Central Serous Chorioretinopathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Visual Performance and Metamorphopsia of Patients with Macular Holes
CLINICAL SCIENCES The Visual Performance and Metamorphopsia of Patients With Macular Holes Yoshihiro Saito, MD; Yoshiko Hirata, MD; Atsushi Hayashi, MD; Takashi Fujikado, MD; Masahito Ohji, MD; Yasuo Tano, MD Background: Most patients attain better visual acuity divided the subjective changes into 2 types of metamor- with the elimination of metamorphopsia after success- phopsia; of the 54 eyes, pincushion distortion (bowed ful closure of a macular hole (MH) by vitrectomy. toward the center) was found in 33 (61%), and unpat- terned distortion (no specific pattern) was found in 21 Objective: To determine the presurgical visual func- (39%). Pincushion distortion was significantly associ- tion of eyes with an MH. ated with an MH of shorter duration (#6 months) (P = .03) and an early stage (stage 2) of MH formation Methods: We examined 54 eyes of 51 patients with an (P = .02). A scotoma was hard to detect, and patients had idiopathic MH using the Amsler chart. We evaluated difficulty describing their scotomata and distortions. In the types of subjective metamorphopsia and compared the montage test, patients with early MHs chose por- them with the clinical factors associated with MHs. In a traits modified with a pincushion type of distortion. prospective study, we performed a montage test on a separate group of 16 patients with unilateral idiopathic Conclusions: We found concentric pincushion meta- MHs. The patients were asked to choose, while viewing morphopsia without subjective scotomata, which we sug- with their better eye, the computer-modified picture gest arises from an eccentric displacement of the photo- that best matched the unmodified image seen by the eye receptors. -

Vitreomacular Traction Syndrome
RETINA HEALTH SERIES | Facts from the ASRS The Foundation American Society of Retina Specialists Committed to improving the quality of life of all people with retinal disease. Vitreomacular Traction Syndrome SYMPTOMS IN DETAIL The vitreous humor is a transparent, gel-like material that fills the space within the eye between the lens and The most common symptoms the retina. The vitreous is encapsulated in a thin shell experienced by patients with VMT syndrome are: called the vitreous cortex, and the cortex in young, healthy • Decreased sharpness of vision eyes is usually sealed to the retina. • Photopsia, when a person sees flashes of light in the eye As the eye ages, or in certain pathologic conditions, the vitreous cortex can • Micropsia, when objects appear pull away from the retina, leading to a condition known as posterior vitreous smaller than their actual size detachment (PVD). This detachment usually occurs as part of the normal • Metamorphopsia, when vision aging process. is distorted to make a grid of There are instances where a PVD is incomplete, leaving the vitreous straight lines appear wavy partially attached to the retina, and causing tractional (pulling) forces that or blank can cause anatomical damage. The resulting condition is called vitreomacular Some of these symptoms can be traction (VMT) syndrome. mild and develop slowly; however, VMT syndrome can lead to different maculopathies or disorders in the chronic tractional effects can macular area (at the center of the retina), such as full- or partial-thickness lead to continued visual loss macular holes, epiretinal membranes, and cystoid macular edema. These if left untreated. -

Myopic Choroidal Neovascularisation: Current Concepts and Update On
BJO Online First, published on July 1, 2014 as 10.1136/bjophthalmol-2014-305131 Review Br J Ophthalmol: first published as 10.1136/bjophthalmol-2014-305131 on 1 July 2014. Downloaded from Myopic choroidal neovascularisation: current concepts and update on clinical management Tien Y Wong,1 Kyoko Ohno-Matsui,2 Nicolas Leveziel,3 Frank G Holz,4 Timothy Y Lai,5 Hyeong Gon Yu,6 Paolo Lanzetta,7 Youxin Chen,8 Adnan Tufail9 For numbered affiliations see ABSTRACT PATHOGENESIS OF MYOPIC CNV end of article. Choroidal neovascularisation (CNV) is a common vision- Several theories have been proposed to explain the threatening complication of myopia and pathological development of myopic CNV, reviewed in detail Correspondence to 4 Dr Tien Y Wong, Singapore Eye myopia. Despite significant advances in understanding elsewhere. The mechanical theory is based on the Research Institute, Singapore the epidemiology, pathogenesis and natural history of assumption that the progressive and excessive National Eye Centre, National myopic CNV, there is no standard definition of myopic elongation of the anteroposterior axis causes a University of Singapore, 11 CNV and its relationship to axial length and other mechanical stress on the retina, leading to an imbal- Third Hospital Avenue, Singapore 168751, Singapore; myopic degenerative changes. Several treatments are ance between pro-angiogenic and anti-angiogenic 7 [email protected] available to ophthalmologists, but with the advent of factors, resulting in myopic CNV. In support, the new therapies there is a need for further consensus and presence of lacquer cracks has been shown to be a Received 7 March 2014 clinical management recommendations. -

Cholesterol Dyshomeostasis and Age Related Macular Degeneration Bhanu Chandar Dasari
University of North Dakota UND Scholarly Commons Theses and Dissertations Theses, Dissertations, and Senior Projects 1-1-2012 Cholesterol Dyshomeostasis And Age Related Macular Degeneration Bhanu Chandar Dasari Follow this and additional works at: https://commons.und.edu/theses Recommended Citation Dasari, Bhanu Chandar, "Cholesterol Dyshomeostasis And Age Related Macular Degeneration" (2012). Theses and Dissertations. 1235. https://commons.und.edu/theses/1235 This Thesis is brought to you for free and open access by the Theses, Dissertations, and Senior Projects at UND Scholarly Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. CHOLESTEROL DYSHOMEOSTASIS AND AGE RELATED MACULAR DEGENERATION by Bhanu Chandar Dasari Bachelor of Science, Kakatiya University, 1999 Master of Science, University of Pune, 2001 A Dissertation Submitted to the Graduate Faculty of the University of North Dakota in partial fulfillment of the requirements for the degree of Doctor of Philosophy Grand Forks, North Dakota May 2012 This dissertation, submitted by Bhanu Chandar Dasari in partial fulfillment of the requirements for the Degree of Doctor of Philosophy from the University of North Dakota, has been read by the Faculty Advisory Committee under whom the work has been done and is hereby approved. __________________________________ Othman Ghribi, Ph.D. __________________________________ Brij B. Singh, Ph.D. __________________________________ Colin K. Combs, Ph.D. __________________________________ James E. Porter, Ph.D. __________________________________ Saobo Lei, Ph.D. This dissertation is being submitted by the appointed advisory committee as having met all of the requirements of the Graduate School at the University of North Dakota and is hereby approved. -

Retinal Contraction and Metamorphopsia Scores in Eyes with Idiopathic Epiretinal Membrane
Retinal Contraction and Metamorphopsia Scores in Eyes with Idiopathic Epiretinal Membrane Eiko Arimura, Chota Matsumoto, Sachiko Okuyama, Sonoko Takada, Shigeki Hashimoto, and Yoshikazu Shimomura PURPOSE. Using M-CHARTS (Inami Co., Tokyo, Japan), which assessment charts, M-CHARTS (Inami Co., Tokyo, Japan), with were developed by the authors to measure metamorphopsia, which it is possible to quantify the degree of metamorphopsia and image-analysis software, which was developed to quantify in patients with disease involving the macula.2,3 It is known retinal contraction, the authors investigated the relationship that one of the main causes of metamorphopsia in individuals between the degree of retinal contraction and the degree of with macula diseases is disarray of the photoreceptors in the metamorphopsia in eyes with idiopathic epiretinal membrane sensory retina. Especially in cases of ERM, the photoreceptors (ERM). and/or the outer segments are dislocated due to the contrac- METHODS. This study was conducted in 29 eyes with ERM (29 tion of the proliferating membranes. However, to date there patients, 20 women; mean age, 62.1 Ϯ 8.6 years) observed for have been no detailed long-term follow-up studies to evaluate at least 3 years (mean, 3.55 Ϯ 0.6 years) after diagnosis. Hori- the relationship between the progression of retinal contraction zontal (MH) and vertical (MV) metamorphopsia scores were and change in metamorphopsia. We therefore decided to con- obtained with the M-CHARTS. Horizontal and vertical retinal duct this study to investigate the relationship between the contraction due to ERM was measured by using image-analysis severity of retinal contraction and amount of change in meta- software developed by the authors to calculate horizontal and morphopsia in patients with ERM who were observed over the vertical components of changes in the locations of retinal long-term (at least 3 years) after diagnosis of ERM. -

Bullous Central Serous Chorioretinopathy: a Rare and Atypical Form of Central Serous Chorioretinopathy
pharmaceuticals Review Bullous Central Serous Chorioretinopathy: A Rare and Atypical Form of Central Serous Chorioretinopathy. A Systematic Review Francesco Sartini * , Martina Menchini, Chiara Posarelli , Giamberto Casini and Michele Figus Ophthalmology, Department of Surgical, Medical, Molecular Pathology and of the Critical Area, University of Pisa, 56126 Pisa, Italy; [email protected] (M.M.); [email protected] (C.P.); [email protected] (G.C.); fi[email protected] (M.F.) * Correspondence: [email protected]; Tel.: +39-050-997675 Received: 26 July 2020; Accepted: 28 August 2020; Published: 28 August 2020 Abstract: Bullous central serous chorioretinopathy (bCSCR) is a rare variant of the central serous chorioretinopathy, complicated by an exudative retinal detachment with shifting fluid. This systematic review aims to present the epidemiology, the pathogenesis, the clinical presentation, the imaging, the differential diagnosis, and the latest treatments of this disease. A total of 60 studies were identified following a literature search adhering to PRISMA guidelines. After full-text evaluation, 34 studies about bCSCR were included. bCSCR usually affects middle-aged men, and the principal risk factor is corticosteroid medications. Pathogenesis is related to an increased choroidal vessel and choriocapillaris permeability, with subsequent subretinal fluid accumulation, rich in fibrin, which may provoke the exudative retinal detachment. Clinical presentation and imaging are fundamental to distinguish bCSCR from other pathologies, avoiding unappropriated treatment. Corticosteroid withdraws (if assumed) and laser photocoagulation of leakage sites seen at angiography may speed up retinal reattachment. Verteporfinphotodynamic therapy,transpupillary thermal therapy, oral eplerenone and scleral thinning surgery are other therapeutic options. An early diagnosis might prevent disease progression due to harmful medications as well as unnecessary surgery. -
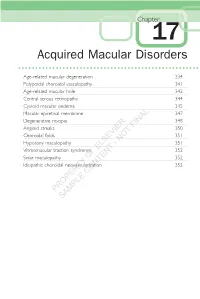
Acquired Macular Disorders
Chapter 17 Acquired Macular Disorders Age-related macular degeneration 334 Polypoidal choroidal vasculopathy 341 Age-related macular hole 342 Central serous retinopathy 344 Cystoid macular oedema 345 Macular epiretinal membrane 347 Degenerative myopia 348 Angioid streaks FINAL 350 Choroidal folds 351 NOT Hypotony maculopathy - 351 Vitreomacular traction syndrome ELSEVIER 352 Solar maculopathy OF 352 Idiopathic choroidal neovascularization 352 CONTENT PROPERTY SAMPLE 334 Acquired Macular Disorders Age-related macular degeneration Drusen 1. Histopathology (Fig. 17.1) • Discrete deposits of the abnormal material located between the basal lamina of the RPE and the inner collagenous layer of Bruch membrane. • Thickening of Bruch membrane Fig. 17.2 Hard drusen compounded by excessive production of basement mem- brane deposit by the RPE. a FINAL Atrophy and depigmentation NOT - RPE ELSEVIER OF Bruch membrane Drusen Thickening CONTENTb Fig. 17.1 Histopathology of drusen 2. Signs – yellow sub-RPEPROPERTY excrescences distributed symmetricallySAMPLE at both posterior poles. a. Small hard drusen – less than half a vein width in diameter with discrete margins (Fig. 17.2). b. Large soft drusen – vein width or more in diameter with indistinct margins (Fig. 17.3a). Fig. 17.3 (a) Soft drusen; (b) FA c. Calcifi ed drusen – may be hard or soft (Fig. 17.4). Age-related macular degeneration 335 a Fig. 17.4 Calcifi ed drusen b 3. FA a. Hyperfl uorescence – window defect due to atrophy of the overlying RPE and late staining (see FINAL Fig. 17.3b). b. Hypofl uorescence – of hydrophobic NOT (high lipid content) drusen. - 4. Drusen and AMD – features ELSEVIER associated with an increased risk of subsequent visual loss include largeOF soft and/or confl uent drusen, and Fig. -

Recent Advances of Computerized Graphical Methods for the Detection and Progress Assessment of Visual Distortion Caused by Macular Disorders
Review Recent Advances of Computerized Graphical Methods for the Detection and Progress Assessment of Visual Distortion Caused by Macular Disorders Navid Mohaghegh, Ebrahim Ghafar-Zadeh * and Sebastian Magierowski Department of Electrical Engineering and Computer Science (EECS), Lassonde School of Engineering, York University, Toronto, ON M3J 1P3, Canada; [email protected] (N.M); [email protected] (S.M.) * Correspondence: [email protected]; Tel.: +1-416-736-2100 Received: 17 April 2019; Accepted: 27 April 2019; Published: 5 June 2019 Abstract: Recent advances of computerized graphical methods have received significant attention for detection and home monitoring of various visual distortions caused by macular disorders such as macular edema, central serous chorioretinopathy, and age-related macular degeneration. After a brief review of macular disorders and their conventional diagnostic methods, this paper reviews such graphical interface methods including computerized Amsler Grid, Preferential Hyperacuity Perimeter, and Three-dimensional Computer-automated Threshold Amsler Grid. Thereafter, the challenges of these computerized methods for accurate and rapid detection of macular disorders are discussed. The early detection and progress assessment of macular disorders can significantly enhance the required clinical procedure for the diagnosis and treatment of macular disorders. Keywords: macular disorders; central serous retinopathy (CSR); graphical macular interface system (GMIS); age-related macular degeneration (AMD) I. Introduction Macular disorders such as myopic maculopathy, macular holes, diabetic macular edema, age- related macular degeneration (AMD), and central serous retinopathy (CSR) cause visual distortion (VD) in their early stages [1,2]. In their advanced phases, macular disorders cause central vision loss. Among these retinal conditions, AMD is the leading cause of blindness and will affect the central vision of 196 million people over the age of 65 worldwide by 2020 [3]. -

Retinal Pigment Epithelial Detachment Pigment Epithelial Detachment (PED)
Retinal pigment epithelial detachment Pigment epithelial detachment (PED) DESCRIPTION reveal a deficit: Visual field testing Retinal pigment epithelium (RPE) with an 18Hz flickering stimulus can detachment appears to result from disor- enhance the detection of the visual ders that disrupt the normal junction defect in RPE detachment. Delayed between the basement membrane of the retinal recovery time with the photo- RPE and the inner collagenous Bruch’s stress test may be present. membrane. This disruption may be associated with: Review and advice ● Thickening of Bruch’s membrane, Review and monitoring may be all that with associated increased resistance to is needed for RPE detachment without fluid flow from the retina, causing serous evidence of other retinal or choroidal fluid accumulation under the RPE disease. Review interval is dictated by the ● Choroidal circulation abnormalities level of symptoms and visual compro- leading to accumulation of serous fluid mise. Patients may be advised to conduct from the choriocapillaris in the sub-RPE Large chronic RPE detachment monocular checks (alternate covering of space each eye) and weekly home-monitoring ● Choroidal neovascularisation (CNV) DIFFereNTIal DIAGNOSIS with an Amsler grid. leading to haemorrhagic or fibrovascular Retinal detachment – exudative, Central RPE detachment. serous chorio-retinopathy, Choroidal Laser surgery detachment, Melanoma of the choroid Photodynamic therapy is rarely indicated ASSOCIATED CONDITIONS (malignant melanoma), Choroidal for chronic non-resolving idiopathic The most common condition associated metastasis, Best’s disease RPE detachment, or that associated with RPE detachment is age-related with CNV, with the aim of decreasing macular degeneration. Other possible SEE alSO leakage from the possibly anomalous associated ocular conditions are listed Age-related macular degeneration, underlying choriocapillaris circulation below. -

Epiretinal Membranes
RETINA HEALTH SERIES | Facts from the ASRS The Foundation American Society of Retina Specialists Committed to improving the quality of life of all people with retinal disease. Epiretinal Membranes (ERMs), also commonly SYMPTOMS known as cellophane maculopathy or macular puckers, are avascular (having few or no blood vessels), semi- Most patients with ERMs have translucent, fibrocellular membranes that form on the no symptoms; their ERMs are inner surface of the retina. They most commonly cause found incidentally on dilated retinal exam or on retinal imaging minimal symptoms and can be simply observed, but in such as with ocular coherence some cases they can result in painless loss of vision and tomography (OCT). In such cases, metamorphopsia (visual distortion). Generally, ERMs are patients typically have normal or near-normal vision. However, ERMs most symptomatic when affecting the macula, which is the can slowly progress, leading to central portion of the retina that helps us to distinguish fine a vague visual distortion that can detail used for reading and recognizing faces. be perceived better by closing the non- or less-affected eye. Patients may notice metamorph- The cause of ERMs is due to a Causes: opsia, a symptom that causes visual defect in the surface layer of the retina distortion in which shapes that where a type of cell, called glial cells, are normally straight, like window can migrate through and start to grow blinds or a door frame, looking in a membranous sheet on the retinal “wavy” or “crooked,” especially surface. This membrane can appear when compared to the other like cellophane and over time may eye. -

Focal Congenital Anomalies of the Retinal Pigment Epithelium
Eye (1989) 3,1-18 DOYNE LECTURE Focal Congenital Anomalies of the Retinal Pigment Epithelium J. D. M. GASS Miami, Florida, USA Summary The terms, 'hamartoma', 'choristoma', 'phacoma' (mother-spot), and 'naevus', are used to describe benign developmental tumours or placoid lesions. Stedman's Medical Dictionary defines a hamartoma as: 'A focal malformation that resembles a neoplasm grossly and even microscopically, but results from faulty development in an organ; it is composed of an abnor mal mixture of tissue elements, or an abnormal proportion of a single element, normally pre sent in that site, which develop and grow at virtually the same rate as normal components, and are not likely to result in compression of the adjacent tissue (in contrast to neoplastic tissue).>! A choristoma is defined as 'a mass formed by maldevelopment of tissue of a type not normally found at that site.' Phacoma is defined as, 'a hamartoma found in phacomatosis,' a group of hereditary diseases characterised by hamartomas of multiple tissues. A naevus is a, 'birth mark; a circumscribed malformation of the skin, especially if coloured by hyperpigmentation or increased vascularity; it may be predominantly epidermal, adnexal, melanocytic, vascular, or mesodermal, or a localised overgrowth of melanin-forming cells arising in the skin early in life.' Ophthalmologists have adopted the term to refer to developmental melanocytic lesions of the uveal tract, but heretofore have not used it to describe developmental melanocytic, glial, or vascular lesions of the retina. The purpose of this report is to summarise the author's observations and concepts concern ing focal lesions that probably are developmental tumours and placoid lesions composed of either entirely or in part retinal pigment epithelium (RPE). -

Novel Quantitative Assessment of Metamorphopsia in Maculopathy
Low Vision Novel Quantitative Assessment of Metamorphopsia in Maculopathy Emily Wiecek,1–3 Kameran Lashkari,1,2 Steven C. Dakin,3–5 and Peter Bex1,2,6 1Schepens Eye Research Institute/Mass. Eye and Ear, Boston, Massachusetts, United States 2Harvard Medical School, Department of Ophthalmology, Boston, Massachusetts, United States 3Institute of Ophthalmology, University College London, London, United Kingdom 4National Institute for Health Research (NIHR) Biomedical Research Centre at Moorfields Eye Hospital NHS Foundation Trust, London, United Kingdom 5Department of Optometry & Vision Science, University of Auckland, New Zealand 6Department of Psychology, Northeastern University, Boston, Massachusetts, United States Correspondence: Emily Wiecek, PURPOSE. Patients with macular disease often report experiencing metamorphopsia (visual 105-107 Forsyth Street, Boston, MA distortion). Although typically measured with Amsler charts, more quantitative assessments of 02115, USA; perceived distortion are desirable to effectively monitor the presence, progression, and [email protected]. remediation of visual impairment. Submitted: August 4, 2014 METHODS. Participants with binocular ( 33) and monocular ( 50) maculopathy across Accepted: October 27, 2014 n ¼ n ¼ seven disease groups, and control participants (n ¼ 10) with no identifiable retinal disease Citation: Wiecek E, Lashkari K, Dakin completed a modified Amsler grid assessment (presented on a computer screen with eye SC, Bex P. Novel quantitative assess- tracking to ensure fixation compliance) and two novel assessments to measure metamor- ment of metamorphopsia in maculop- phopsia in the central 58 of visual field. A total of 81% (67/83) of participants completed a athy. Invest Ophthalmol Vis Sci. 2015;56:494–504. DOI:10.1167/ hyperacuity task where they aligned eight dots in the shape of a square, and 64% (32/50) of iovs.14-15394 participants with monocular distortion completed a spatial alignment task using dichoptic stimuli.