Spring 2002 Silver Lining CDH Newsletter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

New Books List October-December 2011
New Books List October-December 2011 This catalogue of the Shakespeare First Folio (1623) is the result of two decades of research during which 232 surviving copies of this immeasurably important book were located – a remarkable 72 more than were recorded in the previous census over a century ago – and examined in situ, creating an essential reference work. ෮ Internationally renowned authors Eric Rasmussen, co-editor of the RSC Shakespeare series and Professor of English at the University of Nevada, Reno, USA; Anthony James West, Shakespeare scholar, focused on the history of the First Folio since it left the press. ෮ Full bibliographic descriptions of each extant copy, including detailed accounts of press variants, watermarks, damage or repair and provenance ෮ Fascinating stories about previous owners and incidents ෮ Striking Illustrations in a colour plate section ෮ User’s Guide and Indices for easy cross referencing ෮ Hugely significant resource for researchers into the history of the book, as well as auction houses, book collectors, curators and specialist book dealers November 2011 | Hardback | 978-0-230-51765-3 | £225.00 For more information, please visit: www.palgrave.com/reference Order securely online at www.palgrave.com or telephone +44 (0)1256 302866 fax + 44(0)1256 330688 email [email protected] Jellybeans © Andrew Johnson/istock.com New Books List October-December 2011 KEY TO SYMBOLS Title is, or New Title available Web resource as an ebook Textbook comes with, a available CD-ROM/DVD Contents Language and Linguistics 68 Anthropology -
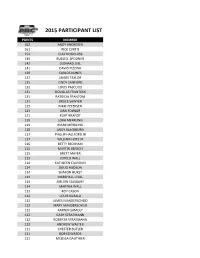
2015 Abcs Membersht.Csv
2015 PARTICIPANT LIST POINTS MEMBER 162 ANDY ANDRESEN 161 RICK CURTIS 152 CLAY DOUGLASS 145 RUSSELL SPOONER 142 LEONARD DILL 141 DAVID PIZZINO 139 CARLOS NUNES 137 JAMESTAYLOR 135 CINDY SANFORD 132 LOUIS PASCUCCI 131 DOUGLAS FRANTOM 131 PATRICIA FRANTOM 131 BRUCE SAWYER 125 NIKKI PETERSEN 123 DANFOWLER 121 KURT BRANDT 119 LORA MERKLING 119 MARK MERKLING 118 ANDY BLACKBURN 117 PHILLIP HALLFORD JR 117 WILLIAM HOTZ JR 116 BETTY BECKHAM 115 MARTIN BENSCH 115 BRETT MAYER 115 JEROLD WALL 114 KATHLEEN CALHOUN 114 DOUG HUDSON 114 SHARON HURST 114 MARSHALL LYALL 114 MELVIN SALSBURY 114 MARTHA WALL 113 ROY CASON 112 LOUIS KUBALA 112 JAMES MANDERSCHEID 112 MARY MANDERSCHEID 112 KAYREN SAMOLY 112 GARY STRATMANN 112 ROBERTA STRATMANN 112 ANDREW WALTER 111 CHESTER BUTLER 111 BOB EDWARDS 111 MELISSA GAUTHIER 111 LARRY LANGLINAIS 111 FREDERICK MCKAY 111 JAMES PIRTLE 111 THELMA PIRTLE 110 JOHN BRATSCHUN 110 NORMA EDWARDS 110 JEFF MCCLAIN 110 SANDRA MCCLAIN 110 MICHAEL PRITCHETT 110 CAROL TIMMONS 110 ROBERT TIMMONS 109 ERNEST STAPLES SR 108 BYRON CONSTANCE 108 ALFRED RATHBUN 107 WILLIAM BUSHALL JR 107 A CALVERT 107 JOHNKIME 107 KELLIE SALSBURY 106 MICHAEL ISEMAN 106 MONAOLSEN 106 THOMASOLSEN 106 SAMUEL STONE 106 JOHNTOOLE 105 VICTOR PONTE 104 PAUL CIPAR 104 DAVID THOMPSON 103 JOHN MCFADDEN 103 BENJAMIN PHILHOWER 103 SHERI PHILHOWER 103 BILL STOCK JR 103 MARTHA STOCK 102 GARY DYER 101 EDWARD GARBIN 101 TEDLAWSON 101 ROY STEPHENS JR 101 CLINT STOTT 100 JACK HARTLEY 100 PETER HULL 100 AARON KONECKY 100 DONNA LANDERS 100 GLEN LANDERS 100 DONSEPANSKI 99 CATHEY -

Embracing Entrepreneurship
Southern Methodist University SMU Scholar Doctor of Ministry Projects and Theses Perkins Thesis and Dissertations Spring 5-15-2021 Embracing Entrepreneurship Naomy Sengebwila [email protected] Naomy Nyendwa Sengebwila Southern Methodist University, [email protected] Follow this and additional works at: https://scholar.smu.edu/theology_ministry_etds Part of the Biological and Physical Anthropology Commons, Folklore Commons, Food Security Commons, Food Studies Commons, Labor Economics Commons, Macroeconomics Commons, Other Social and Behavioral Sciences Commons, Public Affairs, Public Policy and Public Administration Commons, Regional Economics Commons, Social and Cultural Anthropology Commons, Social Justice Commons, Social Work Commons, and the Urban Studies and Planning Commons Recommended Citation Sengebwila, Naomy and Sengebwila, Naomy Nyendwa, "Embracing Entrepreneurship" (2021). Doctor of Ministry Projects and Theses. 9. https://scholar.smu.edu/theology_ministry_etds/9 This Thesis is brought to you for free and open access by the Perkins Thesis and Dissertations at SMU Scholar. It has been accepted for inclusion in Doctor of Ministry Projects and Theses by an authorized administrator of SMU Scholar. For more information, please visit http://digitalrepository.smu.edu. Embracing Entrepreneurship How Christian Social Innovation and Entrepreneurship can Lead to Sustainable Communities in Zambia and Globally Approved by: Dr. Hal Recinos/Dr. Robert Hunt ___________________________________ Advisors Dr. Hugo Magallanes ___________________________________ -

A Vision for a Diocesan Family of Schools
A DIOCESAN FAMILY OF SCHOOLS A Vision for Catholic Schools in the Diocese of Leeds 1. Introduction 1.2 From the time of the restoration of the Catholic Hierarchy in 1850, the provision of, and support for, Catholic schools has been central to the life and mission of the Church in England and Wales. Ever since then, we have been required to work together as a Catholic community to rise to the political, economic and social challenges and opportunities which the Church’s mission in education has had to face. This mission has always taken place in a testing and changing context and our contemporary situation is no exception. 1.3 In the course of my visits to parishes over the past three years, I have met with the Chairs of Governors and Headteachers of the primary schools and academies located within those parishes to listen to their hopes and concerns. It has been a great encouragement to me to learn of the wonderful commitment and energy that exists in our diocesan schools. What has also emerged is a desire for greater clarity about the expectations on primary and secondary schools in relation to the development of the five multi-academy trusts within the diocese. 1.4 It is now just over six years since the Diocese of Leeds published its guidance for governors in October 2011, ‘Building the Future: Considering Multi-Academy Trusts’. This document presented a very clear description of ‘how’ schools could convert to academy status and proposed a framework of how five multi- academy trusts could be structured to offer parents a provision of Catholic education for 3-19 years. -
Fall 2017 Commencement Program
TE TA UN S E ST TH AT I F E V A O O E L F A DITAT DEUS N A E R R S I O Z T S O A N Z E I A R I T G R Y A 1912 1885 ARIZONA STATE UNIVERSITY COMMENCEMENT AND CONVOCATION PROGRAM Fall 2017 December 11-13, 2017 THE NATIONAL ANTHEM THE STAR-SPANGLED BANNER O say can you see, by the dawn’s early light, What so proudly we hailed at the twilight’s last gleaming? Whose broad stripes and bright stars through the perilous fight O’er the ramparts we watched, were so gallantly streaming? And the rockets’ red glare, the bombs bursting in air Gave proof through the night that our flag was still there. O say does that Star-Spangled Banner yet wave O’er the land of the free and the home of the brave? ALMA MATER ARIZONA STATE UNIVERSITY Where the bold saguaros Raise their arms on high, Praying strength for brave tomorrows From the western sky; Where eternal mountains Kneel at sunset’s gate, Here we hail thee, Alma Mater, Arizona State. —Hopkins-Dresskell MAROON AND GOLD Fight, Devils down the field Fight with your might and don’t ever yield Long may our colors outshine all others Echo from the buttes, Give em’ hell Devils! Cheer, cheer for A-S-U! Fight for the old Maroon For it’s Hail! Hail! The gang’s all here And it’s onward to victory! Students whose names appear in this program have completed degree requirements. -

Spring 1998 Course Guide TABLE of CONTENTS
WOMEN, GENDER, SEXUALITY STUDIES PROGRAM UNIVERSITY OF MASSACHUSETTS AMHERST Spring 1998 Course Guide TABLE OF CONTENTS This catalog contains descriptions of all Women’s Studies courses for which information was available in our office by the publication deadline for pre-registration. Please note that some changes may have been made in time, and/or syllabus since our print deadline. Exact information on all courses may be obtained by calling the appropriate department or college. Please contact the Five-College Exchange Office (545-5352) for registration for the other schools listed. Listings are arranged in the following order: Women, Gender, Sexuality Studies Core Courses Courses offered through the Women, Gender, Sexuality Studies program Women of Color Courses Courses that count towards the Woman of Color requirement for UMass Amherst Women, Gender, Sexuality Studies undergraduate majors and minors. Departmental Courses Courses offered in other UMass departments and programs. All courses listed except 100-level automatically count towards the the major. Component Courses Courses offered in other University Departments and Programs. In order to have these courses count towards the major or minor students must focus their paper(s) or project(s) on gender. Graduate Level Five-College Options: Amherst College Hampshire College Mount Holyoke College Smith College Please note that updates to this guide are available on the website. www.umass.edu/wost/courseinfo.htm WOMEN’S STUDIES COURSE DESCRIPTION GUIDE ADDENDA 1/22/98 Cancellation: WOST 492H/682H - Political Ecology of Women’s Health Janice Raymond New departmental course listings: WOST 394E Comparative Approaches to Women and Health: Historical and Activist Case Studies Elise Young Schedule #274419 -- Wednesday 2:30-5:00 The goal of this course is to study the international context of women and health, drawing on case studies. -

Care and Share Food Bank for Southern Colorado 2012-13 Financial Supporters
Care and Share Food Bank for Southern Colorado 2012-13 Financial Supporters 12 Volt Tavern Ms. Sandra Achord Mr. and Mrs. D. V. Addington 1st Bank Mr. and Mrs. Edward Achtenberg Ms. Linda Addington 1st Place for Memories Ms. Cheryl Ackerman Adesa Colorado Springs 2013 Winter in Widefield Ice Bowl Ackley’s Rocks Adesa Great Lakes 4 Bits 4 H Club Ms. Wanda Ackor Adesa Minneapolis 4 MRS Booster Club Mr. Ivan Acosta Ms. Beth Adeson 56 Spirit Committee Mr. and Mrs. George Acree Ms. Janet Adessa A Brit and 3 Yanks Mr. and Mrs. Terry Acree Mr. Tony Adkison A Plus Properties Rosie Adair and Alfred Coxe Ms. Carol Adkisson A to Z Realty Ms. Sally Adame Mr. Douglas Adler A. Bookkeeping and Consulting Service Mr. and Mrs. Bernard Adams Ms. Louise Adler AA “Accurate and Affordable” Striping, Inc Mr. Dale Adams Ms. Margaret Adler AAHS Cheerleaders Mr. and Mrs. David Adams Ms. Kristie Adler Hawkins Ms. Renee Abbe Mr. and Mrs. Ernest Adams Mr. and Mrs. James Adley Mr. and Mrs. James Abbott Mr. and Mrs. Gary Adams Ms. Ann Adnet Ms. Janet Abbott Mr. John Adams II Mr. and Mrs. Dana Adoretti Ms. Marjory Abbott Mr. and Mrs. John Adams Adrian Leroy Hall Trust Mr. and Mrs. Donald Abdallah Mr. and Mrs. John Adams Advanced Auto Detail, LLC Mr. and Mrs. William Abel Maj Kenneth Adams Advisers Investment Management, Inc. Mr. and Mrs. Scott Abell Mr. and Mrs. Laurence Adams Jr. Aerospace Sams Ms. Jennifer Abernathey Mr. and Mrs. Leo Adams Affiliated Business Consultants, Inc. Ms. Mary Lou Abernathy Mr. -

INDIVIDUAL DONORS Mr
Car e and INDIVIDUAL DONORS Mr. and Mrs. Lonnie Adams Ms. Mary Adams Ms. Mary Anne Abbate Mr. and Mrs. Samuel Adams Ms. Renee Abbe Mr. Steve Adams Ms. Marjory Abbott Mr. Tilmon Adams Mr. and Mrs. Steven Abbott Ms. Kimberly Adams-Johnson Mr. and Mrs. Donald Abdallah Mrs. Alda Adcox Mr. and Mrs. Scott Abell Ms. Constance Addington Ms. Mary Lou Abernathy Mr. and Mrs. D. V. Addington Mr. David Abeyta Ms. Linda Addington Mr. Floyd Abeyta Ms. Vicky Addison Mr. and Mrs. Mel Abeyta Ms. Deirdre Aden-Smith Mrs. Dorothy Abrue Ms. Carol Adkisson Ms. Katrina Achivida Ms. Louise Adler Mr. and Mrs. Edward Achtenberg Ms. Kristie Adler Hawkins Ms. Clara Ackerman Mr. and Mrs. James Adley Mr. Mitchell Ackerman Mr. and Mrs. Dana Adoretti Ms. Wanda Ackor Ms. Wendy Adrian Mr. Ivan Acosta Mr. and Mrs. Glen Agajanian Mr. and Mrs. George Acree Mrs. Joan Agee Rosie Adair and Alfred Coxe Erika and Kiyoshi Agena Mr. Paul Adam Mr. and Mrs. Billy Ager Ms. Sally Adame Mr. and Mrs. Gerald Ager Jr. Mr. and Mrs. Bernard Adams Ms. Marilyn Ager Mr. and Mrs. Charles Adams Mr. and Mrs. Mark Aggers Mr. Dale Adams Mr. and Mrs. Gary Agnes Deborah Adams and Charles Campbell Mr. Todd Agthe LTC and Mrs. Donald Adams (Ret) Mr. and Mrs. Albert Aguilar Mr. and Mrs. Ernest Adams Mr. and Mrs. Charles Aguilar Frances and Linda Adams Mr. and Mrs. Erwin Aguilar Mr. and Mrs. Garth Adams Mr. Robert Aguilar Mr. and Mrs. Gary Adams Mr. and Mrs. Theodore Aguilar Ms. Karen Adams Ms. -

Faculty Scholarship May 2015-May 2016
FACULTY SCHOLARSHIP MAY 2015-MAY 2016 Faculty Scholarship at Whitworth in the 21st century, and explore the work of WHO WE ARE Teresa of Avila. Social scientists compare The Whitworth faculty comprises 154 Christian religious and secular HIV-prevention NGOs in teacher-scholars who engage in research, Kenya and present on hope in a consumerist writing, and creative performance to advance culture. Faculty in the arts perform, contribute their understanding of the world, to enrich to exhibits, write about microcontrollers and their teaching, to share their discoveries, and music, create arrangements for jazz ensembles, to bring new information and insights into and compose hymns. Economists write about their classrooms. Organizations beyond our household economics, and educators present campus recognize the high quality of our faculty their research on programs for high-ability scholarship; many support Whitworth research learners. programs. Whitworth faculty members have received grants from a broad range of funders WHY WE DO IT including federal grants from the National At Whitworth, teaching and scholarship are Science Foundation, the National Institutes not seen as separate and competing spheres. of Health and the U.S. State Department’s Faculty members model lifelong learning for Fulbright program; state funding from our students while staying immersed in the the Office of the Superintendent of Public joy of discovery and connected to the broader Instruction; support from private regional and conversations of their academic disciplines. national foundations such as the M. J. Murdock Some faculty members conduct research and Charitable Trust and the Lilly Endowment; write monographs with their undergraduate and funding from local corporate foundations students in special research programs that including Spokane Teachers Credit Union and mentor students for graduate study. -
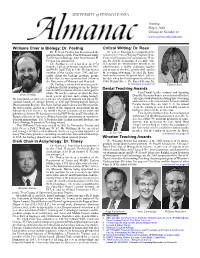
May 6 Issue-Final
UNIVERSITY of PENNSYLVANIA Tuesday, May 6, 2003 Volume 49 Number 32 www.upenn.edu/almanac Williams Chair in Biology: Dr. Poethig Critical Writing: Dr. Ross Dr. R. Scott Poethig has been named the Dr. Valerie Ross has been appointed Di- inaugural holder of the Paul Williams Family rector of the Critical Writing Program in the Term Chair in Biology, SAS Dean Samuel H. Center for Programs in Contemporary Writ- Preston has announced. ing, Dr. Al Filreis announced recently. “She Dr. Poethig received his B.A. in 1974 is a person of extraordinary talents as an from the College of Wooster and his M. Phil. administrator, a highly evaluated teacher and Ph.D. from Yale in 1981. He has been a and mentor to teachers, greatly dedicated to member of the faculty since 1983 and cur- the teaching of writing,” he said. Dr. Ross’ rently chairs the biology graduate group. work as director will begin on July 1, 2003— Before that, he was a postdoctoral fellow at the date when the Center opens its offices at the University of Missouri and Stanford. 3808 Walnut Street. Dr. Ross will join Dr. Dr. Poethig’s research focuses on genetic (continued on page 3) Valerie Ross regulation of plant morphogenesis, the forma- tion and differentiation of tissues and organs in Dental Teaching Awards Penn Dental faculty, students, and departing Scott Poethig plants. He teaches courses on plant develop- ment, genetic systems, and teaching biology. Dean Dr. Raymond Fonseca were honored by their He has published articles in a number of scholarly journals and sits on the colleagues with awards for distinguished teaching editorial boards of Annual Review of Cell and Developmental Biology, and academic achievement at the School’s Alumni Developmental Biology, The Plant Journal and Evolution and Development. -

St. Ambrose and the Architecture of the Churches of Northern Italy : Ecclesiastical Architecture As a Function of Liturgy
University of Louisville ThinkIR: The University of Louisville's Institutional Repository Electronic Theses and Dissertations 12-2008 St. Ambrose and the architecture of the churches of northern Italy : ecclesiastical architecture as a function of liturgy. Sylvia Crenshaw Schneider 1948- University of Louisville Follow this and additional works at: https://ir.library.louisville.edu/etd Recommended Citation Schneider, Sylvia Crenshaw 1948-, "St. Ambrose and the architecture of the churches of northern Italy : ecclesiastical architecture as a function of liturgy." (2008). Electronic Theses and Dissertations. Paper 1275. https://doi.org/10.18297/etd/1275 This Master's Thesis is brought to you for free and open access by ThinkIR: The University of Louisville's Institutional Repository. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of ThinkIR: The University of Louisville's Institutional Repository. This title appears here courtesy of the author, who has retained all other copyrights. For more information, please contact [email protected]. ST. AMBROSE AND THE ARCHITECTURE OF THE CHURCHES OF NORTHERN ITALY: ECCLESIASTICAL ARCHITECTURE AS A FUNCTION OF LITURGY By Sylvia Crenshaw Schneider B.A., University of Missouri, 1970 A Thesis Submitted to the Faculty of the Graduate School of the University of Louisville in Partial Fulfillment of the Requirements for the Degree of Master of Arts Department of Art History University of Louisville Louisville, Kentucky December 2008 Copyright 2008 by Sylvia A. Schneider All rights reserved ST. AMBROSE AND THE ARCHITECTURE OF THE CHURCHES OF NORTHERN ITALY: ECCLESIASTICAL ARCHITECTURE AS A FUNCTION OF LITURGY By Sylvia Crenshaw Schneider B. A., University of Missouri, 1970 A Thesis Approved on November 22, 2008 By the following Thesis Committee: ____________________________________________ Dr. -
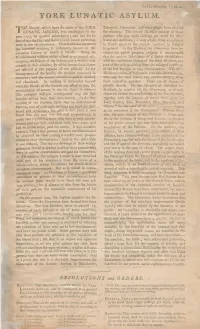
York Lunatic Asylum
York, August i, ISOO. YORK LUNATIC ASYLUM. Charity, which bears the name of the YORK Liverpool, Gloucester, and other places, have adopted THELUNATIC ASYLUM, was established in the the measure. The second Division consists of those year 1777, by general subscription ; and had for its patients who pay eight shillings per week for their first object the Cure and Reliefof such Insane persons as board and medicines; a sum which, from experience, were in low circumstances. How well it has answered is found equal to the expense incurred by Patients the intended purpose, is sufficiently known in the in general. In this Division the Governors have in- extensive County in which it stands. Being an cluded the parish paupers, judging it unreasonable Establishment without either a fund or an annual sub- that the opulent Inhabitants of a Parish should share scription,the friends of the Patients pay a weekly sum with the necefsitous objects of the third Division, any of suitable to their abilities ; by which means the indigent part the savings arising from the enlarged payments are relieved at the expense of the affluent. In the of the few Patients in easy circumstances. The third management of the family, the strictest oeconomy is Division consists of Patients in very low circumstances, utmost is to who for their and receive observed ; and the attention paid decency pay board, nothing from and cleanlinefs. As nothing is demanded beyond their respective parishes. These are all objects of what the friends of the Patients can afford to pay, the pitiable distrefs. On this Division of distrefsed In- accumulation of money is not the object in view.— dividuals, in number 26, the Governors, as already The unhappy sufferers consequently reap the full observed, bestow the overflowings of the first Division, benefits arising from their own money.