Clinical Parameters Related to Metamorphopsia Outcome In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Challenges in Ophthalmic Pathology: the Vitreoretinal Membrane Biopsy
Challenges in PAUL HISCOTT, DAVID WONG, IAN GRIERSON ophthalmic pathology: The vitreoretinal membrane biopsy Abstract detachment.s Sheets or strands crossing the vitreous are sometimes called transvitreous The introduction of vitreoretinal microsurgery membranes. Anteriorly, membranes can arise has produced a new type of biopsy; that of the in, or be continuous with, the vitreous base and vitreoretinal membrane. This review even extend as far as the posterior iris surface or investigates methods by which these scar-like pupil. tissues are handled in the laboratory and Biopsies of pathological tissue are usually explores the implications of the results of such undertaken to establish a diagnosis. evaluations. The study of vitreoretinal Vitreoretinal biopsies also may be for diagnostic membrane biopsies has provided much purposes as, for example, in the case of information concerning the pathobiology of intraocular lymphoma, but such conditions are the various conditions which may give rise to rare and tend not to produce membranes. the tissue as well as insights into how Conversely, in the conditions which do produce membranes themselves develop. Moreover, membranes the diagnosis is seldom in doubt. the application of new laboratory techniques Why, then, attempt laboratory studies of is expected to enhance our understanding of vitreoretinal membranes? Laboratory findings the formation of vitreoretinal membranes, and from the membranes may have a number of lead to further advances in their surgical and uses, for example providing 'feed-back' to the medical management. surgeon concerning surgical dissection planes Key words Age-related macular degeneration, (see below). However, the principal objective of Epiretinal membrane, Proliferative diabetic these investigations is to improve our retinopathy, Proliferative vitreoretinopathy, understanding of the pathogenesis of P Hiscott D. -

SHOULD YOU OPEN a DRY-EYE CLINIC? Experts Help You Weigh the Pros and Cons
RETINAL PHOTOS ON THE GO P. 16 • CHANGES TO MEDICARE ABN FORMS P. 20 ENSURING A HAPPY CATARACT PATIENT P. 22 • MANAGING GLAUCOMA IN KPRO PATIENTS P. 58 THE CURRENT STATE OF VITREORETINAL EDUCATION P. 64 • WILLS EYE RESIDENT CASE REPORT P. 70 September 2020 reviewofophthalmology.com SHOULD YOU OPEN A DRY-EYE CLINIC? Experts help you weigh the pros and cons. P. 28 ALSO INSIDE: • The Latest Treatments for Dry Eye P. 38 • Comprehensive Ophthalmologists and Anti-VEGF Injections P. 48 • How to Manage Ocular Herpes P. 54 SHE MAY NEED MORE THAN ARTIFICIAL TEARS TO DISRUPT INFLAMMATION IN DRY EYE DISEASE1,2 Her eyes deserve a change. Choose twice-daily Xiidra for lasting relief that can start as early as 2 weeks.3*† Not an actual patient. *In some patients with continued daily use. One drop in each eye, twice daily (approximately 12 hours apart).3 †XiidraisanLFA-1antagonistforthetreatmentofdryeyedisease.Pivotaltrialdata:ThesafetyandefficacyofXiidrawereassessedinfour Important Safety Information (cont) 12-week,randomized,multicenter,double-masked,vehicle-controlledstudies(N=2133).Patientsweredosedtwicedaily.Useofartificial • I n clinicaltrials,themostcommonadversereactionsreportedin5-25%ofpatientswereinstillationsite tearswasnotallowedduringthestudies.Thestudyendpointsincludedassessmentofsigns(basedonInferiorfluoresceinCornealStaining irritation,dysgeusiaandreducedvisualacuity.Otheradversereactionsreportedin1%to5%ofthepatients Score [ICSS] on a scale of 0 to 4) and symptoms (based on patient-reported Eye Dryness Score [EDS] on a visual analogue scale of 0 to 100).3 were blurred vision, conjunctival hyperemia, eye irritation, headache, increased lacrimation, eye discharge, A larger reduction in EDS favoring Xiidra was observed in all studies at day 42 and day 84. Xiidra reduced symptoms of eye dryness at eye discomfort, eye pruritus and sinusitis. 2 weeks (based on EDS) compared to vehicle in 2 out of 4 clinical trials. -

Exploring Topical Anti-Glaucoma Medication Effects on the Ocular Surface in the Context of the Current Understanding of Dry Eye
The Ocular Surface 16 (2018) 289e293 Contents lists available at ScienceDirect The Ocular Surface journal homepage: www.theocularsurface.com Original Research Exploring topical anti-glaucoma medication effects on the ocular surface in the context of the current understanding of dry eye Aaron B.C. Wong, Michael T.M. Wang, Kevin Liu, Zak J. Prime, Helen V. Danesh-Meyer, * Jennifer P. Craig Department of Ophthalmology, New Zealand National Eye Centre, The University of Auckland, New Zealand article info abstract Article history: Purpose: To assess tear film parameters, ocular surface characteristics, and dry eye symptomology in Received 11 November 2017 patients receiving topical anti-glaucoma medications. Received in revised form Methods: Thirty-three patients with a diagnosis of open angle glaucoma or ocular hypertension, 26 February 2018 receiving unilateral topical anti-glaucoma medication for at least 6 months, were recruited in a cross- Accepted 2 March 2018 sectional, investigator-masked, paired-eye comparison study. Tear film parameters, ocular surface characteristics, and dry eye symptomology of treated and fellow eyes were evaluated and compared. Keywords: Results: The mean ± SD age of the participants was 67 ± 12 years, and the mean ± SD treatment duration Glaucoma ± fi ¼ fi Prostaglandin analogue was 5.3 4.4 years. Treated eyes had poorer non-invasive tear lm breakup time (p 0.03), tear lm ¼ ¼ Tear film osmolarity (p 0.04), bulbar conjunctival hyperaemia (p 0.04), eyelid margin abnormality grade Ocular surface (p ¼ 0.01), tear meniscus height (p ¼ 0.03), and anaesthetised Schirmer value (p ¼ 0.04) than fellow eyes. Dry eye There were no significant differences in dry eye symptomology, meibomian gland assessments, and Meibomian gland ocular surface staining between treated and fellow eyes (all p > 0.05). -

The Visual Performance and Metamorphopsia of Patients with Macular Holes
CLINICAL SCIENCES The Visual Performance and Metamorphopsia of Patients With Macular Holes Yoshihiro Saito, MD; Yoshiko Hirata, MD; Atsushi Hayashi, MD; Takashi Fujikado, MD; Masahito Ohji, MD; Yasuo Tano, MD Background: Most patients attain better visual acuity divided the subjective changes into 2 types of metamor- with the elimination of metamorphopsia after success- phopsia; of the 54 eyes, pincushion distortion (bowed ful closure of a macular hole (MH) by vitrectomy. toward the center) was found in 33 (61%), and unpat- terned distortion (no specific pattern) was found in 21 Objective: To determine the presurgical visual func- (39%). Pincushion distortion was significantly associ- tion of eyes with an MH. ated with an MH of shorter duration (#6 months) (P = .03) and an early stage (stage 2) of MH formation Methods: We examined 54 eyes of 51 patients with an (P = .02). A scotoma was hard to detect, and patients had idiopathic MH using the Amsler chart. We evaluated difficulty describing their scotomata and distortions. In the types of subjective metamorphopsia and compared the montage test, patients with early MHs chose por- them with the clinical factors associated with MHs. In a traits modified with a pincushion type of distortion. prospective study, we performed a montage test on a separate group of 16 patients with unilateral idiopathic Conclusions: We found concentric pincushion meta- MHs. The patients were asked to choose, while viewing morphopsia without subjective scotomata, which we sug- with their better eye, the computer-modified picture gest arises from an eccentric displacement of the photo- that best matched the unmodified image seen by the eye receptors. -

Macular Hole Formation Following Choroidal Neovascularization
Yoshida et al., Int J Ophthalmol Clin Res 2015, 2:1 International Journal of ISSN: 2378-346X Ophthalmology and Clinical Research Case Report: Open Access Macular Hole Formation Following Choroidal Neovascularization Treatment in A High Myopic Eye with Epiretinal Membrane Yusaku Yoshida*, Manabu Yamamoto, Takeya Kohno and Kunihiko Shiraki Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, Japan *Corresponding author: Yusaku Yoshida, MD, Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka 545-8585, Japan, Fax:+81-666-343- 873, E-mail: [email protected] macular hole development where post-treatment regression of CNV Abstract seemed to have played a major role in a high myopic eye with ERM. Purpose: To report on the development of macular hole after treatment of choroidal neovascularization (CNV) in a patient with Case high myopia and epiretinal membrane (ERM). A 60-year-old man was examined in the Department of Methods: Retrospective single case report. Ophthalmology of Osaka City University Hospital for reduced vision Patients: A 60-year-old man presented with reduced vision in his in his right eye in January 2009. On initial examination, decimal best- right eye. On the initial examination, the right eye was high myopic corrected visual acuity (BCVA) was 0.3 in the right eye and 1.5 in with decimal best-corrected visual acuity (BCVA) of 0.3. the left eye, while intraocular pressures were 13 and 14 mmHg in the right and left eye, respectively. His previous medical and family Results: A subretinal grayish-white lesion was seen at the macula with hemorrhage, and optical coherence tomography showed a histories included nothing of note. -
Epiretinal Membrane
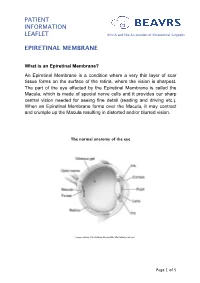
PATIENT INFORMATION LEAFLET British and Eire Association of Vitreoretinal Surgeons EPIRETINAL MEMBRANE What is an Epiretinal Membrane? An Epiretinal Membrane is a condition where a very thin layer of scar tissue forms on the surface of the retina, where the vision is sharpest. The part of the eye affected by the Epiretinal Membrane is called the Macula, which is made of special nerve cells and it provides our sharp central vision needed for seeing fine detail (reading and driving etc.). When an Epiretinal Membrane forms over the Macula, it may contract and crumple up the Macula resulting in distorted and/or blurred vision. The normal anatomy of the eye *Image courtesy of the National Eye Institute http://www.nei.nih.gov Page 1 of 5 PATIENT INFORMATION British and Eire Association of Vitreoretinal Surgeons LEAFLET EPIRETINAL MEMBRANE Why do I have an Epiretinal Membrane? In most cases the development of an Epiretinal Membrane appears to be related to normal aging changes inside the eye. In some cases it can be related to other conditions such as diabetes, blockage of blood vessel, inflammation or following retinal surgery. Epiretinal membranes are not related to Macular Degeneration. Epiretinal Membranes do not usually affect the other eye. They are quite common and affect up to 8% of people in later years. Cross-section of a healthy macula Cross-section of a macula with an epiretinal membrane Assessment for Epiretinal Membrane Your eye doctor is able to detect an Epiretinal Membrane during an eye examination following the use of eye drops that temporarily make your pupils large. -

Vitreomacular Traction Syndrome
RETINA HEALTH SERIES | Facts from the ASRS The Foundation American Society of Retina Specialists Committed to improving the quality of life of all people with retinal disease. Vitreomacular Traction Syndrome SYMPTOMS IN DETAIL The vitreous humor is a transparent, gel-like material that fills the space within the eye between the lens and The most common symptoms the retina. The vitreous is encapsulated in a thin shell experienced by patients with VMT syndrome are: called the vitreous cortex, and the cortex in young, healthy • Decreased sharpness of vision eyes is usually sealed to the retina. • Photopsia, when a person sees flashes of light in the eye As the eye ages, or in certain pathologic conditions, the vitreous cortex can • Micropsia, when objects appear pull away from the retina, leading to a condition known as posterior vitreous smaller than their actual size detachment (PVD). This detachment usually occurs as part of the normal • Metamorphopsia, when vision aging process. is distorted to make a grid of There are instances where a PVD is incomplete, leaving the vitreous straight lines appear wavy partially attached to the retina, and causing tractional (pulling) forces that or blank can cause anatomical damage. The resulting condition is called vitreomacular Some of these symptoms can be traction (VMT) syndrome. mild and develop slowly; however, VMT syndrome can lead to different maculopathies or disorders in the chronic tractional effects can macular area (at the center of the retina), such as full- or partial-thickness lead to continued visual loss macular holes, epiretinal membranes, and cystoid macular edema. These if left untreated. -

Myopic Choroidal Neovascularisation: Current Concepts and Update On
BJO Online First, published on July 1, 2014 as 10.1136/bjophthalmol-2014-305131 Review Br J Ophthalmol: first published as 10.1136/bjophthalmol-2014-305131 on 1 July 2014. Downloaded from Myopic choroidal neovascularisation: current concepts and update on clinical management Tien Y Wong,1 Kyoko Ohno-Matsui,2 Nicolas Leveziel,3 Frank G Holz,4 Timothy Y Lai,5 Hyeong Gon Yu,6 Paolo Lanzetta,7 Youxin Chen,8 Adnan Tufail9 For numbered affiliations see ABSTRACT PATHOGENESIS OF MYOPIC CNV end of article. Choroidal neovascularisation (CNV) is a common vision- Several theories have been proposed to explain the threatening complication of myopia and pathological development of myopic CNV, reviewed in detail Correspondence to 4 Dr Tien Y Wong, Singapore Eye myopia. Despite significant advances in understanding elsewhere. The mechanical theory is based on the Research Institute, Singapore the epidemiology, pathogenesis and natural history of assumption that the progressive and excessive National Eye Centre, National myopic CNV, there is no standard definition of myopic elongation of the anteroposterior axis causes a University of Singapore, 11 CNV and its relationship to axial length and other mechanical stress on the retina, leading to an imbal- Third Hospital Avenue, Singapore 168751, Singapore; myopic degenerative changes. Several treatments are ance between pro-angiogenic and anti-angiogenic 7 [email protected] available to ophthalmologists, but with the advent of factors, resulting in myopic CNV. In support, the new therapies there is a need for further consensus and presence of lacquer cracks has been shown to be a Received 7 March 2014 clinical management recommendations. -

Cholesterol Dyshomeostasis and Age Related Macular Degeneration Bhanu Chandar Dasari
University of North Dakota UND Scholarly Commons Theses and Dissertations Theses, Dissertations, and Senior Projects 1-1-2012 Cholesterol Dyshomeostasis And Age Related Macular Degeneration Bhanu Chandar Dasari Follow this and additional works at: https://commons.und.edu/theses Recommended Citation Dasari, Bhanu Chandar, "Cholesterol Dyshomeostasis And Age Related Macular Degeneration" (2012). Theses and Dissertations. 1235. https://commons.und.edu/theses/1235 This Thesis is brought to you for free and open access by the Theses, Dissertations, and Senior Projects at UND Scholarly Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. CHOLESTEROL DYSHOMEOSTASIS AND AGE RELATED MACULAR DEGENERATION by Bhanu Chandar Dasari Bachelor of Science, Kakatiya University, 1999 Master of Science, University of Pune, 2001 A Dissertation Submitted to the Graduate Faculty of the University of North Dakota in partial fulfillment of the requirements for the degree of Doctor of Philosophy Grand Forks, North Dakota May 2012 This dissertation, submitted by Bhanu Chandar Dasari in partial fulfillment of the requirements for the Degree of Doctor of Philosophy from the University of North Dakota, has been read by the Faculty Advisory Committee under whom the work has been done and is hereby approved. __________________________________ Othman Ghribi, Ph.D. __________________________________ Brij B. Singh, Ph.D. __________________________________ Colin K. Combs, Ph.D. __________________________________ James E. Porter, Ph.D. __________________________________ Saobo Lei, Ph.D. This dissertation is being submitted by the appointed advisory committee as having met all of the requirements of the Graduate School at the University of North Dakota and is hereby approved. -

Retinal Contraction and Metamorphopsia Scores in Eyes with Idiopathic Epiretinal Membrane
Retinal Contraction and Metamorphopsia Scores in Eyes with Idiopathic Epiretinal Membrane Eiko Arimura, Chota Matsumoto, Sachiko Okuyama, Sonoko Takada, Shigeki Hashimoto, and Yoshikazu Shimomura PURPOSE. Using M-CHARTS (Inami Co., Tokyo, Japan), which assessment charts, M-CHARTS (Inami Co., Tokyo, Japan), with were developed by the authors to measure metamorphopsia, which it is possible to quantify the degree of metamorphopsia and image-analysis software, which was developed to quantify in patients with disease involving the macula.2,3 It is known retinal contraction, the authors investigated the relationship that one of the main causes of metamorphopsia in individuals between the degree of retinal contraction and the degree of with macula diseases is disarray of the photoreceptors in the metamorphopsia in eyes with idiopathic epiretinal membrane sensory retina. Especially in cases of ERM, the photoreceptors (ERM). and/or the outer segments are dislocated due to the contrac- METHODS. This study was conducted in 29 eyes with ERM (29 tion of the proliferating membranes. However, to date there patients, 20 women; mean age, 62.1 Ϯ 8.6 years) observed for have been no detailed long-term follow-up studies to evaluate at least 3 years (mean, 3.55 Ϯ 0.6 years) after diagnosis. Hori- the relationship between the progression of retinal contraction zontal (MH) and vertical (MV) metamorphopsia scores were and change in metamorphopsia. We therefore decided to con- obtained with the M-CHARTS. Horizontal and vertical retinal duct this study to investigate the relationship between the contraction due to ERM was measured by using image-analysis severity of retinal contraction and amount of change in meta- software developed by the authors to calculate horizontal and morphopsia in patients with ERM who were observed over the vertical components of changes in the locations of retinal long-term (at least 3 years) after diagnosis of ERM. -

Home>>Common Retinal & Ophthalmic Disorders
Common Retinal & Ophthalmic Disorders Cataract Central Serous Retinopathy Cystoid Macular Edema (Retinal Swelling) Diabetic Retinopathy Floaters Glaucoma Macular degeneration Macular Hole Macular Pucker - Epiretinal Membrane Neovascular Glaucoma Nevi and Pigmented Lesions of the Choroid Posterior Vitreous Detachment Proliferative Vitreoretinopathy (PVR) Retinal Tear and Detachment Retinal Artery and Vein Occlusion Retinitis Uveitis (Ocular Inflammation) White Dot Syndromes Anatomy and Function of the Eye (Short course in physiology of vision) Cataract Overview Any lack of clarity in the natural lens of the eye is called a cataract. In time, all of us develop cataracts. One experiences blurred vision in one or both eyes – and this cloudiness cannot be corrected with glasses or contact lens. Cataracts are frequent in seniors and can variably disturb reading and driving. Figure 1: Mature cataract: complete opacification of the lens. Cause Most cataracts are age-related. Diabetes is the most common predisposing condition. Excessive sun exposure also contributes to lens opacity. Less frequent causes include trauma, drugs (eg, systemic steroids), birth defects, neonatal infection and genetic/metabolic abnormalities. Natural History Age-related cataracts generally progress slowly. There is no known eye-drop, vitamin or drug to retard or reverse the condition. Treatment Surgery is the only option. Eye surgeons will perform cataract extraction when there is a functional deficit – some impairment of lifestyle of concern to the patient. Central Serous Retinopathy (CSR) Overview Central serous retinopathy is a condition in which a blister of clear fluid collects beneath the macula to cause acute visual blurring and distortion (Figure 2). Central serous retinochoroidopathy Left: Accumulation of clear fluid beneath the retina. -

Bullous Central Serous Chorioretinopathy: a Rare and Atypical Form of Central Serous Chorioretinopathy
pharmaceuticals Review Bullous Central Serous Chorioretinopathy: A Rare and Atypical Form of Central Serous Chorioretinopathy. A Systematic Review Francesco Sartini * , Martina Menchini, Chiara Posarelli , Giamberto Casini and Michele Figus Ophthalmology, Department of Surgical, Medical, Molecular Pathology and of the Critical Area, University of Pisa, 56126 Pisa, Italy; [email protected] (M.M.); [email protected] (C.P.); [email protected] (G.C.); fi[email protected] (M.F.) * Correspondence: [email protected]; Tel.: +39-050-997675 Received: 26 July 2020; Accepted: 28 August 2020; Published: 28 August 2020 Abstract: Bullous central serous chorioretinopathy (bCSCR) is a rare variant of the central serous chorioretinopathy, complicated by an exudative retinal detachment with shifting fluid. This systematic review aims to present the epidemiology, the pathogenesis, the clinical presentation, the imaging, the differential diagnosis, and the latest treatments of this disease. A total of 60 studies were identified following a literature search adhering to PRISMA guidelines. After full-text evaluation, 34 studies about bCSCR were included. bCSCR usually affects middle-aged men, and the principal risk factor is corticosteroid medications. Pathogenesis is related to an increased choroidal vessel and choriocapillaris permeability, with subsequent subretinal fluid accumulation, rich in fibrin, which may provoke the exudative retinal detachment. Clinical presentation and imaging are fundamental to distinguish bCSCR from other pathologies, avoiding unappropriated treatment. Corticosteroid withdraws (if assumed) and laser photocoagulation of leakage sites seen at angiography may speed up retinal reattachment. Verteporfinphotodynamic therapy,transpupillary thermal therapy, oral eplerenone and scleral thinning surgery are other therapeutic options. An early diagnosis might prevent disease progression due to harmful medications as well as unnecessary surgery.