A. Battery Or Negligence? a Battery Action
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wrongful Life in the Age of CRISPR-CAS: Using the Legal Fiction of “The Conceptual Being” to Redress Wrongful Gamete Manipulation
Wrongful Life in the Age of CRISPR-CAS: Using the Legal Fiction of “The Conceptual Being” to Redress Wrongful Gamete Manipulation Barbara Pfeffer Billauer J.D., M.A., Ph.D.* ABSTRACT Virtually all ‘wrongful life’ actions (claims brought by children for pre-birth injuries) are denied. The basis for this doctrine pivots around the refusal to allow recompense for actions which cause harm, but also result in the child’s birth. We, therefore, are faced with a legal lacuna, where children suffering serious harms as a result of the latest reproductive technologies are legal orphans. This Article details the avenues of potential harm caused by modern reproductive technologies, which I call wrongful genetic manipulation (WGM), where the injured child would have no right of action. To address this void, I create a novel remedy via a legal fiction, “the conceptual being,” which would enable these children to bypass current restrictions and claim an expanded class of damages, including pain and suffering, emotional injury, and unjust enrichment. *About the author: Dr. Billauer holds academic appointments at the University of Porto, Portugal, where she is a Professor in the International Program on Bioethics, and the Institute of World Politics in Washington, D.C., where she is a research Professor of Scientific Statecraft. She has advanced degrees in law and public health and sits on the UNESCO committee currently compiling a Casebook on Bioethics. She has also edited Professor Amnon Carmi’s Casebook on Bioethics for Judges. Prior to transitioning to academia, Dr. Billauer practiced medical malpractice, toxic tort, and products liability law. -

HB 651 Recovery of Damages in Claims for Medical Negligence SPONSOR(S): Roach TIED BILLS: IDEN./SIM
HOUSE OF REPRESENTATIVES STAFF ANALYSIS BILL #: HB 651 Recovery of Damages in Claims for Medical Negligence SPONSOR(S): Roach TIED BILLS: IDEN./SIM. BILLS: SB 1112 REFERENCE ACTION ANALYST STAFF DIRECTOR or BUDGET/POLICY CHIEF 1) Civil Justice & Property Rights Subcommittee 18 Y, 0 N Brascomb Jones 2) Judiciary Committee SUMMARY ANALYSIS A "wrongful death" action arises when a person dies from injuries sustained as a result of a wrongful act or omission by the defendant. In a wrongful death action, Florida's Wrongful Death Act limits the types of damages recoverable by certain parties as follows: The deceased’s estate may recover for: o Lost wages, benefits, and other earnings; o Medical and funeral expenses that were paid by the estate; and o The value the estate could reasonably have been expected to acquire if the deceased had lived. Specified family members may recover for: o The value of support and services the deceased provided; o Loss of companionship and guidance; o Mental and emotional pain and suffering, in specified cases; and o Compensation for medical and funeral expenses the family member has paid for the deceased. In an ordinary wrongful death action (such as a suit based on a death caused by an automobile accident), parents can recover for their mental pain and suffering for the loss of an adult child when there is no surviving spouse or child. However, when the wrongful death action is based on a medical malpractice claim, parents cannot recover for their mental pain and suffering for the loss of an adult child. -
Toxic Trespass: Lead Us Not Into Litigation
toxic trespass: lead us not into litigation 44 by Steven N. Geise and Hollis R. Peterson Since the chemical revolution began to unfold in the 1950s, people have ingested hundreds of toxic substances—knowingly or not. Our bodies carry chemicals found in the products and processes we use or to which we are exposed. Many toxins take up residence in body fat, where they may remain for decades; others are absorbed into the body and quickly metabolized and excreted. Winds and water currents can carry persistent chemicals thousands of miles until they find a home in our blood- streams. Just by living in an industrialized society, we all carry a sampling of the chem- ical cocktail created by our surroundings. As modern science advances, biomonitor- ing data is able to detect the presence of specific toxins. But science cannot always inform us about how the chemi- cals were introduced, how long they have been there, or whether they pose a legiti- mate health risk. If not for recent develop- ments in detection, we might never know that our bodies harbor such chemicals. 55 Nevertheless, creative litigants are forcing courts to deal with (“CELDF”) has proposed a strict-liability model ordinance to a new wave of toxic tort claims seeking to make chemicals local legislators that recognizes “that it is an inviolate, funda- in a person’s bloodstream an actionable offense. This cause mental, and inalienable right of each person … to be free from of action is known as “toxic trespass.” Courts must decide involuntary invasions of their bodies by corporate chemicals.” whether the mere presence of chemicals in an individual Corporate Chemical Trespass Ordinance, http://www.celdf.org/ gives rise to civil liability when the individual has no diag- Ordinances/CorporateChemicalTrespassOrdinance/tabid/257/ nosed injury and the causal link between the exposure and Default.aspx (web sites last visited February 6, 2009). -

The Standard of Care in Malpractice Cases Irvin Sherman
Osgoode Hall Law Journal Article 4 Volume 4, Number 2 (September 1966) The tS andard of Care in Malpractice Cases Irvin Sherman Follow this and additional works at: http://digitalcommons.osgoode.yorku.ca/ohlj Article Citation Information Sherman, Irvin. "The tS andard of Care in Malpractice Cases." Osgoode Hall Law Journal 4.2 (1966) : 222-242. http://digitalcommons.osgoode.yorku.ca/ohlj/vol4/iss2/4 This Article is brought to you for free and open access by the Journals at Osgoode Digital Commons. It has been accepted for inclusion in Osgoode Hall Law Journal by an authorized editor of Osgoode Digital Commons. THE STANDARD OF CARE IN MALPRACTICE CASES IRVIN SHERMAN Medical malpractice has been a controversial issue both in the press and in medical and legal circles in recent years. As a result, the public in general and the medical profession in particular have become increasingly aware of the professional conduct of doctors. In Califor- nia, "malpractice actions have become so prevalent that on the average one out of every four doctors is sued at some time for malpractice".1 The situation is not quite as serious in Canada. In 1965, the Canadian Medical Protective Association which represents 78% (15,500 out of 22,000) of Canadian doctors handled just 27 cases in- volving malpractice.2 It has been stated that, "the practising physician or surgeon is an easy target for the blackmailer. The disgruntled or unscrupulous patient can inevitably destroy the reputation of the most eminent physician or surgeon by an ill-founded action for malpractice." 3 The adverse publicity atributable to a medical negligence case, regardless how unfounded the action may be, can only have a detrimental effect upon the doctor's career, thus weakening the vital role he can play in contributing to the needs of society. -

Of Rescue and Report: Should Tort Law Impose a Duty to Help Endangered Persons Or Abused Children? Marc A
Santa Clara Law Review Volume 40 | Number 4 Article 3 1-1-2000 Of Rescue and Report: Should Tort Law Impose a Duty to Help Endangered Persons or Abused Children? Marc A. Franklin Matthew loP eger Follow this and additional works at: http://digitalcommons.law.scu.edu/lawreview Part of the Law Commons Recommended Citation Marc A. Franklin and Matthew Ploeger, Symposium, Of Rescue and Report: Should Tort Law Impose a Duty to Help Endangered Persons or Abused Children?, 40 Santa Clara L. Rev. 991 (2000). Available at: http://digitalcommons.law.scu.edu/lawreview/vol40/iss4/3 This Symposium is brought to you for free and open access by the Journals at Santa Clara Law Digital Commons. It has been accepted for inclusion in Santa Clara Law Review by an authorized administrator of Santa Clara Law Digital Commons. For more information, please contact [email protected]. OF RESCUE AND REPORT: SHOULD TORT LAW IMPOSE A DUTY TO HELP ENDANGERED PERSONS OR ABUSED CHILDREN? Marc A. Franklin* & Matthew Ploeger** I. INTRODUCTION This essay explores whether a civil duty to rescue' should be imposed on a person who has the apparent ability to save another person or to prevent that person from entering a po- sition of peril.2 It also examines the related question of * Frederick I. Richman Professor, Stanford Law School. LL.B., Cornell Law School; A.B., Cornell University. A version of this essay was presented at the Santa Clara Law Review Symposium, Law, Ethics, and the Good Samari- tan, held at Santa Clara University School of Law on March 24, 2000. -

Libel As Malpractice: News Media Ethics and the Standard of Care
Fordham Law Review Volume 53 Issue 3 Article 3 1984 Libel as Malpractice: News Media Ethics and the Standard of Care Todd F. Simon Follow this and additional works at: https://ir.lawnet.fordham.edu/flr Part of the Law Commons Recommended Citation Todd F. Simon, Libel as Malpractice: News Media Ethics and the Standard of Care, 53 Fordham L. Rev. 449 (1984). Available at: https://ir.lawnet.fordham.edu/flr/vol53/iss3/3 This Article is brought to you for free and open access by FLASH: The Fordham Law Archive of Scholarship and History. It has been accepted for inclusion in Fordham Law Review by an authorized editor of FLASH: The Fordham Law Archive of Scholarship and History. For more information, please contact [email protected]. LIBEL AS MALPRACTICE: NEWS MEDIA ETHICS AND THE STANDARD OF CARE TODD F. SIMON* INTRODUCTION D OCTORS, lawyers, and journalists share a strong common bond: They live in fear of being haled into court where the trier of fact will pass judgment on how they have performed their duties. When the doc- tor or lawyer is sued by a patient or client, it is a malpractice case.I The standard by which liability is determined is whether the doctor or lawyer acted with the knowledge, skill and care ordinarily possessed and em- ployed by members of the profession in good standing.' Accordingly, if * Assistant Professor and Director, Journalism/Law Institute, Michigan State Uni- versity School of Journalism; Member, Nebraska Bar. 1. W. Keeton, D. Dobbs, R. Keeton & D. Owen, Prosser and Keeton on Torts, § 32, at 185-86 (5th ed. -

Imposed in Intentional Torts Suits Defendant Are at Fault
Using Comparative Fault to Replace the All-or-Nothing Lottery Imposed in Intentional Torts Suits in Which Both Plaintiff and Defendant Are at Fault Gail D. Hollister* I. INTRODUCTION .......................................... 122 II. REASONS FOR USING COMPARATIVE FAULT IN INTENTIONAL TORT CASES ............................................ 127 III. JUSTIFICATIONS OFFERED TO SUPPORT THE BLANKET PROHI- BITION ON THE USE OF COMPARATIVE FAULT IN INTEN- TIONAL TORT CASES ..................................... 132 A. Plaintiff's Fault Must Be Ignored to Circumvent the Harsh Results Imposed by Contributory Negli- gence ......................................... 132 B. Comparative Negligence Statutes Prohibit the Use of Comparative Fault in Intentional Tort Cases.. 134 C. Intent and Negligence Are Different in Kind and Thus Cannot Be Compared ..................... 135 1. Do Negligence and Intent Differ in Kind? .. 136 2. Do Differences in Kind Mandate Different R esults? .... 141 D. Plaintiff Is Entitled to Full Compensation....... 143 E. Plaintiff Has No Duty to Act Reasonably to Avoid H arm ......................................... 143 F. Plaintiff's Fault Cannot Be a Proximate Cause of H er Injury .................................... 144 G. The Need to Punish Defendant Precludes the Use of Comparative Fault .......................... 145 * Associate Professor of Law, Fordham University. B.S., University of Wisconsin, 1967; J.D., Fordham University School of Law, 1970. The author would like to thank Professors Helen Hadjiyannakis Bender, Robert M. Byrn, and Ludwik A. Teclaff for their helpful comments on earlier drafts. VANDERBILT LAW REVIEW [Vol. 46:121 H. The Need to Deter Substandard Conduct Makes Comparative Fault Undesirable................. 146 L Victim Compensation Militates Against the Use of Comparative Fault ............................ 149 IV. WHEN COMPARATIVE FAULT SHOULD BE USED IN INTEN- TIONAL TORT CASES ................................ -
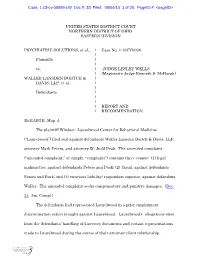
Case: 1:13-Cv-00098-LW Doc #: 33 Filed: 06/04/14 1 of 26. Pageid
Case: 1:13-cv-00098-LW Doc #: 33 Filed: 06/04/14 1 of 26. PageID #: <pageID> UNITED STATES DISTRICT COURT NORTHERN DISTRICT OF OHIO EASTERN DIVISION PSYCHIATRIC SOLUTIONS, et al., ) Case No. 1:13CV0098 ) Plaintiffs, ) ) vs. ) JUDGE LESLEY WELLS ) (Magistrate Judge Kenneth S. McHargh) WALLER LANSDEN DORTCH & ) DAVIS, LLP, et al., ) ) Defendants ) ) ) ) REPORT AND ) RECOMMENDATION McHARGH, Mag. J. The plaintiff Windsor- Laurelwood Center for Behavioral Medicine (“Laurelwood”) filed suit against defendants Waller Lansden Dortch & Davis, LLP, attorney Mark Peters, and attorney W. Judd Peak. The amended complaint (“amended complaint,” or simply, “complaint”) contains three counts: (1) legal malpractice, against defendants Peters and Peak; (2) fraud, against defendants Peters and Peak; and (3) vicarious liability/ respondeat superior, against defendant Waller. The amended complaint seeks compensatory and punitive damages. (Doc. 2 5 , Am. Compl.) The defendants had represented Laurelwood in a prior employment discrimination action brought against Laurelwood. Laurelwood’s allegations stem from the defendants’ handling of discovery documents and certain representations made to Laurelwood during the course of their attorney-client relationship. Case: 1:13-cv-00098-LW Doc #: 33 Filed: 06/04/14 2 of 26. PageID #: <pageID> The defendants have filed a motion to dismiss the fraud count, and the request for punitive damages. (Doc. 27, and exhibits, doc. 28.) The plaintiffs have filed a memorandum in opposition. (Doc. 29.) The defendants have filed a reply (doc. 30), with supplemental authority (doc. 31). The plaintiffs have weighed in on the supplemental authority. (Doc. 32.) I. MOTION TO DISMISS FOR FAILURE TO STATE A CLAIM Until fairly recently, the standard for a motion to dismiss for failure to state a claim upon which relief can be granted was that the motion establish, beyond a reasonable doubt, that “the plaintiff can prove no set of facts in support of his claim which would entitle him to relief.” Conley v. -

The Prima-Facie Case for Negligence (NB!: This Is the Basic Framework; You Will Need to Populate It with More Rules)
The Prima-Facie Case for Negligence (NB!: This is the basic framework; you will need to populate it with more rules) Plaintiff bears the burden of proof on the following elements of the prima-facie case. I. Duty (DUTY + STD): The issues of whether a [1] duty exists and, if so, what the [2] applicable standard or duty of care is, are generally legal determinations for the judge only:1 [1]. Does ∂ owe a legal duty to π; this is a binary issue, “yes or no.” [a]. Assume yes, unless a special no-duty rule says otherwise. [2]. If “yes,” then determine what standard of care the law prescribes: [a]. The default standard at common law is to act as a reasonable and prudent person would under the same or similar circumstances; [i]. Sometimes this standard is directly modified by the common law or by statute—e.g. physical infirmity, children, trespassers, medical malpractice. [b]. Sometimes a statute or regulation indirectly prescribes the standard, i.e., negligence per se. II. Breach: Breach issues are for the fact finder (the jury, in a jury trial), unless there is no triable issue of fact [e.g., MSJ or JMOL]. Once the judge decides on the proper “standard of care” for the case, see supra § I.[2], the fact finder must determine whether the ∂ has failed to conform to the applicable standard. Stated another way, the fact finder must decide whether the ∂ has breached his or her “duty of care” or was “negligent.” For example: [1]. ∂ has breached the applicable common-law standard; or [a]. -

United States Court of Appeals for the Eighth Circuit ______
United States Court of Appeals For the Eighth Circuit ___________________________ No. 17-2274 ___________________________ Stuart Wright lllllllllllllllllllllPlaintiff - Appellant v. United States of America lllllllllllllllllllllDefendant - Appellee John Clark; Walter R. Bradley, in his official capacity as the United States Marshal for the District of Kansas; Sean Franklin, in his official capacity as a Deputy United States Marshal and in his individual capacity; Deputy United States Marshals 1 - 10, in their official and individual capacities (names unknown at this time); Stacia A. Hylton, in her official capacity; Christopher Wallace, in his official capacity as a Deputy United States Marshal and in his individual capacity lllllllllllllllllllllDefendants ____________ Appeal from United States District Court for the Western District of Missouri - Kansas City ____________ Submitted: March 16, 2018 Filed: June 13, 2018 ____________ Before WOLLMAN, SHEPHERD, and ERICKSON, Circuit Judges. ____________ Appellate Case: 17-2274 Page: 1 Date Filed: 06/13/2018 Entry ID: 4672148 SHEPHERD, Circuit Judge. In the third iteration of this unfortunate case of mistaken identity, Plaintiff Stuart Wright (“Wright”) appeals the district court’s1 grant of summary judgment to the United States and the Deputy U.S. Marshals in their individual and official capacities on Wright’s claims under the Federal Tort Claims Act (the “FTCA”). Wright argues that the district court erred when it found there was no genuine dispute of material fact and that, as a matter of law, the Marshals were not liable to him under the FTCA for false arrest, false imprisonment, abuse of process, and assault and battery. We disagree and affirm the district court’s grant of summary judgment. -

United States District Court for the District
Case 2:16-cv-00081-CWD Document 96 Filed 07/14/17 Page 1 of 9 UNITED STATES DISTRICT COURT FOR THE DISTRICT OF IDAHO JUSTIN T. GARRIOTT and SUSAN GARRIOTT, husband and wife; Case No. 2:16-cv-00081-CWD JASPYN GARRIOTT, JUSTIN GARRIOTT JR., JMG1, a minor, and MEMORANDUM DECISION AND JMG2, a minor, ORDER (Dkt. 85) Plaintiffs, v. WESTERN MEDICAL ASSOCIATES, PLLC, an Idaho corporation; PAUL PASCHALL, MD; ERIC CHUN, MD, Defendants. INTRODUCTION Before the Court is Defendants’ first partial motion for summary judgment (Dkt. 85), filed on March 31, 2017. The parties have filed their responsive briefing and the matter is ripe for the Court's consideration. This matter involves a medical malpractice claim brought against two emergency room physicians. His four children each bring a claim for loss of consortium based upon the injury to their father, Justin Garriott Sr. MEMORANDUM DECISION AND ORDER - 1 Case 2:16-cv-00081-CWD Document 96 Filed 07/14/17 Page 2 of 9 The Court conducted a hearing regarding the motion on July 11, 2017, at which the parties appeared and presented their arguments. After carefully considering the parties’ written memoranda, relevant case law, and the parties’ arguments, the Court will grant Defendants’ motion for partial summary judgment. FACTS According to the complaint, Plaintiffs Justin T. Garriott and Susan Garriott are husband and wife, and they have four children. They reside together in Spokane County, Washington. On March 25, 2015, Justin Garriott began feeling ill, and he visited an urgent care center. On March 27, 2015, Mr. -

Fraud and Misrepresentation Claims Against Lawyers
16 NEV. L.J. 57, RICHMOND - FINAL.DOCX 1/15/16 1:34 PM FRAUD AND MISREPRESENTATION CLAIMS AGAINST LAWYERS Douglas R. Richmond* TABLE OF CONTENTS INTRODUCTION ................................................................................................. 57 I. UNDERSTANDING FRAUD AND MISREPRESENTATION ........................... 63 A. Common Law Fraud ...................................................................... 63 B. Fraudulent Concealment ............................................................... 70 C. Constructive Fraud ....................................................................... 75 D. Negligent Misrepresentation ......................................................... 77 E. The Role of Rules of Professional Conduct ................................... 82 II. ILLUSTRATIVE CASES ............................................................................ 84 A. Settlement Negotiations in Litigation ............................................ 84 B. Litigators’ Allegedly Fraudulent Statements Outside of Settlement Negotiations ................................................................. 88 C. Third Party Reliance on a Lawyer’s Statements in a Real Estate Transaction ......................................................................... 93 D. The Dean Foods Opinion Controversy ......................................... 99 CONCLUSION .................................................................................................. 103 INTRODUCTION Most lawyers are competent, diligent, and honest. No lawyer