To Test Or Not: Occurrence of Sickle Cell Trait
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Reflecting on the First Two COVID-19 Deaths in Uganda: a Public Health Perspective
Volume 12 • Number 2 • June 2021 • em00773 JOURNAL OF CLINICAL AND BRIEF REPORT EXPERIMENTAL INVESTIGATIONS Reflecting on the First Two COVID-19 Deaths in Uganda: A Public Health Perspective Joseph Kawuki 1,2*, Quraish Sserwanja 3, Nathan Obore 2, Zixin Wang 1, Joseph Tak Fai Lau 1 1 Centre for Health Behaviours ABSTRACT Research, Jockey Club School of Public Health and Primary Care, COVID-19 being a rapidly evolving pandemic, early lessons from the first deaths must be learnt Faculty of Medicine, The Chinese to help feed into the public health guidelines. This article, therefore, aims to present the first University of Hong Kong, Hong two deaths due to COVID-19 in Uganda and their public health relevance. This is a case study Kong - SAR, China of the first two COVID-19 deaths reported in Uganda, and the events were prospectively 2 Department of Global Health, documented. The first case was a 34-year-old female and support staff at a health center II. School of Public Health, Southeast She first presented with COVID-19 like symptoms before dying on 21st July 2020. The second University, Nanjing, 210009, Jiangsu case was an 80 years old female, who also presented with COVID-19 like symptoms before Province, China dying on 24th July 2020. The postmortem samples of both cases were confirmed positive for 3 Monitoring and Evaluation COVID-19. This study identifies a need for timely identification and testing of COVID-19 Department, Doctors with Africa, Juba, South Sudan suspects, strengthening of health center capacity, as well as more awareness for effective prevention and control of COVID-19. -
UNVEILING the CULTURAL and HERITAGE TREASURES of BUGISU REGION 1 2 UNVEILING the CULTURAL and HERITAGE TREASURES of BUGISU REGION Table of Contents
UNVEILING THE CULTURAL HERITAGE TREASURES OF BUGISU This monument of the legendary Wandulu wa Netuwa depicts the typical appearance of a youth in transition to manhood in Masaabaland UNVEILING THE CULTURAL AND HERITAGE TREASURES OF BUGISU REGION 1 2 UNVEILING THE CULTURAL AND HERITAGE TREASURES OF BUGISU REGION Table of Contents Foreword ii Namasho Bull Fighting 12 Introduction 1 The Namasho Cultural Site 13 The Partnership with the Cross-Cultural Foundation of The Nashula Cultural Site 14 Uganda (CCFU) 2 The Namisindwa Cave 15 Opening up the research potential 2 The Semei Kakungulu Residence and Tombs 16 Key Cultural Heritage Resources in the Bugisu Region 3 The Bukusu Prayer Mountain 17 The Biritanyi George 3 The Mutoto Cultural Site 19 The Sisiyi Falls 4 The Nusu Hill 20 The Zebubu Cave 5 The Wanale (Nkonkonjeru) Ridge 21 The Nakoko Cave 6 Key Historic buildings 22 Kagyere Falls I 7 Mt. Elgon Culture and History Museum 23 Kagyere Falls II 7 Conclusion 26 Kamashengelo 8 The Lwandubi Inemba Site 9 The Nalufutu Cultural Site 11 UNVEILING THE CULTURAL AND HERITAGE TREASURES OF BUGISU REGION i Foreword It is with great pleasure that I, on behalf of Mt. Elgon Culture and History Museum of the product diversification strategy for the development of Community-Based (MECHM), present these Research Findings of an exercise that was aimed at Tourism (CBT). strengthening the capacity of the museum managers to carry out research on cultural resources. In Bugisu Region many heritage and cultural sites remain We encourage stakeholders and other interested parties to read this publication virgin and not mapped for appreciation and tourism exploitation. -
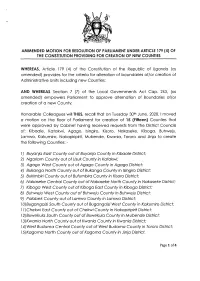
(4) of the Constitution Providing for Creation of New Counties
AMMENDED MOTTON FOR RESOLUTTON OF PARLTAMENT UNDER ARTTCLE 179 (4) OF THE CONSTITUTION PROVIDING FOR CREATION OF NEW COUNTIES WHEREAS, Ariicle 179 (a) of the Constitution of the Republic of Ugondo (os omended) provides for the criterio for olterotion of boundories oflor creotion of Administrotive Units including new Counties; AND WHEREAS Section 7 (7) of the Locql Governments Act Cop. 243, (os omended) empowers Porlioment to opprove olternotion of Boundories of/or creotion of o new County; Honoroble Colleogues willTHUS, recoll thot on Tuesdoy 30rn June, 2020,1 moved o motion on the floor of Porlioment for creotion of I5 (Fitteen) Counties thot were opproved by Cobinet hoving received requests from the District Councils of; Kiboole, Kotokwi, Agogo, lsingiro, Kisoro, Nokoseke, Kibogo, Buhweju, Lomwo, Kokumiro, Nokopiripirit, Mubende, Kwonio, Tororo ond Jinjo to creote the following Counties: - l) Buyanja Eost County out of Buyanjo County in Kibaale Distric[ 2) Ngoriom Covnty out of Usuk County in Kotakwi; 3) Agago Wesf County out of Agogo County in Agogo District; 4) Bukonga Norfh County out of Bukongo County in lsingiro District; 5) Bukimbiri County out of Bufumbira County in Kisoro District; 6) Nokoseke Centrol County out of Nokoseke Norfh County in Nokoseke Disfricf 7) Kibogo Wesf County out of Kibogo Eost County in Kbogo District; B) Buhweju West County aut of Buhweju County in Buhweju District; 9) Palobek County out of Lamwo County in Lamwo District; lA)BugongoiziSouth County out of BugongoiziWest County in Kokumiro Districf; I l)Chekwi Eosf County out of Chekwi County in Nokopiripirit District; l2)Buweku/o Soufh County out of Buweku/o County in Mubende Disfricf, l3)Kwanio Norfh County out of Kwonio Counfy in Kwonio Dislricf l )West Budomo Central County out of Wesf Budomo County inTororo Districf; l5)Kogomo Norfh County out of Kogomo County in Jinjo Districf. -

Proceedings of the VIP4FS Project Mid-Term Review in Kapchorwa and Manafwa Districts, Uganda
Proceedings of the VIP4FS Project Mid-term Review in Kapchorwa and Manafwa districts, Uganda Developing Value Chain Innovation Platforms to Improve Food Security in East and Southern Africa (VIP4FS Project - FST/2014/093) World Agroforestry Centre, Nairobi 15th November 2017 1 Contributing authors Jude Sekatuba1, Joan Kimaiyo2, Clement Okia3 and Prossy Isubikalu4 1National Forestry Resources Research Institute (NaFORRI), P.O. Box 1752, Kampala 2World Agroforestry Centre (ICRAF), P.O. Box 30677-00100 Nairobi 3World Agroforestry Centre (ICRAF), Uganda Country Office, P.O. Box 26416, Kampala 4College of Agricultural & Environmental Sciences (CAES), Makerere University, P.O. Box 7062, Kampala Correct citation Sekatuba J, Kimaiyo J, Isubikalu Prossy & Okia C.A (2017) Proceedings of the value chain innovation platforms for food security project in Kapchorwa and Manafwa districts, Uganda. World Agroforestry Centre, Nairobi, Kenya, 27pp. Project partners 2 Acronyms ACIAR Australian Centre for International Agricultural Research AFCA African Fine Coffees Association AI artificial insemination CAO Chief Administrative Officer IPs Innovation Platforms KACSOA Kapchorwa Civil Society Alliance LC3 Local Council 3 Mak Makerere University MERECEP Mt. Elgon Regional Ecosystem Conservation Project MTR Mid-Term Review NaFORRI National Forestry Resources Research Institute NARO National Agricultural Research Organisation NUSAF Northern Uganda Social Action Fund OWC Operation Wealth Creation PCs Planned Comparisons RDC Resident District Commissioner SACCO Savings and Credit Cooperative Organization UCDA Uganda Coffee Development Authority UWA Uganda Wildlife Authority VIP4FS Value chain innovation platform for food security project 3 Table of Contents Acronyms 3 Day One: Field visit to project sites in Kapchorwa district 5 Courtesy call Kapchorwa District Local Government 5 Tegeres Dairy Innovation Platform 6 Tegeres Honey Innovation Platform 10 Mt. -

EPISTLE from the UGANDA YEARLY MEETING (UYM) FRIENDS CHURCH (QUAKERS) August 30 – September 3, 2017 to Friends Everywhere
EPISTLE FROM THE UGANDA YEARLY MEETING (UYM) FRIENDS CHURCH (QUAKERS) August 30 – September 3, 2017 To Friends everywhere Dear Friends, We send greetings from the Uganda Yearly Meeting (UYM). We (more than 250 Quakers from Uganda, Kenya & Rwanda) have come together from August 30 to September 3, 2017 as a Yearly Meeting at Sibuse Friends Church. The UYM Presiding Clerk Paul Kuloba welcomed the delegates to the conference. This is the 31st Session. It is a very historic conference because Quakerism spread into Uganda from Sibuse. By 1945, there were Quaker churches in Sibuse and Nabiswa to the East, Kigumba to the West and Nang’oma and Kampala to the Central by 1948. The venue, the newly constructed Church, a 500-seater is set in the lush foothills of the Mt. Elgon (below). It is 5km from the Uganda/Kenya Lwakhakha border and 37km to Mbale, Uganda’s Eastern regional capital. Politically, it is located in Bubutu Sub-County, Namisindwa District. Our theme has been “I will uphold you with my righteous right hand.” (Isaiah 41:10). The main speaker, the UYM General Superintendent Samuel Wefafa has urged the congregants to live righteous lives so that God can “uphold you with my righteous right hand”. We have listened to and discussed other topics including Stress Management, Quakerism, HIV/AIDS/Hepatitis, Gifts of the Holy Spirit, Armour of God, Church Planting and others. We have engaged in informative group discussions on Missions, Evangelism, Discipleship, Africans are religiously notorious, God as a commodity of Trade, Cult/Occult and others. We have been blessed with international visitors including a team from Kakamega Yearly Meeting led by Eileen Malova, Lugulu Yearly Meeting represented by Evelyn Cheroh Nyongesa, Rwanda Yearly Meeting represented by Emmanuel Ndazimenyera. -

Re Ecting on the Rst Two COVID-19 Deaths in Uganda
Reecting on the rst two COVID-19 deaths in Uganda: a public health case study Joseph Kawuki ( [email protected] ) Centre for Health Behaviours Research, JC School of Public Health and Primary Care, Faculty of Medicine, the Chinese University of Hong Kong Quraish Sserwanja Monitoring and Evaluation Department, Doctors with Africa, Juba, South Sudan Nathan Obore Department of Global Health, School of Public Health, Southeast University, Nanjing, 210009, Jiangsu Province, China Johnson Wang Centre for Health Behaviours Research, JC School of Public Health and Primary Care, Faculty of Medicine, the Chinese University of Hong Kong Joseph Lau Centre for Health Behaviours Research, JC School of Public Health and Primary Care, Faculty of Medicine, the Chinese University of Hong Kong Short Report Keywords: COVID-19, First death, Case study, Uganda Posted Date: August 4th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-52459/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/9 Abstract Objective: COVID-19 being a rapidly evolving pandemic, early lessons from the rst deaths must be learnt to help feed into the public health guidelines. This study, therefore, aims to present the rst two deaths due to COVID-19 in Uganda and their public health relevance. Cases: The rst case was a 34-year female and support staff at a health center II. She rst presented with COVID-19 like symptoms before dying on 21st July 2020. The second case was an 80 years old female, who also presented with COVID-19 like symptoms before dying on 24th July 2020. -
Survey and Management of Potato Pests in Uganda Final Report: December 2019 Submitted to MEL (CC3.1.2.2- Output No
Survey and management of potato pests in Uganda Final report: December 2019 Submitted to MEL (CC3.1.2.2- output no. 12557) Submitted by: Dr. Laura Cortada (IITA), Dr. Danny Coyne (IITA); Dr. Valentine Nakato (IITA); Joseph Kisitu (MSc), Dr. Arthur Wasukira (NARO); Dr. Joshua Okonya (CIP) RESEARCH PROGRAM ON Roots, Tubers and Bananas Survey and management of potato pests in Uganda December 2019 Survey and management of potato pests in Uganda © International Potato Center 2019 ISBN: 978‐92‐9060‐547-8 DOI: 10.4160/9789290605478 CIP publications contribute important development information to the public arena. Readers are encouraged to quote or reproduce material from them in their own publications. As copyright holder CIP requests acknowledgement and a copy of the publication where the citation or material appears. Please send a copy to the Communications Department at the address below. International Potato Center P.O. Box 1558, Lima 12, Peru [email protected] • www.cipotato.org Citation: Cortada, L., Coyne, D., Nakato, V., Kisitu, J., Wasukira, A., and Okonya, J. (2019). Survey and management of potato pests in Uganda (CC3.1.2.2 - output no. 12557). International Potato Center: Lima, Peru. Corresponding author: Laura Cortada, International Institute of Tropical Agriculture, [email protected] Cover design Communications department December 2019 Note: This research was funded through a grant from the International Fertilizer Development Center (www.ifdc.org) to the International Institute of Tropical Agriculture. The research was conducted -

Developed Special Postcodes
REPUBLIC OF UGANDA MINISTRY OF INFORMATION & COMMUNICATIONS TECHNOLOGY AND NATIONAL GUIDANCE DEVELOPED SPECIAL POSTCODES DECEMBER 2018 TABLE OF CONTENTS KAMPALA 100 ......................................................................................................................................... 3 EASTERN UGANDA 200 ........................................................................................................................... 5 CENTRAL UGANDA 300 ........................................................................................................................... 8 WESTERN UGANDA 400 ........................................................................................................................ 10 MID WESTERN 500 ................................................................................................................................ 11 WESTNILE 600 ....................................................................................................................................... 13 NORTHERN UGANDA 700 ..................................................................................................................... 14 NORTH EASTERN 800 ............................................................................................................................ 15 KAMPALA 100 No. AREA POSTCODE 1. State House 10000 2. Parliament Uganda 10001 3. Office of the President 10002 4. Office of the Prime Minister 10003 5. High Court 10004 6. Kampala Capital City Authority 10005 7. Central Division 10006 -

Statistical Abstract 2018
---------------------------------------------------- < The Republic of Uganda MINISTRY OF LOCAL GOVERNMENT Ministry of Local Government, Plot 1, Pilkington Road, Worker’s House P.O. Box 7037, Kampala (U) Tel: +256-414-256533 Email:[email protected]; Website:http://molg.go.ug December 2018 Ministry of Local Government (MoLG) Statistical Abstract 2018 Statistical Abstract Ministry of Local Government December 2018 i Ministry of Local Government (MoLG) Statistical Abstract 2018 Districts of Uganda ii Ministry of Local Government (MoLG) Statistical Abstract 2018 Foreword Hon. Col. Tom Butime Minister of Local Government The Mandate of the Ministry of Local Government is to guide, harmonize, mentor and advocate for all Local Governments in support of Government’s vision of bringing about socio-economic transformation of the country. The Ministry is responsible for mentoring, compliance inspection and support supervision of Local Governments. In order to fulfil this mandate, quality statistics are required to measure development outcomes, identify development issues, inform policy formulation, and facilitate planning, decision making, implementation, monitoring and evaluation of the impact of development programmes in the LGs. It is on this basis that the Ministry of Local Government, with support from Uganda Bureau of Statistics, adopted a strategic approach towards managing data and statistics of the Ministry. This necessitated development and implementation of a five year Strategic Plan for Statistics (SPS) covering the period 2015/16 – 2019/20 to act as a building block for the Plan for National Statistical Development (PNSD) framework. The plan is aimed at enhancing data quality and use and comprehensiveness of statistics produced by the ministry. In line with the MoLG-SPS, the Ministry is required to produce an Annual Statistical abstract.The MoLG Statistical Abstract 2018 consolidates data relating to its various output indicators. -

Regional Report Central, East and Southern Africa 2019
Central, East and Southern Africa Regional Report 2019 Swisscontact Swiss Foundation for Technical Cooperation We are a leading partner organisation for the implementation of international development projects. Founded in 1959 and registered under Swiss law, we are an independent non-profit organisation. We are politically and denominationally neutral. Our Mission We promote inclusive economic, social and ecological development to make an effective contribution towards sustainable and widespread prosperity in developing and emerging economies. With this objective in mind, we offer the chance to economically and socially disadvantaged people to improve their lives on their own initiative. Our Values • We believe that people, even in dire conditions have the and Beliefs ability and will to act and liberate themselves from the shackles of poverty. However, this is only possible in an enabling environment and level playing field. • We make an effective contribution to improve the framework conditions for sustainable development through the facilitation of access to skills, knowledge, markets, technologies and financial services. • We believe that balanced private sector and market- driven approaches in the context of an environmentally and socially sustainable market economy offer the best conditions for people to fulfill their potential and make sustainable development possible. • We act responsibly and respect people in their own contexts, societies and cultures. • We stand for professional quality and high ethical standards in our activities. What we do • We strengthen the competencies of people, improving their employability • We increase the competitiveness of enterprises growing their business • We foster social and economic systems promoting inclusive development What we offer • Project Implementation • Advisory Services • Training • Applied Research My business turnover has increased fivefold since the start of my involvement with the PROMOST project in April 2018. -

Lot 1 Tors Implementation Supervision of Catchment Mgt
THE REPUBLIC OF UGANDA MINISTRY OF WATER AND ENVIRONMENT DIRECTORATE OF WATER RESOURCES MANAGEMENT INTEGRATED WATER MANAGEMENT AND DEVELOPMENT PROJECT (IWMDP) TERMS OF REFERENCE FOR LOT 1: CONSULTANCY SERVICES FOR TECHNICAL SUPERVISION OF IMPLEMENTATION OF CATCHMENT MANAGEMENT MEASURES IN LWAKHAKHA SUB-CATCHMENT SEPTEMBER 2020 1 INTRODUCTION Government of Uganda, with funding from the World Bank is implementing Integrated Water Management and Development Project which provides support to catchment management and activities in sub-catchments of Lwakhakha (Mpologoma catchment), Lake Okolitorom and Apeduru Apapai (Awoja catchment), Kochi (Albert Nile catchment), and Aswa II (Aswa catchment). The project supports implementation of catchment management measures, including soil and water conservation, eco-system protection and restoration; livelihood improvement for the affected communities and supporting stakeholder engagement and the establishment of micro catchment structures for sustainable management of the interventions. Implementation of the IWMDP is fully integrated within the government structure. Thus, the water resources management component of the project is implemented by the Directorate of Water Resources Management (DWRM) through its various departments and the relevant Water Management Zones (WMZs). The task teams are composed of staff from DWRM, WMZs, relevant MWE departments and agencies, and other government ministries and agencies. The services and works for implementation of project activities will be outsourced to Buwasa Dola BULAMBULI consultants and contractors. BulujewaZesui Makerere KWEEN Namanyonyi SIRONKO Buteza T.C Namwani Bunamubi Bunakhaya Bunaporo Bushunya These Terms of Reference are for technical supervision of Bumboyi Bushiribo Mooni Buchibino implementation of catchment management measures in Lwakhakha ¸ Busanza Bukalasi Bushika Busano Bukigai MBALE BUDUDA sub-catchment in Mpologoma catchment in Kyoga Water Shanzou Kuwushu Nangako Konokoyi Bumayoka Busai Bududa Namaitsu Bubita Management Zone. -

UWEP) Ministry of Gender, Labour and Social Development Simbamanyo House, Plot 2, George Street
BUSINESS & TENDERS UGANDA WOMEN ENTREPRENEURSHIP PROGRAMME (UWEP) Ministry of Gender, Labour and Social Development Simbamanyo House, Plot 2, George Street. P.O Box 7136, Kampala Tel: 041-4 343572/ 0414 699219/ 0414 699220, Facebook: @uwep.mglsd ON THE OCCASION TO MARK THE International Women’s Day, 2021 H.E. Yoweri Kaguta Museveni HON. Frank K. Tumwebaze HON. Mutuuzo Peace Regis Aggrey David Kibenge Winifred Komuhangi Masiko THE PRESIDENT OF THE MINISTER OF GENDER, LABOUR MINISTER OF STATE FOR PERMANENT SECRETARY National Programme REPUBLIC OF UGANDA AND SOCIAL DEVELOPMENT GENDER AND CULTURE Coordinator - UWEP Programme Background: h) The group approach has given Women an opportunity to improve Over the years, majority of women in Uganda have been disenfranchised knowledge and skill through mentoring each other. The greater from the formal business sector due to limited access to affordable involvement of the Women in mobilization, sensitization, prioritization credit, limited technical knowledge on business entrepreneurship and and planning for their needs, implementation and monitoring and management, limited access to markets as well as information regarding evaluation of Programme activities has created a sense of business opportunities. To address that problem, Government of Uganda empowerment and confidence to take charge of their destiny. in the FY 2015/2016 initiated the Uganda Women Entrepreneurship Programme (UWEP) with a core goal of empowering Ugandan women to improve their income levels and their contribution to economic