The Effects of Meldonium on the Renal Acute Ischemia/Reperfusion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Annual Report 2016
ANNUAL REPORT 2016 Facts and Introduction Corporate Manufacturing Products Markets Personnel Communication Figures speech Governance Policy Policy CONTENTS Facts and Figures Introduction speech by the Chairmen of the Council and Board Corporate Governance Manufacturing Products Markets Personnel Policy Communication Policy “Grindeks” Group – JSC “Grindeks” and five its subsidiary companies – JSC “Tallin Pharmaceutical plant” in Estonia, JSC “Kalceks” in Latvia, “Namu Apsaimniekošanas projekti” Ltd in Latvia, “Grindeks Rus” Ltd in Russia and “HBM Pharma” Ltd in Slovakia Core business – research, development, manufacturing and sales of original products, generics and active pharmaceutical ingredients Turnover – 105.4 million euros Net profit – 9.5 million euros Investments – 5.5 million euros Gross profit margin – 55% Net profit margin – 9% Export volume – 95.7 million euros Export countries – 71 Main markets – European Union, Russia and other CIS countries, USA, Canada, Japan and Vietnam FACTS AND FIGURES OF 2016 ANNUAL REPORT 2016 SALES OF FINAL DOSAGE FORMS Final dosage forms sales volume – 97.5 million euros Sales volume in Russia, other CIS countries and Georgia – 58.2 million euros Sales volume in the Baltic States and other countries – 39.3 million euros TOP products – meldonium, tegafurum, zopiclone, risperidone, ipidacrine, oxytocin, pain relief ointments and dietary supplementsApilak-Grindeks. SALES OF ACTIVE PHARMACEUTICAL INGREDIENTS (API'S) Sales volume of API's – 6.3 million euros Offered 17 API's The most demanded API's of “Grindeks” – oxytocin, zopiclone, droperidol, detomidine, and pimobendan. QUALITY AND ENVIRONMENTAL CONTROL “Good Manufacturing Practice” certificates for manufacturing of final dosage forms and active pharmaceutical ingredients ISO 9001; ISO 14001; LVS OHSAS 18001 certificates Russian ГОСТ ISO 9001-2011 certificate LVS EN ISO 50001:2012 Energy management certificate FACTS AND FIGURES OF 2016 ANNUAL REPORT 2016 achievements, the greater our ability to invest in further business growth. -

Maciej Łuczak Oszustwo Dopingowe W Sporcie Wyczynowym
ROZPRAWY NAUKOWE Akademii Wychowania Fizycznego we Wrocławiu 2018, 60, 118 – 134 Maciej Łuczak Akademia Wychowania Fizycznego w Poznaniu OSZUSTWO DOPINGOWE W SPORCIE WYCZYNOWYM WśRÓD KOBIET W LATACH 1950–2017 Cel badań. W artykule przedstawiono zjawisko dopingu kobiet w sporcie w XX i XXI w. Wśród sportsmenek sztuczne wspomaganie wykryto w latach 50. XX w. W niektórych krajach powstał system maskowania dopingu przez władze państwowe. Doświadczenie w zakresie opracowywania i podawania leków wspomagających miały laboratoria antydopingowe, m.in. w Kreischa w NRD. Stosowanie niedozwolonych praktyk ukazano na przykładzie NRD, RFN, ZSRR, Chin, USA, Kenii i Polski. Materiał i metody. Materiał badawczy został zinterpretowany przy użyciu metod stoso- wanych w naukach historycznych: indukcyjnej, dedukcyjnej, komparatystycznej i analizy litera- tury specjalistycznej. Do sformułowania ostatecznych wniosków wykorzystano metodę syntezy. Wyniki. Praktyki dopingowe miały miejsce w wielu krajach. Od 1956 r. notuje się stosowanie wspomagania organizmów sportsmenek za pomocą testosteronu. Z czasem doszły bardziej udo- skonalone niedozwolone środki oraz metody, takie jak np. doping ciążowy. Najbardziej zorganizo- wany doping pod kuratelą państwa miał miejsce w NRD, RFN, ZSRR, Chinach, USA, Kenii i w Polsce. Wnioski. W latach 50. XX w. zawodniczki – zwłaszcza w Związku Radzieckim – spo- radycznie przyjmowały testosteron oraz steroidy anaboliczno-androgenne. Później liczba stoso- wanych środków dopingujących systematycznie rosła. Na większą skalę zaczęto je przyjmować dopiero w latach 70. i 80. XX w. Próbą zapanowania nad tym zjawiskiem są badania antydopin- gowe, jednak chęć zwycięstwa często przeważa nad zdrowym rozsądkiem. Słowa kluczowe: sport, doping, historia, kobiety WprowadzEniE Doping w sporcie znany jest od bardzo dawna. Zapewne byłby łatwiejszy do wykrycia, gdyby nie korzyści płynące z niego dla firm farmaceutycznych, lekarzy, trenerów, za- wodników, federacji sportowych oraz polityków i rządów państw. -
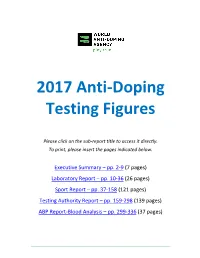
2017 Anti-Doping Testing Figures Report
2017 Anti‐Doping Testing Figures Please click on the sub‐report title to access it directly. To print, please insert the pages indicated below. Executive Summary – pp. 2‐9 (7 pages) Laboratory Report – pp. 10‐36 (26 pages) Sport Report – pp. 37‐158 (121 pages) Testing Authority Report – pp. 159‐298 (139 pages) ABP Report‐Blood Analysis – pp. 299‐336 (37 pages) ____________________________________________________________________________________ 2017 Anti‐Doping Testing Figures Executive Summary ____________________________________________________________________________________ 2017 Anti-Doping Testing Figures Samples Analyzed and Reported by Accredited Laboratories in ADAMS EXECUTIVE SUMMARY This Executive Summary is intended to assist stakeholders in navigating the data outlined within the 2017 Anti -Doping Testing Figures Report (2017 Report) and to highlight overall trends. The 2017 Report summarizes the results of all the samples WADA-accredited laboratories analyzed and reported into WADA’s Anti-Doping Administration and Management System (ADAMS) in 2017. This is the third set of global testing results since the revised World Anti-Doping Code (Code) came into effect in January 2015. The 2017 Report – which includes this Executive Summary and sub-reports by Laboratory , Sport, Testing Authority (TA) and Athlete Biological Passport (ABP) Blood Analysis – includes in- and out-of-competition urine samples; blood and ABP blood data; and, the resulting Adverse Analytical Findings (AAFs) and Atypical Findings (ATFs). REPORT HIGHLIGHTS • A analyzed: 300,565 in 2016 to 322,050 in 2017. 7.1 % increase in the overall number of samples • A de crease in the number of AAFs: 1.60% in 2016 (4,822 AAFs from 300,565 samples) to 1.43% in 2017 (4,596 AAFs from 322,050 samples). -

<Vorname> <Nachname>
To the INTERNATIONAL SKI FEDERATION - Members of the FIS Council Blochstrasse 2 - National Ski Associations 3653 Oberhofen/Thunersee - Committee Chairwomen/Chairmen Switzerland Tel +41 33 244 61 61 Fax +41 33 244 61 71 Oberhofen, 4th June 2019 Summary of the FIS Council Meeting, 2nd June 2019, Cavtat-Dubrovnik (CRO) Dear Mr. President, Dear Ski Friends, In accordance with art. 32.2 of the FIS Statutes we have pleasure in sending you the Summary of the most important decisions from the FIS Council Meeting which took place on 2nd June 2019 in Cavtat-Dubrovnik (CRO). 1. Members present The following elected Council Members were present at the meeting in Cavtat- Dubrovnik (SUI) on Sunday, 2nd June 2019: President Gian Franco Kasper, Vice-Presidents Mats Arjes, Janez Kocijancic, Aki Murasato and Patrick Smith, Members: Andrey Bokarev, Steve Dong Yang, Dean Gosper, Alfons Hörmann, Hannah Kearney (Athletes’ Commission Representative), Roman Kumpost, Dexter Paine, Flavio Roda, Erik Roeste, Konstantin Schad (Athletes’ Commission Representative), Peter Schröcksnadel, Martti Uusitalo (by ‘phone), Eduardo Valenzuela and Michel Vion. Secretary General Sarah Lewis 2. Minutes from the Council Meeting in Oberhofen (SUI) November 2019 With the inclusion of a correction in the report on Tokyo 2020 (reference to currency Japanese yen instead of US dollars) requested by Vice-President Aki Murasato, the minutes from the Council Meeting in Oberhofen (SUI) from 16th November 2018 and the Gathering in Åre (SWE) from 13th February were approved. 3. The FIS World -

The Effects of Meldonium on the Acute Ischemia/Reperfusion Liver Injury in Rats
www.nature.com/scientificreports OPEN The efects of meldonium on the acute ischemia/reperfusion liver injury in rats Siniša Đurašević1*, Maja Stojković2, Jelena Sopta2, Slađan Pavlović3, Slavica Borković‑Mitić3, Anđelija Ivanović3, Nebojša Jasnić1, Tomislav Tosti4, Saša Đurović5, Jelena Đorđević1 & Zoran Todorović2,6 Acute ischemia/reperfusion (I/R) liver injury is a clinical condition challenging to treat. Meldonium is an anti‑ischemic agent that shifts energy production from fatty acid oxidation to less oxygen‑ consuming glycolysis. Thus, we investigated the efects of a 4‑week meldonium pre‑treatment (300 mg/kg b.m./day) on the acute I/R liver injury in Wistar strain male rats. Our results showed that meldonium ameliorates I/R‑induced liver infammation and injury, as confrmed by liver histology, and by attenuation of serum alanine‑ and aspartate aminotransferase activity, serum and liver high mobility group box 1 protein expression, and liver expression of Bax/Bcl2, haptoglobin, and the phosphorylated nuclear factor kappa‑light‑chain‑enhancer of activated B cells. Through the increased hepatic activation of the nuclear factor erythroid 2‑related factor 2, meldonium improves the antioxidative defence in the liver of animals subjected to I/R, as proved by an increase in serum and liver ascorbic/dehydroascorbic acid ratio, hepatic haem oxygenase 1 expression, glutathione and free thiol groups content, and hepatic copper‑zinc superoxide dismutase, manganese superoxide dismutase, catalase, glutathione peroxidase, and glutathione reductase activity. Based on our results, it can be concluded that meldonium represent a protective agent against I/R‑induced liver injury, with a clinical signifcance in surgical procedures. Acute ischemia/reperfusion (I/R) refers to a temporary abolishment of blood fow during surgical interventions, followed by its re-establishment once an intervention is fnished 1. -

Uww Ordinary Congress Mâcon (Fra)
UWW ORDINARY CONGRESS MÂCON (FRA) Parc des Expositions – Le Spot 4 September 2016 - 9am *** MINUTES Voters attending the Congress (Total : 119) : Bureau members in attendance: 1. Nenad LALOVIC President 2. Ahmet AYIK Vice-president 3. Stan DZIEDZIC Vice-president 4. Mikhail MAMIASHVILI Vice-president 5. Akhroldjan RUZIEV Vice-president 6. Nataliya YARIGUINA Vice-president 7. Michel DUSSON Secretary General 8. Namig ALIYEV Member 9. Zamel Sayyaf AL SHAHRANI Member 10. Karl-Martin DITTMANN Member 11. Pedro GAMA FILHO Member 12. Theodoros HAMAKOS Member 13. Ik-Jong KIM Member 14 Fouad MESKOUT Member and President of UWW-Africa 15 Marina PELLICONE Member 16. Daulet TURLYKHANOV Member 17. Tzeno TZENOV Member and President of UWW-Europe 18. Rodica YAKSI Member 19. Carol HUYNH President of the Athletes Commission Presidents of continental Councils: Francisco LEE LOPEZ President, UWW-Americas John TARKONG President, UWW-Oceania Dr Chang-Kew KIM President, UWW-Asia United World Wrestling Ordinary Congress 2016 - Minutes Page 1 | 10 African Continent (Total : 21) 1. Algeria 8. Central Africa Republic 15. Mauritania 2. Angola 9. Egypt 16. Mauritius 3. Botswana 10. Ghana 17. Morocco 4. Burkina Faso 11. Guinea 18. South Africa 5. Burundi 12. Kenya 19. Senegal 6. Democratic Republic 13. Madagascar 20. Sierra Leone of Congo 14. Mali 21. Zimbabwe 7. Côte d’Ivoire American Continent (Total : 22) 1. Argentina 9. Cuba 17. Peru 2. Bahamas 10. Ecuador 18. Puerto Rico 3. Barbados 11. El Salvador 19. Trinidad & Tobago 4. Brazil 12. Guatemala 20. United States 5. Canada 13. Honduras 21. Venezuela 6. Chili 14. Mexico 22. Virgin Islands 7. -

Summary of Product Characteristics 1. Name Of
SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Meldonium Pharmexon 500 mg hard capsules 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each hard capsule contains 500 mg of meldonium dihydrate. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Hard capsule. White hard gelatin capsules. The content – white crystalline powder with faint odor. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Adjuvant treatment of mild chronic cardiac insufficiency. 4.2 Posology and method of administration Posology Adults The usual daily dose is 500-1000 mg of meldonium. The daily dose may be divided into two single doses. The maximum daily dose is 1000 mg. The treatment course varies from 4 to 6 weeks. Elderly No specific recommendation for the use in this age group. Elderly patients with hepatic and/or renal impairment may require lower doses (see section 4.4). Patients with hepatic and/or renal disorders As the medicinal product is eliminated through the kidney, in patients with renal disorders, as well as those with liver diseases, doses should be reduced (see section 4.4). Paediatric population Due to lack of data on the safety and efficacy, the medicinal product is not recommended for use in children. Method of administration For oral administration. It is advised to use meldonium in the morning because of the possible stimulating effect. In order to avoid gastrointestinal disturbances the medicinal product can be taken with food. 4.3 Contraindications Hypersensitivity to the active substance or to any of the excipients listed in section 6.1. 4.4 Special warnings and precautions for use Patients with chronic liver and renal diseases should use this medicinal product carefully because no studies were held to find out the effects on elevated risk patients. -

April 2020 Sanctions List Full
GLOBAL LIST OF INELIGIBLE PERSONS Period of Date of Discipline Date of Ineligibility Lifetime Infraction Name Nationality Role Sex Discipline 2 Sanction Disqualification ADRV Rules ADRV Notes Description Birth 1 Infraction until Ban? Type of results ABAKUMOVA, Maria 15/01/1986 RUS athlete F Javelin Throws 21/08/2008 4 years 17/05/2020 From 21.08.08 to No Doping Presence,Use Dehydrochlormethyltestost In competition test, XXIX Olympic ineligibility 20.08.12 erone games, Beijing, CHN ABDOSH, Ali 25/08/1987 ETH athlete M Long Distance 24/12/2017 4 years 04/02/2022 Since 24-12-2017 No Doping Presence,Use Salbutamol In competition test, 2017 Baoneng (3000m+) ineligibility Guangzhou Huangpu Marathon , Guangzhou, CHN ABDUL SHAHID (NASERA), Haidar 13/01/1981 IRQ athlete M Throws 08/03/2019 4 years 05/05/2023 Since 08.03.19 No Doping Presence,Use Metandienone In competition test, Iraqi ineligibility Championships, Baghdad, IRQ ACHERKI, Mounir 09/02/1981 FRA athlete M 1500m Middle Distance 01/01/2014 4 years 15/04/2021 Since 01-01-2014 No Doping Use,Possessio Use or Attempted Use by an IAAF Rule 32.2(b) Use of a prohibited (800m-1500m) ineligibility n Athlete of a Prohibited substance Substance or a Prohibited IAAF Rule 32.2(f) Possession of a Method, Possession of a prohibited substance Prohibited Substance or a Prohibited Method ADAMCHUK, Mariya 29/05/2000 UKR athlete F Long Jump Jumps 03/06/2018 4 years 16/08/2022 Since 03.06.18 No Doping Presence,Use Trenbolone, DMBA & ICT, Ukrainian club U20 ineligibility Methylhexaneamine Championships', Lutsk, UKR ADEKOYA, Kemi 16/01/1993 BRN athlete F 400m Sprints (400m or 24/08/2018 4 years 25/11/2022 Since 24.08.18 No Doping Presence,Use Stanozolol Out-of-competition test, Jakarta, IDN Hurdles less) ineligibility ADELOYE, Tosin 07/02/1996 NGR athlete F 400m Sprints (400m or 24/07/2015 8 years 23/07/2023 Since 24-07-2015 No Doping Presence,Use Exogenous Steroids In competition test, Warri Relays - less) ineligibility (2nd CAA Super Grand Prix , Warri, NGR ADRV) ADLI SAIFUL, Muh. -

Harmonization of Anti-Doping Policies Within the International Scenario: an Impossible Challenge?
Rivista Internazionale di Diritto ed Etica dello Sport 6,7,8 (2016) Submitted 16/04/2017; Published 03/05/2017 Harmonization of anti-doping policies within the international scenario: an impossible challenge? Michael Geistlinger University of Salzburg, Austria [email protected] 1. Introductory Remarks In 1947 the General Assembly of the United Nations established the International Law Commission (ILC) to undertake the mandate of the Assembly, under article 13 (1) (a) of the Charter of the United Nations to “initiate studies and make recommendations for the purpose of ... encouraging the progressive development of international law and its codification”.1 The first Statute of this Commission, which was attached to the respective General Assembly’s Resolution, provided for fifteen members of this Commission who had to be persons of recognized competence in international law.2 There were topics on the Agenda of the ILC, which could be dealt with in a very short period of time, such as the Fundamental Rights and Duties of States or the Formulation of the Nürnberg Principles, both in 1949 – 1950.3 But, whenever it came to substantial issues of public international law, the ILC needed nearly a decade or even well more than a decade for concluding a report and eventually draft articles as a basis for a later convention. Thus, for example, the codification of the law of international treaties stayed on the Agenda of the ILC from 1950 – 1966, treaties concluded between states and international organizations or between two or more international organizations were dealt with by the ILC from 1971 – 1982. -

M. Sharapova and the Meldonium Scandal: Anti-Crisis Communications
SHS Web of Conferences 110, 04009 (2021) https://doi.org/10.1051/shsconf/202111004009 ICEMT 2021 M. Sharapova and the meldonium scandal: anti- crisis communications in personal branding Alexandra Zaharova1,*, and Elena Karmalova2 ¹Novosibirsk State Technical University», Russia ²Federal State Budget Educational Institution of Higher Education «Saint-Petersburg State University of Economics», Russia Abstract. The article simulates and analyzes a practical case of building anti-crisis communications by tennis player Maria Sharapova in the meldonium scandal. The factors of the development of the crisis are analyzed, strategic and tactical mistakes and blunders are revealed, strategic and tactical successes and achievements are indicated. Anti-crisis management and anti-crisis communications in the situation of the COVID-19 pandemic have become especially relevant for business, the social sphere and society as a whole. Before the pandemic crisis, the problem was perceived as important primarily by businesses and structures associated with potential emergencies. In the field of personal branding, anti-crisis communications are generally poorly understood, but today the need for anti-crisis programs and measures is not disputed in any area of activity. The successful anti-crisis case “Maria Sharapova and meldonium”, modeled and analyzed, and can become a successful algorithm for practical actions both in the field of anti-crisis communications of personal branding and in the field of sports anti-crisis. The latter area seems to be very crisis-intensive for various reasons. To date, there are no detailed studies devoted to the problem of anti-crisis communications in the field of personal branding or sports. We can only talk about a fairly well developed area of research - anti-crisis communications in business. -

Page 1 the Official Channel of the Athletes Movement® ΛC 1
Athletes Channel What’s really at stake? Sun Yang vs WADA ATHLETES C H A N N E L What’s really at stake? Sun Yang vs WADA Steven V. Selthoffer Athletes Channel September 12, 2019 20:12 pm GMT +1 (Lausanne, SUI) – New revelations have come to light in the Sun Yang case from Chinese state run media Xinhuanet in the past two days upending global public opinion that only one member of the three person testing team was trained to perform the tests on the swimmer, also calling into question the ages of the other two anti-doping DCOs and their medical training according to Sun’s attorney Zhang Qihuai, Chinese Media: Tester in Sun Yang Case was Untrained Classmate of Main Officer, Jared Anderson, SwimSwam, August 28, 2019. In a second report this time from Channel News Asia August 27 states that there is possible security video footage of the anti-doping mission that night. Sun states (Weibo) “There is something I can’t say, I can’t make the truth public… But fortunately the surveillance cameras have recorded everything, otherwise I won’t be able to defend myself against irresponsible accusations.” And it was announced earlier from the Court of Arbitration and Sport, Lausanne, SUI on August 20, 2019 that the Sun Yang, CHN and FINA vs WADA CAS case will be held after October 2019 in public with full media in attendance. That changes the dynamics. This a major victory for transparency, athletes rights and will force issues out into the open that WADA, the IOC and others have been reluctant to address. -

Attaining Olympus: a Critical Analysis of Performance-Enhancing Drug Law and Policy for the 21St Century
Franco Book Proof (Do Not Delete) 4/16/19 11:35 PM ATTAINING OLYMPUS: A CRITICAL ANALYSIS OF PERFORMANCE-ENHANCING DRUG LAW AND POLICY FOR THE 21ST CENTURY ALEXANDRA M. FRANCO1 ABSTRACT While high-profile doping scandals in sports always garner attention, the public discussion about the use of performance-enhancing substances ignores the growing social movement towards enhancement outside of sports. This Article discusses the flaws in the ethical origins and justifications for modern anti-doping law and policy. It analyzes the issues in the current regulatory scheme through its application to different sports, such as cycling and bodybuilding. The Article then juxtaposes those issues to general anti-drug law applicable to non-athletes seeking enhancement, such as students and professionals. The Article posits that the current regulatory scheme is harmful not only to athletes but also to people in general—specifically to their psychological well-being—because it derives from a double social morality that simultaneously shuns and encourages the use of performance-enhancing drugs. I. INTRODUCTION “Everybody is going to do what they do.” — Phil Heath, Mr. Olympia champion.2 The relationship between performance-enhancing drugs and American society has been problematic for the past several decades. High- profile doping scandals regularly garner media attention—for example, 1. © Alexandra M. Franco, J.D. The Author is an Affiliated Scholar at the Institute for Science, Law and Technology at IIT Chicago-Kent College of Law. She previously worked as a Judicial Law Clerk for the Honorable Franklin U. Valderrama in the Circuit Court of Cook County, Illinois (the views expressed in this Article are solely those of the Author, and do not represent those of Equal Justice Works or Cook County).