Pharmacologyonline 1: 498-524
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Basis of Blood Glucose Regulation Asma Ahmed and Noman Khalique
Chapter Molecular Basis of Blood Glucose Regulation Asma Ahmed and Noman Khalique Abstract Blood glucose level is regulated by multiple pancreatic hormones, which regulate it by different pathways in normal and abnormal conditions by expressing or suppressing multiple genes or molecular or cellular targets. Multiple synthetic drugs and therapies are used to cure glucose regulatory problems, while many of them are used to cure other health issues, which arise due to disturbance in blood glucose regulations. Many new approaches are used for the development of phytochemical- based drugs to cure blood glucose regulation problems, and many of the compounds have been isolated and identified to cure insulin resistance or regulate beta cell function or glucose absorption in the guts or GLP-1 homoeostasis or two/more pathways (e.g., either cure hyperglycemia or raise insulin resistance or cure pan- creatic beta cell regeneration or augmentation of GLP-1, production of islet cell, production and increased insulin receptor signaling and insulin secretion or decreased insulin tolerance or gluconeogenesis and insulin-mimetic action or pro- duction of α-glucosidase and α-amylase inhibitor or conserve islet mass or activate protein kinase A (PKA) and extracellular signal regulated kinases (ERK) or activate AMPK and reduce insulin sensitivity or suppress α-glucosidase activity and activate AMPK and downstream molecules or prevents cell death of pancreatic β-cell and activates SIRT1 or lower blood glucose due to their insulin-like chemical structures or decrease lipid peroxidation. Keywords: genes, molecular and cellular targets, hormones, pathways 1. Introduction Blood glucose is regulated by the pancreatic hormones alone or in combination with other endocrine glands and all this is controlled by one or more gene or cellular or molecular targets. -

Inhaled Insulin: the Solution for Suboptimal Diabetes Control?
I EDITORIALS Inhaled insulin: the solution for suboptimal diabetes control? Stephanie A Amiel Stephanie A Amiel For nearly a century, we have been using insulin to action comparable to human soluble (regular) BSc MD FRCP, treat diabetes. Until recently, that insulin has been insulin rather than fast-acting analogues.10 In trials, RD Lawrence given by injection. In 2006, the first inhaled insulin, Exubera® is only ‘non-inferior’ to conventional (not Professor of Diabetic Exubera®, was licenced for use in Europe. The man- analogue) insulins, the latter not always used in Medicine, King’s ufacturers hoped for a warm welcome – the end of equivalent basal-bolus regimens11–14 and in type 2, College London School of Medicine injections and the dawn of a new era of enthusiastic slightly more effective than adding a second oral insulin takers with perfect diabetic control. The agent in very poorly controlled disease.15,16 It has not Clin Med National Institute for Health and Clinical Excellence been tested against fully flexible analogue regimens. 2007;7:430–2 (NICE) was more cautious and recommend that It is clear that inhaled insulin’s sole advantage over inhaled insulin only be used in the presence of diag- injected insulin is its route of delivery. nosed needle phobia (or severe intractable problems Exubera® has low bioavailability, minor and prob- with injection sites) and should be supervised by dia- ably reversible effects on lung function17 and a nat- betes specialists.1 True needle phobia is rare and ural lack of long-term safety data. Active smoking treatable by standard psychological techniques.2,3 On contraindicates its use because of increased bioavail- the NICE criteria, the market for inhaled insulin may abilty of inhaled insulin,18,19 while absorption may be small indeed. -

(12) United States Patent (10) Patent No.: US 7,700,128 B2 Doken Et Al
US007700128B2 (12) United States Patent (10) Patent No.: US 7,700,128 B2 Doken et al. (45) Date of Patent: Apr. 20, 2010 (54) SOLID PREPARATION COMPRISING AN 5,726,201 A * 3/1998 Fekete et al. ................ 514,471 INSULIN SENSITIZER, AN INSULIN 6,599,529 B1* 7/2003 Skinha et al. .... ... 424/458 SECRETAGOGUE ANDA 2003/0147952 A1* 8, 2003 Lim et al. ................... 424/468 POLYOXYETHYLENE SORBITAN EATTY 2003. O180352 A1 9, 2003 Patel et al. ACD ESTER 2004/O147564 A1 7/2004 Rao et al. 2004/0175421 A1* 9, 2004 Gidwani et al. ............. 424/465 (75) Inventors: Kazuhiro Doken, Osaka (JP); Tetsuya FOREIGN PATENT DOCUMENTS Kawano, Osaka (JP); Hiroyoshi EP O749751 A2 12/1996 Koyama, Osaka (JP): Naoru FR 2758461 7, 1998 Hamaguchi, Osaka (JP) GB 23990 15 9, 2004 JP 58065213 * 4f1983 (73) Assignee: Takeda Pharmaceutical Company WO WO95/12385 5, 1995 Limited, Osaka (JP) WO WO98, 11.884 3, 1998 WO WO 98,31360 7, 1998 (*) Notice: Subject to any disclaimer, the term of this WO WO 98/36755 8, 1998 patent is extended or adjusted under 35 WO WO98,57649 12/1998 U.S.C. 154(b) by 711 days. WO WO99.03476 1, 1999 WO WO99.03477 1, 1999 (21) Appl. No.: 10/544,581 WO WO99.03478 1, 1999 WO WOOO,274O1 5, 2000 WO WOOO.28989 5, 2000 (22) PCT Filed: Oct. 21, 2004 WO WOO1? 41737 A2 6, 2001 WO WOO1, 51463 T 2001 (86). PCT No.: PCT/UP2004/O15958 WO WOO2,04024 1, 2002 WO WO O2/O55009 T 2002 S371 (c)(1), WO WO 03/066028 A1 8, 2003 (2), (4) Date: Apr. -

WO 2016/118476 Al 28 July 2016 (28.07.2016) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/118476 Al 28 July 2016 (28.07.2016) W P O P C T (51) International Patent Classification: DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, A61K 38/46 (2006.01) HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (21) International Application Number: MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PCT/US2016/013847 PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (22) International Filing Date: SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, 19 January 2016 (19.01 .2016) TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (26) Publication Language: English GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, (30) Priority Data: TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, 62/105,342 20 January 2015 (20.01.2015) US TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, (71) Applicant: THE CHILDREN'S MEDICAL CENTER LV, MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, CORPORATION [US/US]; 300 Longwood Avenue, Bo SM, TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, ston, Massachusetts 021 15-5724 (US). -

203313Orig1s000 203314Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 203313Orig1s000 203314Orig1s000 PROPRIETARY NAME REVIEW(S) PROPRIETARY NAME MEMORANDUM Division of Medication Error Prevention and Analysis (DMEPA) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) *** This document contains proprietary information that cannot be released to the public*** Date of This Review: September 1, 2015 Application Type and Number: NDA 203313 Product Name and Strength: Ryzodeg 70/30 (insulin degludec and insulin aspart) injection, 100 units/mL Product Type: Combination (Drug + Device) Rx or OTC: Rx Applicant/Sponsor Name: Novo Nordisk Panorama #: 2015-1341036 DMEPA Primary Reviewer: Sarah K. Vee, PharmD DMEPA Team Leader: Yelena Maslov, PharmD Reference ID: 3813971 1 INTRODUCTION The Applicant submitted the proposed proprietary name, Ryzodeg on March 26, 2015 (b) (4) Division of Medication Error Prevention and Analysis (DMEPA) found the name conditionally acceptable in our previous review1 . On August 19, 2015, the Agency recommended that the Applicant consider including the modifier “70/30” to the proposed proprietary name to indicate the concentrations of the two insulins in the formulation. Since Ryzodeg is a mixed insulin formulation containing 70 % insulin degludec and 30 % insulin aspart, the addition of the modifier 70/30 would be consistent with current naming approach for mixed insulins. Thus, the Applicant submitted the name, Ryzodeg 70/30, for review on August 21, 2015. We note that the product characteristics are the same. This memorandum is to communicate that DMEPA finds the proposed proprietary name, Ryzodeg 70/30 (b) (4) is acceptable from both a misbranding and safety perspective. -

The Un-Design and Design of Insulin: Structural Evolution
THE UN-DESIGN AND DESIGN OF INSULIN: STRUCTURAL EVOLUTION WITH APPLICATION TO THERAPEUTIC DESIGN By NISCHAY K. REGE Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Biochemistry Dissertation Advisor: Dr. Michael A. Weiss CASE WESTERN RESERVE UNIVERSITY August, 2018 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of Nischay K. Rege candidate for the degree of Doctor of Philosophy*. Committee Chair Paul Carey Committee Member Michael Weiss Committee Member Faramarz Ismail-Beigi Committee Member George Dubyak Date of Defense: June 26th, 2018 *We also certify that written approval has been obtained for any proprietary material contained therein. Dedication This thesis is dedicated to my mother, Dipti, whose constant love and faith have never failed, to my father, Kiran, who taught me of the virtue of curiosity, and to my wife, Shipra, whose kindness and companionship have given me enough strength for eight lifetimes. i Table of Contents Dedication ..................................................................................................................................... i Table of Contents ......................................................................................................................... ii List of Tables ............................................................................................................................... v List of Figures ........................................................................................................................... -

Curriculum Vitae: Marc Stephen Rendell, Md
P a g e | 1 CURRICULUM VITAE: MARC STEPHEN RENDELL, M.D. ADDRESS: The Rose Salter Medical Research Foundation 34 Versailles Newport Coast, CA 92657-0065 clinic office 355 Placentia Avenue, Suite 308b Newport Beach, CA 92663 TELEPHONE: 402 -578-1580 HOSPITAL AND FACULTY APPOINTMENTS: 12/1977-6/1983 Active Staff and Assistant Professor Division of Endocrinology Department of Medicine The Johns Hopkins Hospital Baltimore, Maryland 6/1980-6/1983 Assistant Professor Division of Nuclear Medicine Department of Radiology The Johns Hopkins University School of Medicine Baltimore, Maryland 12/1977-6/1983 Chief, Endocrinology Director, Radioimmunoassay Laboratory The US Public Health Service Hospital Baltimore, Maryland 7/1983-11/1984 Director, Diabetes Institute City of Faith Medical and Research Center Associate Professor, Medicine and Pathology ORU School of Medicine Tulsa, Oklahoma 2/1985- 9/2016 Director, Creighton Diabetes Center Associate Professor of Medicine Associate Professor of Biomedical Sciences (1993-1995) P a g e | 2 Professor of Medicine and Biomedical Sciences (1996-2016 ) Creighton University School of Medicine Omaha, Nebraska 3/1999- Medical Director: Rose Salter Medical Research Foundation Baltimore, Maryland, Omaha, Nebraska, Newport Beach, California CLINICAL PRACTICE 12/1977-6/1983 Active Staff Division of Endocrinology Department of Medicine The Johns Hopkins Hospital Baltimore, Maryland 12/1977-6/1983 Chief, Endocrinology Director, Radioimmunoassay Laboratory The US Public Health Service Hospital Baltimore, Maryland 7/1983-11/1984 Director, Diabetes Institute City of Faith Medical and Research Center ORU School of Medicine Tulsa, Oklahoma 2/1985- 9/2016 Director, Creighton Diabetes Center Creighton University Medical Center Omaha, Nebraska 9/2016- Medical Director: Rose Salter Diabetes Center Newport Beach, California 1/2017- Telemedicine Physician Teladoc and MDLive EDUCATION: 9/1964-6/1968 B.S. -

Maikawa STM 2021.Pdf
SCIENCE TRANSLATIONAL MEDICINE | REVIEW DRUG DEVELOPMENT Copyright © 2021 The Authors, some rights reserved; Engineering biopharmaceutical formulations exclusive licensee American Association to improve diabetes management for the Advancement Caitlin L. Maikawa1, Andrea I. d’Aquino2, Rayhan A. Lal3,4,5, of Science. No claim 4,5 1,2,4,5,6 to original U.S. Bruce A. Buckingham , Eric A. Appel * Government Works Insulin was first isolated almost a century ago, yet commercial formulations of insulin and its analogs for hormone replacement therapy still fall short of appropriately mimicking endogenous glycemic control. Moreover, the controlled delivery of complementary hormones (such as amylin or glucagon) is complicated by instability of the pharmacologic agents and complexity of maintaining multiple infusions. In this review, we highlight the advantages and limitations of recent advances in drug formulation that improve protein stability and pharmacokinetics, prolong drug delivery, or enable alternative dosage forms for the management of diabetes. With controlled delivery, Downloaded from these formulations could improve closed-loop glycemic control. ENGINEERING OPPORTUNITIES TO IMPROVE DIABETES tive treatment with insulin alone is already highly burdensome and MANAGEMENT costly—requiring frequent glucose monitoring, mealtime insulin Over the past century, insulin replacement therapy has been impera- boluses, basal insulin delivery through infusion pumps or long-acting http://stm.sciencemag.org/ tive to saving lives and improving diabetes treatment outcomes. The analogs, and routine carbohydrate counting—and still does not truly administration of exogenous insulin prevents ketoacidosis, which recapitulate the complexities of metabolic control in nondiabetic was once a universally fatal condition. Although insulin has histor- individuals (Fig. 1B) (7). -

The Leading Source of Diabetes Business News It's Complicated
The Leading Source of Diabetes Business News It’s Complicated January/February 2011 • No. 105 The diabetes business used to be fairly straightforward. It’s a lot more complicated now, but that’s not a bad thing. Take insulin. After it was commercialized in the early 1920s, the goal was clear: sell more insulin. But look at today’s three major insulin makers: Eli Lilly, sanofi-aventis, and Novo Nordisk. For all three, to be sure, insulin is still preeminent. The diabetes divisions of Novo Nordisk and Lilly draw most of their revenue from human insulin and rapid-acting analogs, while sanofi-aventis’ blockbuster basal analog Lantus, as well as its mealtime insulins, continue to drive the bottom line. But all three companies have also developed (or are developing) GLP-1 analogs, Lilly has invested in oral drugs for type 2 diabetes (most recently through a major partnership with Boehringer Ingelheim), and the companies are also developing new therapeutic approaches for different stages of disease progression. The evolution of the insulin makers reflects broader industry trends. As our understanding of diabetes has expanded – and we dig deeper into the molecular complexities of the disease – it’s clear that single- focus large companies can no longer prosper. Ours is an era of individualized treatment that mixes and matches different drugs and technologies that try to meet the unique needs of every person with diabetes. Toward that end, companies are forming partnerships to find complementary therapies and development efforts that will create -

Various Emerging Trends in Insulin Drug Delivery Systems
British Journal of Pharmaceutical Research 5(5): 294-308, 2015, Article no.BJPR.2015.029 ISSN: 2231-2919 SCIENCEDOMAIN international www.sciencedomain.org Various Emerging Trends in Insulin Drug Delivery Systems Yasmeen1, T. Mamatha1*, Md. Zubair1, Sana Begum1 and Tayyaba Muneera1 1Department of Pharmaceutics, Sultan-ul-Uloom College of Pharmacy, affiliated to Jawaharlal Nehru Technological University Hyderabad, Road No.3, Banjara hills, Hyderabad 500 034, Telangana, India. Authors’ contributions This work was carried out in collaboration between all authors. Author TM designed the study, Authors Y and SB wrote the protocol, and wrote the first draft of the manuscript. Authors Md. Z and TM managed the literature searches. All authors read and approved the final manuscript. Article Information DOI:10.9734/BJPR/2015/12528 Editor(s): (1) Rafik Karaman, Bioorganic Chemistry, College of Pharmacy, Al-Quds University, USA. (2) Alyautdin Renad N, The Department of Pharmacology, I. M. Sechenov MSMU, Russia. Reviewers: (1) Anonymous, Italy. (2) Anonymous, Spain. (3) Anonymous, Norway. (4) Wei Wu, School of Pharmacy, Fudan University, China. (5) Anonymous, Malaysia. (6) Anastasia Thanopoulou, Diabetes Centre and Department of Internal Medicine, National University of Athens, Hippokration General Hospital, Athens, Greece. Complete Peer review History: http://www.sciencedomain.org/review-history.php?iid=883&id=14&aid=7718 Received 4th July 2014 th Review Article Accepted 28 November 2014 Published 9th January 2015 ABSTRACT Lowering of blood glucose level in patients can be achieved by insulin therapy as it plays a key role in the control of hyperglycaemia for type 1 diabetes. Insulin delivery systems that are currently available include syringes, infusion pumps, jet injectors and pens. -

The Prospect of Inhaled Insulin Therapy Via Vibrating Mesh Technology to Treat Diabetes
International Journal of Environmental Research and Public Health Review A Review: The Prospect of Inhaled Insulin Therapy via Vibrating Mesh Technology to Treat Diabetes Seán M. Cunningham and David A. Tanner * School of Engineering, Bernal Institute, University of Limerick, Limerick V94 T9PX, Ireland; [email protected] * Correspondence: [email protected]; Tel.: +35-3612-141-30 Received: 18 June 2020; Accepted: 31 July 2020; Published: 10 August 2020 Abstract: Background: Inhaled insulin has proven to be viable and, in some aspects, a more effective alternative to subcutaneous insulin. Past and present insulin inhaler devices have not found clinical or commercial success. Insulin inhalers create a dry powder or soft mist insulin aerosol, which does not provide the required uniform particle size or aerosol volume for deep lung deposition. Methods: The primary focus of this review is to investigate the potential treatment of diabetes with a wet insulin aerosol. Vibrating mesh nebulisers allow the passive inhalation of a fine wet mist aerosol for the administration of drugs to the pulmonary system in higher volumes than other small-volume nebulisers. Results: At present, there is a significant focus on vibrating mesh nebulisers from the pharmaceutical and biomedical industries for the systemic administration of pharmaceuticals for non-traditional applications such as vaccines or the treatment of diabetes. Systemic drug administration using vibrating mesh nebulisers leads to faster-acting pharmaceuticals with a reduction in drug latency. Conclusions: Systemic conditions such as diabetes, require the innovative development of custom vibrating mesh devices to provide the desired flow rates and droplet size for effective inhaled insulin administration. -
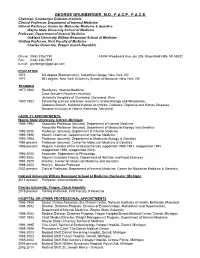
George Grunberger, M.D., F.A.C.P., F.A.C.E
GEORGE GRUNBERGER, M.D., F.A.C.P., F.A.C.E. Chairman, Grunberger Diabetes Institute Clinical Professor, Department of Internal Medicine Clinical Professor, Center for Molecular Medicine & Genetics Wayne State University School of Medicine Professor, Department of Internal Medicine Oakland University William Beaumont School of Medicine Visiting Professor, First Faculty of Medicine Charles University, Prague (Czech Republic) Phone: (248) 335-7740 43494 Woodward Ave, ste 208, Bloomfield Hills, MI 48302 Fax: (248) 338-7979 e-mail: [email protected] EDUCATION 1973 BA degree (Biochemistry), Columbia College, New York, NY 1977 MD degree, New York University School of Medicine, New York, NY TRAINING 1977-1980 Residency, Internal Medicine Case Western Reserve University University Hospitals of Cleveland, Cleveland, Ohio 1980-1983 Fellowship (clinical and basic research), Endocrinology and Metabolism, Diabetes Branch, National Institute of Arthritis, Diabetes, Digestive and Kidney Diseases National Institutes of Health, Bethesda, Maryland FACULTY APPOINTMENTS, Wayne State University, Detroit, Michigan 1986-1992 Associate Professor (tenured), Department of Internal Medicine Associate Professor (tenured), Department of Molecular Biology and Genetics 1992-2002 Professor (tenured), Department of Internal Medicine 1995-1996 Interim Chairman, Department of Internal Medicine 1992-1994 Professor (tenured), Department of Molecular Biology & Genetics 1994-present Professor (tenured), Center for Molecular Medicine & Genetics 1986-present Regular member