District Kathua
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![THE JAMMU and KASHMIR CONDUCT of ELECTION RULES, 1965 Notification SRO 133, Dated 14Th June, 1965, Law Department] [As Amended by SRO 391, Dated 29.9.2014]](https://docslib.b-cdn.net/cover/9916/the-jammu-and-kashmir-conduct-of-election-rules-1965-notification-sro-133-dated-14th-june-1965-law-department-as-amended-by-sro-391-dated-29-9-2014-19916.webp)
THE JAMMU and KASHMIR CONDUCT of ELECTION RULES, 1965 Notification SRO 133, Dated 14Th June, 1965, Law Department] [As Amended by SRO 391, Dated 29.9.2014]
THE JAMMU AND KASHMIR CONDUCT OF ELECTION RULES, 1965 Notification SRO 133, dated 14th June, 1965, Law Department] [As Amended by SRO 391, dated 29.9.2014] In exercise of the powers conferredCONDUCT by section OF ELECTION 168C of theRULES, Jammu 1965 and Kashmir Representation of the People Act, 1957 and in supersession of the Jammu and Kashmir Representation of the People (Conduct of Elections and Election Petitions) Rules, 1957, the Government, after consulting the Election Commission, hereby makes the following rules, namely:- PART I PRELIMINARY 1. Short title and commencement (1) These rules may be called the Jammu and Kashmir ConductRule of 1 Election Rules, 1965. (2) They shall come into force at once. 2. Interpretation (1) In these rules, unless the context otherwise requires,— Rule 2 (a) "Act" means the Jammu and Kashmir Representation of the People Act, 1957; (b) "ballot box" includes any box, bag or other receptacle used for the insertion of ballot paper by voters; 1[(bb) "counterfoil" means the counterfoil attached to a ballot paper printed under the provisions of these rules]; (c) "election by assembly members" means an election to the Legislative Council by the members of the Legislative Assembly; (d) "elector" in relation to an election by Assembly Members, means any person entitled to vote at that election; (e) "electoral roll" in relation to an election by Assembly Members, means the list maintained under section 154 by the Returning Officer for that election; 1 Inserted vide SRO-5 dated 8-1-1972. 186 Rule 2 CONDUCT OF -
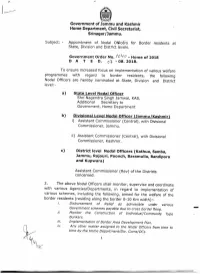
Appointment of Nodal Officers for Border Residents at State, Division
Government of Jammu and Kashmir Home Department,•Civil Secretariat, Srinagar / Jammu . •.. Subject: - Appointment of Nodal Ofticers for Border residents at State, Division and District levels. Government Order No. I v ~ V - Home of 2018 D ATE D. o} - 08. 2018. To ensure increased focus on implementation of various welfare programmes with regard to border residents, the following Nodal Officers are hereby nominated at State, Division and District level:- a) State Level Nodal Officer Shri Nagendra Singh Jamwal, KAS, Additional Secretary to Government, Home Department b) Divisional Level Nodal Officer (Jammu/Kashmir) i) Assistant Commissioner (Central), with Divisional Commissioner, Jammu. ii) Assistant Commissioner (Central), with Divisional Commissioner, Kashmir. c) District level Nodal Officers (Kathua, Samba, lammu, Rajouri, Poonch, Baramulla, Bandipora and Kupwara) Assistant Commissioner (Rev) of the Districts concerned. 2. The above Nodal Officers shall monitor, supervise and coordinate with various Agencies/Departments, in regard to implementation of various schemes, including the following, aimed for the welfare of the border residents (residing along the border 0-10 Km width):- i. Disbursement of Relief as admissible under various Government schemes payable due to cross border firing. - ii. Monitor the Construction of Individual/Community Type Bunkers. iii. Implementation of Border Area Development Plan. iv. Any other matter assigned to the Nodal Officers from time to time by the Home Department/Div. Coms/DCs. 1 ;a. ;.... 3. The Nodal Officers shall maintain close liaison and take steps to resolve issues arising from time to time, in consultation with Department concerned. Besides, the District level Nodal Officers would" furnish a monthly report to the Divisional Level Nodal Officer concerned, who would, in turn, furnish a consolidated monthly report to the State Level Nodal Officer by io" of succeeding month. -

English June.Indd
In this Issue... • Saving the Hangul • Cricket stadium in Srinagar being upgraded • Mongolia keen to tap potential of Leh Berry plant • Kani shawl gets Geographical Indication (GI) tag • Reaching out • Sufi shrine, a symbol of Kashmiriyat • Tourists beat the heat in Patnitop • Leh hosts a ʻGreenʼ Rally • A Kashmir success story Vol. 1, No. 10, July 2010 Saving the Hangul Hangul, the state animal of Jammu and Kashmir, is the only survivor of the Red Deer group in the Indian subcontinent and, its population has been declining over the years due to habitat destruction, overgrazing by domestic livestock and poaching. Alarmed by the fall in numbers of this rare red deer, known scientifically as Cervus Elaphus Hanglu, and locally known as “Hangul”, the Government of Jammu and Kashmir is doing everything possible to save it from extinction. Battling for its survival, the Hangul are now scattered within the Dachigam National Park, which is located under the Zabarwan mountain range on the outskirts of Srinagar. The Dachigam National Park is the natural habitat of the Hangul, though in the summers, some of them cross the boundaries of the national park to graze in the higher mountain reaches. The state government has prepared a plan for Hangul conservation with the help of the Dehradun-based Wildlife Institute of India at a cost of Rs.220 million. The five-year plan has been submitted to the Union Ministry of Environment and Forests for approval. As part of the plan, the state government will buy field equipment, satellite images, GIS hardware and software. It would also build carnivore-proof enclosures, guard huts, watch towers and take steps to stop poachers. -
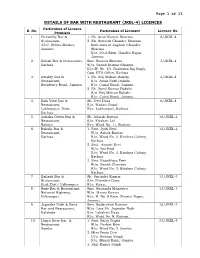
JKEL-4) LICENCES Particulars of Licence S
Page 1 of 13 DETAILS OF BAR WITH RESTAURANT (JKEL-4) LICENCES Particulars of Licence S. No. Particulars of Licensee Licence No. Premises 1. Piccadilly Bar & 1. Sh. Arun Kumar Sharma 2/JKEL-4 Restaurant, 2. Sh. Romesh Chander Sharma 23-C, Nehru Market, both sons of Jagdish Chander Jammu Sharma R/o. 20-A Extn. Gandhi Nagar, Jammu. 2. Satish Bar & Restaurant, Smt. Suman Sharma 3/JKEL-4 Kathua W/o. Satish Kumar Sharma R/o W. No. 10, Chabutra Raj Bagh, Opp. ETO Office, Kathua 3. Kwality Bar & 1. Sh. Brij Mohan Bakshi 4/JKEL-4 Restaurant, S/o. Amar Nath Bakshi Residency Road, Jammu R/o. Canal Road, Jammu. 2. Sh. Sunil Kumar Bakshi S/o. Brij Mohan Bakshi R/o. Canal Road, Jammu. 4. Ravi View Bar & Sh. Devi Dass 8/JKEL-4 Restaurant, S/o. Madan Gopal Lakhanpur, Distt. R/o. Lakhanpur, Kathua. Kathua. 5. Ashoka Green Bar & Sh. Adarsh Rattan 10/JKEL-4 Restaurant, S/o. Krishan Lal Rajouri R/o. Ward No. 11, Rajouri. 6. Bakshi Bar & 1. Smt. Jyoti Devi 12/JKEL-4 Restaurant, W/o. Ashok Kumar Kathua. R/o. Ward No. 3, Krishna Colony, Kathua. 2. Smt . Amarti Devi W/o. Sat Paul R/o. Ward No. 3, Krishna Colony, Kathua. 3. Smt. Kaushlaya Devi W/o. Satish Chander R/o. Ward No. 3, Krishna Colony, Kathua. 7. Kailash Bar & Sh. Surinder Kumar 13/JKEL-4 Restaurant, S/o. Pitamber Dass Kud, Distt. Udhampur. R/o. Katra. 8. Roxy Bar & Restaurant, Smt. Sunanda Mangotra 14/JKEL-4 National Highway, W/o. -

Chapter –I: PERFORMANCE REVIEWS Agriculture Production Department
Chapter –I: PERFORMANCE REVIEWS Agriculture Production Department 1.1 Technology Mission for Integrated Development of Horticulture The Government of India (GOI) approved a Centrally Sponsored Scheme (CSS) ‘Technology Mission (TM) for integrated development of Horticulture’ in Jammu and Kashmir in 200304. The goals of the Mission are to establish convergence and synergy among ongoing governmental programmes in the field of horticulture. The department had not taken an integrated approach by involving all other concerned departments in planning. Utilisation of funds was not proper which had resulted in huge unspent balances at the close of the financial years and loss of assistance to the State. The department had laid more emphasis on area expansion thereby ignoring certain crucial activities like irrigation etc. which had adversely impacted survival of plants and consequently production. The department had failed to provide outlets to the farmers for their produce. Highlights Ø The department had not prepared any perspective plan. Remote Sensing Technology was not used for identification of waste lands for possible exploitation. (Paragraph: 1.1.7) Ø The department had laid more emphasis on ‘area expansion’ thereby spending more funds on the activity at the cost of other components. (Paragraph: 1.1.9.1) Ø The accountal of the excess vegetable seed costing ` 93 lakh procured and issued to the subordinate offices was not shown. (Paragraph: 1.1.9.2) Ø The production of fruit had increased marginally but the productivity per hectare (ha) had declined during 200510. (Paragraph: 1.1.9.6) Ø Marketing facilities had not been provided to the farmers. -

District Census Handbook, Poonch
CENSUS OF INDIA 1961 JAMMU & KASHMIR DISTRICT CENSUS HANDBOOK 9 PDDNCH DISTRICT J. N. ZUTSIU Director of Census Operations, Jammu and Kashmir. THE 1961 CENSUS PUBLICATIONS Part I General . Report on the Census I A General Report including appendix to table A-IV giving the constitution of each urban area for 1961 I B Report on Vital Statistics of the decade I C General Repgrt (Subsidiary Ta'bles) Part II State Census Tables (including Union Tables for the State) on population II A General Population Tables (A-Series) for the State and Primary Census Abstract, including appendix to table A-IV II B Economic Tables (B-Series, Tables I-IX) for the State down to District and all Cities and Town-groups of and above 100,000 population II C Cultural and Migration Tables (C and D Series) for the State down to District and all Cities and Town-groups of and above 100,000 population Part III Household Economic Tables (based on Household Schedules) Part IV Housing and Establishment Tables (E-Series) including .Subsidiary Tables and Report on Housing and Establishment Tables Part V Special Tables for Scheduled Castes (SCT and SC Tables) VA Special Tables on Scheduled Castes as well as reprints from old Census Reports on Castes and Tribes VB Ethnographic nntes Gn Scheduled Castes and backwat:d classes Part VI Village Survey Monographs (each monograph will carry a sub-number 1,23, etc.) Part VII Survey of Handicrafts of the State consisting of Tables for the State, district, tehsil, monographs on individual crafts and general lists of location, mastercraftsmen, etc. -

An Ethnobotanical Study of Medicinal Plants Used by the Locals in Kishtwar, Jammu and Kashmir, India
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by OpenSIUC Ethnobotanical Leaflets 13: 1240-56 , 2009. An Ethnobotanical Study of Medicinal Plants used by the Locals in Kishtwar, Jammu and Kashmir, India Mahesh Kumar, Yash Paul and V. K. Anand Department of Botany, University of Jammu, Jammu.-180006 e-mail. [email protected] Issued October 01, 2009 Abstract This study represents a systematic attempt to explore the knowledge of the native people about plants, which they use to cure diseases. And it is an attempt towards conserving the local knowledge of people to plants. This paper presents a list and uses of some medicinal plants distributed in the high altitude district Kishtwar in Jammu and Kashmir. The list was prepared during an ethno-botanical survey of the region from December 2007 to January, 2009. This paper provides information about 71 ethno-medicinally useful plants grown in this region. In this paper, family, botanical name, local name, ethnomedicinal uses are given for each plant. Introduction It is documented that 80% of the world population has faith in traditional medicines, particularly plant drugs for their primary healthcare (Kala et al., 2006). The use of plants for medicinal purposes and human sustenance has been in practice in India since the Vedic age. The earliest mention of the medicinal use of the plants is found in the Rigveda, 1500-400 BC, Athurveda 1500 BC, Upnishada 1000-600 BC (Chauhan, 1999). In India about 17000 species of higher plants out of which 7500 are known for medicinal uses (Shiva, 1996). -

Page1final.Qxd (Page 3)
MONDAY, APRIL 13, 2020 (PAGE 4) DAILY EXCELSIOR, JAMMU From page 1 First Army jawan, second doctor, Tablighi Coronavirus cases inch closer to 9000 contact among 4 more +ve in Jammu; total 48 have been cured and discharged activities like in the farming sec- over hundreds of miles to their plan to improve the country’s so far. tor in regions with no COVID- home districts. economic activity and provide Seventeen persons were tested police station headed by Inspector According to the latest 19 cases. In the report titled "South liquidity in the hands of the peo- positive for COVID-19 in Kashmir Chanchal Singh have sealed Bohri Union Health Ministry update, The Centre in consultation Asia Economic Update: Impact ple. today taking total number of cases Chowk and surrounding areas as as many as 918 COVID-19 with states is moving to restart of COVID-19", the report at the “These new activities are in the Valley to 197 and that of the they were declared as Red Zones cases and 34 deaths have been economic activities in a graded same time said migrant workers essential to improve the eco- Union Territory of Jammu and by the administration after the doc- reported in the last 24 hours, tak- manner in what is seen as a returning home could become nomic activity and provide liq- Kashmir to 245. However, out of tor tested positive. ing the total number of such nuanced change in strategy from vectors carrying the coronavirus uidity in the hands of the peo- 245 total cases, number of active A 29-year old resident of cases to 8,447 and the fatalities saving lives a month ago to sav- to unaffected states and villages ple,” the DPIIT said in its letter cases stood at 235-44 in Jammu Jawahar Nagar, Satwari, who had to 273. -

List of Specialized Msme Business Units
LIST OF SPECIALIZED MSME BUSINESS UNITS NAME SOL_ID EMAIL ALPHA_CODE ADDRESS ADDRESS2 District State PIN Phone 2313490, AIR CARGO, Metro International 7298004201, 1 SRINAGAR 0252 [email protected] AIRCAR Office Complex Rajbagh Srinagar J&K 190008 2313485, 2312757 01924- AKHNOOR, Main Bazar 252237,252399,9419 2 JAMMU 0024 [email protected] AKHNOR Akhnoor Akhnoor Jammu J&K 181201 139852 BAGHI ALI MARDAN, Baghi Ali Mardan Baghi Ali Mardan 2424751, 3 SRINAGAR 0356 [email protected] MARDAN Khan Khan Srinagar J&K 190011 7298004207 0194- BARZULLA, 2432777,729800421 4 SRINAGAR 0278 [email protected] BAGAAT Baagat Baagat Chowk srinagar J&K 0 BHADERWAH Main Market, 5 MAIN,DODA 0030 [email protected] BHADAR BHADERWAH MAIN Bhaderwah Doda J&K 182222 01997-244247 BIJBHERA, National Highway 6 ANANTNAG 0091 [email protected] BBHARA Bijbehara BijBehara Anantnag J&K 192124 9906645399 Main Bazar, 01921-222027, 7 BILAWAR, KATHUA 0107 [email protected] BILWAR BILAWAR, KATHUA Bilawar Kathua J&K 180542 7298004615 DULHASTI, DULHASTI 8 KISHTWAR 0388 [email protected] DHASTI DULHASTI,KISHTWAR KISHTWAR Kishtwar J&K 182204 7298004441 0194-2416881, GANDERBAL, Beehama 2130336, 9 SRINAGAR 0081 [email protected] GANDER Ganderbal Ganderbal Ganderbal J&K 191201 7298004225 Opp. IFCA 2480119,2481379,94 Botteling 19177999,72980043 10 GANGYAL, JAMMU 0116 [email protected] GNGYAL Gangyal Company Jammu J&K 180010 79 GOVINDSAR, Opp. Industrial 01922-233165, 11 KATHUA 0144 [email protected] GOVIND Govindsar Estates Kathua J&K 184102 7298004759 Near L.I.C Of GUJAR MARKET, -

Kupwara District
Ground Water Information Booklet- Kupwara District Government of India Ministry of Water Resources CENTRAL GROUND WATER BOARD GROUND WATER INFORMATION BOOKLET KUPWARA DISTRICT, JAMMU & KASHMIR NORTH WESTERN HIMALAYAN REGION JAMMU March 2013 Ground Water Information Booklet- Kupwara District GROUND WATER INFORMATION BOOKLET KUPWARA DISTRICT, JAMMU & KASHMIR CONTENTS DISTRICT AT A GLANCE 1.0 INTRODUCTION 2.0 CLIMATE & RAINFALL 3.0 GEOMORPHOLOGY & SOIL TYPES 4.0 GROUND WATER SCENARIO 4.1 Geology 4.2 Hydrogeology 4.3 Depth to water level 4.4 Ground Water Resources 4.5 Ground Water Quality 4.6 Status of Ground Water Development 5.0 GROUND WATER MANAGEMENT STRATEGY 5.1 Ground Water Development 5.2 Water Conservation & Artificial Recharge 6.0 GROUND WATER RELATED ISSUES & PROBLEMS 7.0 AWARENESS & TRAINING ACTIVITY 8.0 AREAS NOTIFIED BY CGWA / SGWA 9.0 RECOMMENDATIONS Ground Water Information Booklet- Kupwara District KUPWARA DISTRICT AT A GLANCE Sl. No. ITEMS STATISTICS 1. GENERAL INFORMATION i) Geographical area (sq km) 2379 ii) Administrative Divisions (2001) • Number of Tehsil & Sub-tehsils 3 • Number of CD Blocks 11 • Number of Panchayats 234 • Number of Villages 370 iii) Population (2001 Census) • Total population 6,50,393 persons • Population Density (pers/sq km) 237 • Muslim & others Population 97.37% & 2.63% • Sex Ratio 906 iv) Average Annual Rainfall (mm) 869 mm 2. GEOMORPHOLOGY Major Physiographic units • High Karewa Plateau lands • Sharp ridges of hard rock • Intervening valleys & River Terraces- Lolab valleys that is 6 Kms long and 4.4 kms wide is most important. Average Range 1635 m amsl Major Drainages • Kishan Ganga basin • Pohru river is the distributaries of Jhelum • Nanchar Nala drains Eastern part • Pohru river basin • Kahmil Nala drains Western part 3. -

Important Stadiums in India & World
Is Now In CHENNAI | MADURAI | TRICHY | SALEM | COIMBATORE | CHANDIGARH | BANGALORE|NAMAKKAL|ERODE|PUDUCHERRY www.raceinstitute.in | www.bankersdaily.in IMPORTANT STADIUMS IN INDIA & WORLD Chennai: #1, South Usman Road, T Nagar. | Madurai: #24/21, Near Mapillai Vinayagar Theatre, Kalavasal. | Trichy: opp BSNL office, Juman Center, 43 Promenade Road, Cantonment. | Salem: #209, Sonia Plaza / Muthu Complex, Junction Main Rd, State Bank Colony, Salem. | Coimbatore #545, 1st floor, Adjacent to SBI (DB Road Branch), Diwan Bahadur Road, RS Puram, Coimbatore (Kovai) – 641002 | Chandigarh: SCO 131-132 Sector 17C. | Bangalore. H.O: 7601808080 / 9043303030 | www.raceinstitute.in Important Stadiums in India: 1. Wankhede Stadium Mumbai, Maharashtra Cricket 2. Feroz Shah Kotla Ground Delhi Cricket 3. M.A. Chidambaram Stadium Chennai , Tamil Nadu Cricket 4. Eden Gardens Kolkata, West Bengal Cricket 5. Gymkhana Ground Mumbai , Maharashtra Cricket 6. Jsca Stadium Ranchi, Jharkhand Cricket 7. Subrata Roy Sahara Stadium Pune , Maharashtra Cricket 8. Rajiv Gandhi International Stadium Hyderabad, Telangana Cricket 9. Barkatullah Khan Stadium Jodhpur, Rajasthan Cricket 10. Jawahar Lal Nehru Stadium Kochi, Kerala Multipurpose ( football (soccer) and cricket) 11. K.D. Singh Babu Stadium Lucknow, Uttar Pradesh Multipurpose 12. Fatorda Stadium Margao, Goa Football & Cricket 13. Maulana Azad Stadium Jammu, Jammu & Kashmir Cricket 14. Indira Priyadarshini Stadium Visakhapatnam, Andhra Cricket Pradesh 15. University Stadium Thiruvananthapuram, Multi-purpose Kerala 16. Roop Singh Stadium Gwalior , Madhya Pradesh Cricket 17. Nehru Stadium Pune, Maharashtra Multipurpose 18. Jawahar Lal Nehru Stadium Delhi Multipurpose 19. Keenan Stadium Jamshedpur , Jharkhand Multipurpose 20. Sardar Patel Stadium Ahmedabad , Gujarat Cricket 21. Moti Bagh Stadium Vadodara , Gujarat Cricket 22. Sher-I-Kashmir Stadium Srinagar, Jammu & Cricket Kashmir 23. -

The Jammu and Kashmir Reorganisation Bill, 2019
1 AS PASSED BY THE RAJYA SABHA ON THE 5TH A UGUST, 2019 Bill No. XXIX-C of 2019 THE JAMMU AND KASHMIR REORGANISATION BILL, 2019 (AS PASSED BY THE RAJYA SABHA) A BILL to provide for the reorganisation of the existing State of Jammu and Kashmir and for matters connected therewith or incidental thereto. BE it enacted by Parliament in the Seventieth Year of the Republic of India as follows:— PART-I PRELIMINARY 1. This Act may be called the Jammu and Kashmir Reorganisation Act, 2019. Short title. 5 2. In this Act, unless the context otherwise requires,— Definitions. (a) “appointed day” means the day which the Central Government may, by notification in the Official Gazette, appoint; (b) “article” means an article of the Constitution; (c) “assembly constituency” and “parliamentary constituency” have the same 43 of 1950. 10 meanings as in the Representation of the People Act, 1950 (43 of 1950); (d) “Election Commission” means the Election Commission appointed by the President under article 324; (e) “existing State of Jammu and Kashmir” means the State of Jammu and Kashmir as existing immediately before the appointed day, comprising the territory which 2 immediately before the commencement of the Constitution of India in the Indian State of Jammu and Kashmir; (f) “law” includes any enactment, ordinance, regulation, order, bye-law, rule, scheme, notification or other instrument having, immediately before the appointed day, the force of law in the whole or in any part of the existing State of Jammu and Kashmir; 5 (g) “Legislative Assembly” means