/Internet/services/sante_voyages/pathologies/typhoide/ Age stratified disease burden 0.4 0.3 0.2 0.1 0 Proportion of Cases of Proportion Age groups Crump JA, et al. Bull World Health Organ 2004;82:346-353 Typhoid fever incidence – Asia and Africa • High incidence of typhoid fever in the region. • High incidence in urban slums; rates similar • Substantial regional variation in incidence. to those from Asia. • “Modified” Passive srvlnce. • Lower burden in rural children from Ghana (and Lwak, Kenya), compared to urban Ochiai RL, et al. Bull World Health Organ 2008;86:260-268. Breiman, RF et. al, PLoS One. 2012; 7(1): e29119. areas; regional differences Marks, F et. al, Emerg Infect Dis. 2010; 16(11): 1796–1797. -

History of Vaccination
SPECIAL FEATURE: PERSPECTIVE PERSPECTIVE SPECIAL FEATURE: History of vaccination Stanley Plotkin1 Department of Pediatrics, University of Pennsylvania, Philadelphia, PA 19104 Edited by Rino Rappuoli, Novartis Vaccines, Siena, Italy, and approved February 5, 2014 (received for review January 13, 2014) Vaccines have a history that started late in the 18th century. From the late 19th century, vaccines could be developed in the laboratory. However, in the 20th century, it became possible to develop vaccines based on immunologic markers. In the 21st century, molecular biology permits vaccine development that was not possible before. killed vaccines | proteins | live vaccine | genetic engineering One of the brightest chapters in the history of in humans (7). This idea played a role in the varicella vaccines were all made possible science is the impact of vaccines on human development of bacillus Calmette–Guérin through selection of clones by cell-culture longevity and health. Over 300 y have elapsed but is even more obvious in the selection of passage in vitro (17–21). In essence, passage since the first vaccine was discovered. In rhesus and bovine rotavirus strains to aid in cell culture leads to adaptation to growth a short article, it is not possible to do justice the creation of human rotavirus vaccines as in that medium, and the mutants best capa- to a subject that encompasses immunology, mentioned below under Reassortment. bleofgrowthhaveoftenlostormodifiedthe molecular biology, and public health, but sev- It was Pasteur and his colleagues who most genes that allow them to infect and spread eral more extensive sources are available clearly formulated the idea of attenuation and within a human host. -

1 Arizona Vaccine News Karen Lewis, M.D. Medical Director
Arizona Vaccine News Karen Lewis, M.D. Medical Director Arizona Immunization Program Office April 12, 2021 Douglas A. Ducey | Governor Cara M. Christ | MD, MS, Director _____________________________________________________________________________________________ 150 North 18th Avenue, Suite 120, Phoenix, AZ 85007-3247 P | 602-364-3630 F | 602-364-3285 W | azdhs.gov Health and Wellness for all Arizonans Newsletter Topics COVID-19 VACCINATIONS • Vaccine Effectiveness of mRNA COVID-19 Vaccines in Healthcare Personnel • How Well Do COVID-19 Vaccines Protect Against Variants? • Delayed Local Reactions to mRNA COVID-19 Vaccine • Overcoming (COVID-19) Vaccine Hesitancy Through Understanding and Trust • Can Colleges and Universities Require Student COVID-19 Vaccination? • Insights for Future Pediatric COVID-19 Vaccine Campaigns • World Health Organization COVID-19 Vaccine Global Clinical Trials Tracker VACCINES AND VACCINE-PREVENTABLE DISEASES • Decrease in Childhood Vaccinations Amid COVID-19 Pandemic • Parental Hesitancy About Routine Childhood and Influenza Vaccinations • Influenza Vaccine Effective Against Pediatric Hospitalizations and Emergency Visits • No Increased Risk of Stillbirth in Pregnant Women who Received Influenza or Tdap Vaccines • Recent History of Measles Outbreaks in Arizona • Cost of a Large Measles Outbreak in the U.S. • Updated CDC Compilation of Meningococcal Vaccination Recommendations • Declines in 4vHPV Vaccine Type Infections Among Females after Introduction of HPV Vaccine • More Provider Recommendations for HPV Vaccine -

First Responder Quick Guide
FIRST RESPONDERS: What you need to know Protect yourself and your loved ones Vaccinations are a critical component of your preparation and training to respond to emergencies and disaster events. Being up-to-date on your immunizations will prevent severe illness or the spread of disease to others. Review this quick guide for answers to some common questions about adult vaccination and recommendations for first responders. Download the complete First Responder Immunization Toolkit. Do I really need vaccines? All adults need vaccines to help protect against serious diseases that can result in severe illness, missed work, medical bills and an inability to care for their families. Adults may not have received all their vaccines during childhood. Some childhood vaccines do not offer protection into adulthood and a booster may be needed. Some vaccines are recommended based on age, job, lifestyle, or health condition. Getting vaccinated lowers the risk of getting sick and lowers the chance of spreading a serious disease to others including those that are most vulnerable to severe illness such as infants, older adults, and those with chronic health conditions or weakened immune systems. How well do adult vaccines work? Vaccines work with the body’s natural defenses to reduce the chances of getting certain diseases and suffering from complications. The amount of protection varies by vaccine and other factors such as age and health but immunizations are the best defense against many serious, sometimes deadly, diseases. The greatest risk of vaccine-preventable diseases occurs among those that are not vaccinated. Are adult vaccines safe? Vaccines are one of the safest ways to protect health.