Scaling of Tele-Health for Hypertension Across Three Healthcare Clusters
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

So, This Is What It Feels Like to Be Old!
WWW.SINGHEALTH.COM.SG • WWW.SGH.COM.SG MAR/APR 2020 MCI (P) 056/10/2019 THE FLAGSHIP IN FOCUS PUBLICATION OF THE SINGHEALTH DUKE-NUS ACADEMIC MEDICAL CENTRE Page 7 Healthy cells left alone in prostate cancer trial PEOPLE Page 12 A night in the life of So, this is a sleep technologist what it HEALTHWATCH feels like to be old! Not a robot but old-age simulated by an “age suit”. It highlights how the loss of muscle strength makes the elderly more prone to falls Page 16 READ MORE ON PAGE 3 The real cause of back and neck pain 01 SingHealth Issue 58 Cover V1.indd 7 13/2/20 5:58 PM SGH200 PAGE 02 The history of Singapore General Hospital (SGH) is the history Counting of medicine in Singapore. The first general hospital for British troops was established in Singapore in 1819, but it was only in 1821 that it began serving the general populace — marking the down to PUBLISHERS true beginnings of SGH. As the countdown to SGH’s bicentennial begins, Singapore Health will present snapshots showing changes in 2021 medicine and its various disciplines in the past 200 years. Photo: SGH Photo: CO-PUBLISHERS The roots of orthopaedic Vernon Wong Photo: surgery ® Staffed by general CONTENT ADVISOR surgeons in the early Group Chief Communications Officer, SingHealth days, the discipline is now Audrey Lau highly specialised, with EDITORIAL TEAM surgeons operating in Lim Mui Khi, Ann Peters, Tina Nambiar, Lydia Ng seven areas, such as spine, sports medicine, and Read Singapore Health online at musculoskeletal tumours. -

Singhealth Duke-NUS Academic Medical Centre
SingHealth Group Overall Key Figures & Statistics Outram Road, Singapore 169608 11 Hospital Drive, Singapore 169610 11 Third Hospital Drive, Singapore 168751 MANPOWER Tel: 6222 3332 www.sgh.com.sg Tel: 6436 8000 www.nccs.com.sg Tel: 6227 7255 www.snec.com.sg Medical Dental Nursing Allied Others TOTAL Medical Dental Nursing Allied Others TOTAL Medical Dental Nursing Allied Others TOTAL Medical Dental Nursing Allied Others Health Health Health Health TOTAL 2,783 171 8,186 4,361 7,197 22,698 1,206 0 4,329 1,893 2,543 9,971 191 0 168 392 357 1,108 125 0 263 134 309 831 Size Workload per annum Workload per annum KEY FIGURES 1,785 Beds (as at end Mar) 9,588 Day Surgeries 42,220 Day Surgeries 151,933 Specialist Outpatient Clinic Attendances 341,815 Specialist Outpatient Clinic Attendances 2017 SingHealth - Overall Workload per annum 80,817 Inpatients Size 45,206 Day Surgeries 3,165 Beds (as at end Mar) 47,022 Inpatient Surgeries 5 Second Hospital Avenue, Singapore 168938 167 Jalan Bukit Merah, Tower 5, #15-10, Workload per annum 724,480 Specialist Outpatient Clinic Attendances Singapore 150167 Tel: 6324 8802 www.ndcs.com.sg 167,599 Inpatients 128,660 Accident & Emergency Attendances Tel: 6236 4800 polyclinic.singhealth.com.sg 122,541 Day Surgeries 73,699 Inpatient Surgeries Medical Dental Nursing Allied Others TOTAL Medical Dental Nursing Allied Others TOTAL 1,963,945 Specialist Outpatient Clinic Attendances Health Health 316,708 Accident & Emergency Attendances 100 Bukit Timah Road, Singapore 229899 0 140 14 66 250 470 195 17 295 180 483 1,170 -

Mutual Recognition of Ethics Review
Mutual Recognition of Research Ethics Review between SingHealth CIRB and NHG DSRB Frequently Asked Questions General 1. What types of cross-cluster studies are eligible for single IRB reviews? All new research applications involving both SingHealth and NHG* sites are eligible to benefit from the CIRB-DSRB mutual recognition arrangement and have their studies reviewed by only 1 IRB. Note: Research studies involving only SingHealth or NHG sites will continue to be reviewed by the respective cluster IRBs (i.e. SingHealth CIRB or NHG DSRB). *including partner institutions under NHG DSRB purview (only for those who has appointed SingHealth CIRB as the reviewing IRB). Under the Oversight of SingHealth CIRB Under the Oversight of NHG DSRB SingHealth Institutions: National Healthcare Group (NHG) Institutions: Changi General Hospital (CGH) Institute of Mental Health (IMH) KK Women’s and Children’s Hospital (KKH) Tan Tock Seng Hospital (TTSH) National Cancer Centre (NCC) National Skin Centre (NSC) National Dental Centre (NDC) NHG Polyclinics (NHGP) National Heart Centre (NHC) NHG Pharmacy National Neuroscience Institute (NNI) NHG HQ Sengkang General Hospital (SKH) NHG Diagnostics Singapore Eye Research Institute (SERI) NHG College Singapore General Hospital (SGH) NHG Eye Institute Singapore Health Services (SingHealth) Khoo Teck Puat Hospital (KTPH) SingHealth Community Hospitals Yishun Community Hospital (YCH) Bright Vision Hospital (BVH) Admiralty Medical Centre (AdMC) Outram Community Hospital (OCH) Geriatric Education & Research Institute -
GIRO Application Form.Pdf
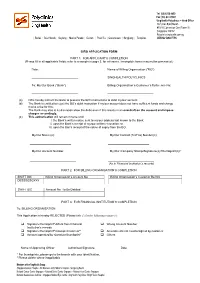
Tel: (65) 6236 4800 Fax: (65) 6274 9901 SingHealth Polyclinics – Head Office 167 Jalan Bukit Merah #15-10 Connection One (Tower 5) Singapore 150167 Polyclinic.singhealth.com.sg | Bedok | Bukit Merah | Geylang | Marine Parade | Outram | Pasir Ris | Queenstown | Sengkang | Tampines UEN No 52928775K GIRO APPLICATION FORM PART 1: FOR APPLICANT’S COMPLETION (Please fill in all applicable fields; refer to a sample in page 3, for reference. Incomplete forms may not be processed.) Date: Name of Billing Organisation (“BO”) ____________________________ SINGHEALTH POLYCLINICS To: My/Our Bank (“Bank”) Billing Organisation’s Customer’s Reference No: _____________________________ _____________________________ (a) I/We hereby instruct the Bank to process the BO’s instructions to debit my/our account. (b) The Bank is entitled to reject the BO’s debit instruction if my/our account does not have sufficient funds and charge me/us a fee for this. The Bank may also at its discretion allow the debit even if this results in an overdraft on the account and impose charges accordingly. (c) This authorisation will remain in force until i. the Bank’s written notice sent to my/our address last known to the Bank; ii. upon the Bank’s receipt of my/our written revocation; or iii. upon the Ban’s receipt of the notice of expiry from the BO. My/Our Name (s): My/Our Contact (Tel/Fax) Number(s): _____________________________ _____________________________ My/Our Account Number: My/Our Company Stamp/Signature(s)/Thumbprint(s)*: _____________________________ _____________________________ (As in Financial Institution’s records) PART 2: FOR BILLING ORGANISATION’S COMPLETION SWIFT BIC Billing Organisation’s Account No Billing Organisation’s Customer Ref No DBSSSGSGXXX SWIFT BIC Account No. -

List of GP Clinics Under Primary Care Network (PCN) Scheme
List of GP Clinics Under Primary Care Network (PCN) Scheme ASSURANCE PCN [ASSURANCE PCN PTE. LTD.] S/N PCN Clinic Name Clinic HCI Address Operating Hours (Please call the clinic to verify operating hours before visiting) Contact No Monday - Friday: 8.30am - 1.00pm, 2.00pm - 5.00pm, 6.00pm - 9.00pm 1 ASSURANCE PCN ACUMED MEDICAL GROUP [BEDOK CLINIC] 9405242 BLK 214 BEDOK NORTH STREET 1 #01-165 SINGAPORE 460214 Saturday: 8.30am - 1.00pm 6443 8077 Sunday, Public Holidays: 9.00am - 12.00noon Monday - Friday: 9.00am - 1.00pm, 2.00pm - 7.00pm 2 ASSURANCE PCN ACUMED MEDICAL GROUP [JOO KOON CLINIC] 15M0211 1 JOO KOON CIRCLE #01-23 FAIRPRICE HUB SINGAPORE 629117 Saturday: 9.00am - 1.00pm 6861 5755 Sunday, Public Holidays: Closed Monday - Friday: 8.30am - 5.00pm 1 JURONG WEST CENTRAL 2 #B1A-19E JURONG POINT SHOPPING CENTRE SINGAPORE 3 ASSURANCE PCN ACUMED MEDICAL GROUP [JURONG WEST CLINIC-JURONG POINT] 9405234 Saturday: 8.30am - 1.00pm 6792 3822 648886 Sunday, Public Holidays: Closed 4 ASSURANCE PCN ACUMED MEDICAL GROUP [RAFFLES PLACE CLINIC-INCOME AT RAFFLES] 9405222 16 COLLYER QUAY #02-03 INCOME AT RAFFLES SINGAPORE 049318 Monday - Friday: 8.30am - 12.30pm, 1.00pm - 5.30pm 6532 7766 Monday - Friday: 9.00am - 1.00pm, 2.00pm - 4.00pm, 6.00pm - 8.30pm 5 ASSURANCE PCN ACUMED MEDICAL GROUP [SENGKANG CLINIC] 17M0142 BLK 215C COMPASSVALE DRIVE #01-02 SINGAPORE 543215 6385 0113 Saturday - Sunday, Public Holidays: 9.30am - 12.30pm, 6.00pm - 8.30pm Monday - Friday: 8.30am - 9.00pm 6 ASSURANCE PCN ACUMED MEDICAL GROUP [TAMAN JURONG CLINIC] 9405239 BLK 64 -

FY2019/2020 Singhealth Fund Annual Report
Making a difference Annual Report SINGHEALTH FUND FY c/o 167 Jalan Bukit Merah, Connection One, Tower 5 #06-11, Singapore 150167 2019 www.singhealth.com.sg/giving | (65) 6377 7605 | [email protected] UEN 201624016E Contents Research 2 Education 8 Patient Care 12 Other Programmes 16 Annual Report for Year 21 Ended 31 March 2020 SingHealth Fund (SHF) champions research, education and patient care causes to support SingHealth’s vision of defining tomorrow’s medicine and to unleash the potential of Medicine to enable better health for future generations. Your gifts to SHF make a real and tangible difference to the lives of patients and their loved ones, empower healthcare professionals to accelerate the search for cures and sharpen their capabilities to provide even better care. Vision Defining Tomorrow’s Medicine Mission Care to Heal, Educate to Empower and Innovate to Advance Value Compassion, Integrity and Collaboration Thank you for believing in our cause, our work and for supporting our pursuit to define tomorrow’s medicine. Page 1 Philanthropy has been important in kick-starting many of our research projects to provide patients with cutting-edge therapies. Donations received in the early years of stem cell transplant research were important in making these treatments available for our patients. Prof William Hwang Medical Director National Cancer Centre Singapore SingHealth Fund Annual Report FY 2019 Research Giving to research enables our clinician scientists to translate groundbreaking ideas into meaningful healthcare solutions that directly benefit our patients. In FY2019, SHF supported: research programmes 72 and projects Advancing research in blood cancers and stem cells The global number of blood cancer cases is hematopoietic stem cell transplant products expected to grow over the next few decades, that can result in better patient outcomes reaching close to two million by 2040. -

International Journal of Cerebrovascular Disease and Stroke Christopher SYH, Et Al
International Journal of Cerebrovascular Disease and Stroke Christopher SYH, et al. Int J Cerebrovasc Dis Stroke 3: 125. Opinion Article DOI: 10.29011/2688-8734.000025 Challenges in Adapting Existing Hyperacute Stroke Protocols by a Tertiary Neuroscience Centre for Patients with COVID – 19 in Singapore Seet Ying Hao Christopher1*, Tham Huilian Carol1, Wong Yu-Lin2 1Department of Neurology, National Neuroscience Institute, Singhealth, Singapore 2Department of Anaesthesia, Tan Tock Seng Hospital, National Healthcare Group, Singapore *Corresponding author: Seet Ying Hao Christopher, Department of Neurology, National Neuroscience Institute, Singhealth, 11 Jalan Tan Tock Seng, Singapore Citation: Christopher SYH, Carol TH, Yu-Lin W (2020) Challenges in Adapting Existing Hyperacute Stroke Protocols by a Ter- tiary Neuroscience Centre for Patients with COVID – 19 in Singapore. Int J Cerebrovasc Dis Stroke 3: 125. DOI: 10.29011/2688- 8734.000025 Received Date: 27 March, 2020; Accepted Date: 02 April, 2020; Published Date: 06 April, 2020 Abstract COVID-19 patients can also present with hyperacute stroke and current stroke workflows are insufficiently equipped to treat such patients. We have created a harmonized stroke protocol to safely continue hyperacute stroke therapy for such patients whilst minimizing the risk of exposure and cross contamination. Keywords: Stroke; Hyperacute protocol; COVID-19; Personal designated tertiary hyperacute stroke centre that manages the Protective Equipment (PPE) largest number of hyperacute stroke cases (1500 – 2000 cases/year) in Singapore. NNI also has direct access to the National Centre Introduction for Infectious Diseases (NCID) which is designated the national centre for suspected and confirmed COVID-19 patients. To date Coronavirus disease 2019 (COVID-19) has been a significant NCID has also managed 181 out of 266 confirmed COVID-19 regional and global health burden since it was first reported patients in Singapore as of 15 March 2020. -

Brain Tumours Brochure English FA Print
Side Eects of Treatment Contact Information Scan the QR code to learn Neurosurgery Department more about other NNI@TTSH Side eects can range from fatigue, headaches and scalp Neuroscience conditions irritation for radiation therapy. Chemotherapy patients Tan Tock Seng Hospital, NNI Block, Neuroscience Clinic may experience nausea and hair loss, while those 11 Jalan Tan Tock Seng, Singapore 308433 undergoing radiosurgery may have headaches and Main Tel: (65) 6357 7153 nausea. Appt. Tel: (65) 6330 6363 Email: [email protected] Surgery for a tumour that is close to a nerve, or located in Website: www.nni.com.sg a critical or sensitive area of the brain may aect body functions such as sight, speech and movement. Scan QR Rehabilitation and Support for Brain Tumour code for NNI@SGH directions Singapore General Hospital, Block 3, Clinic L Recovery depends on the brain’s ability to heal from The National Neuroscience Institute operates out of Outram Road, Singapore 169608 damage caused by the tumour. Therapists such as two main campuses (TTSH, SGH) and Main Tel: (65) 6222 3322 physiotherapist, occupational therapist and speech four partner hospitals (CGH, KKH, KTPH, SKH). therapist to support rehabilitation. If there is persistent Appt. Tel: (65) 6321 4377 disability, the patient may be sent to a community Email: [email protected] NNI @ KTPH hospital for further neuro-rehabilitation. Website: www.nni.com.sg During rehabilitation, the patient and family should NNI @ SKH maintain a positive attitude, set realistic goals and work steadily to accomplish each goal. NNI@CGH NNI@KKH NNI @ TTSH NNI @ CGH Changi General Hospital KK Women’s and NNI @ KKH Brain Tumour Society Singapore 2 Simei Street 3 Children’s Hospital Singapore 529889 100 Bukit Timah Road NNI @ SGH The Brain Tumour Society Singapore (BTSS) is a Appt. -

Key Figures & Statistics
SINGHEALTH GROUP OVERALL Outram Road, Singapore 169608 100 Bukit Timah Road, Singapore 229899 11 Jalan Tan Tock Seng, Singapore 308433 KEY FIGURES & STATISTICS Tel: 6222 3332 www.sgh.com.sg Tel: 6225 5554 www.kkh.com.sg Tel: 6357 7153 www.nni.com.sg Medical Dental Nursing AHPs Others Total Medical Dental Nursing AHPs Others Total Medical Dental Nursing AHPs Others Total MANPOWER 1,147 0 3,708 1,789 2,421 9,066 722 13 1,909 896 1,261 4,800 101 0 41 151 132 424 Medical Dental Nursing AHPs Others Total 2019 2019 2019 3,682 173 10,515 5,623 8,954 28,947 Size Size Workload per annum Beds (As at end March) 1,723 Beds (As at end March) 848 Specialist Outpatient Clinic Attendances 51,395 KEY FIGURES Workload per annum Workload per annum Year ended 31 Mar Bed Occupancy Rate 84.4% Bed Occupancy Rate 79.8% 11 Third Hospital Drive, Singapore 169751 Inpatients 80,423 Inpatients 75,505 2019 Tel: 6227 7255 www.snec.com.sg ACUTE CARE AND POLYCLINICS Total Patient Days 486,015 Total Patient Days 215,468 Average Length of Stay (days) 6.0 Average Length of Stay (days) 2.9 Size Medical Dental Nursing AHPs Others Total Day Surgeries 51,928 Day Surgeries 11,242 Beds (As at end March) 4,345 115 0 305 160 340 920 Inpatient Surgeries 47,784 Inpatient Surgeries 19,581 Workload per annum Specialist Outpatient Clinic Attendances 749,507 Specialist Outpatient Clinic Attendances 552,504 2019 Bed Occupancy Rate 82.5% Accident & Emergency Attendances 124,691 Accident & Emergency Attendances 154,521 Workload per annum Inpatients 236,442 Dental Attendances 5,894 Day Surgeries -

Annual Report 2015
ur interpretation of “An Evolving Primary Care Ecosystem” in Singapore is depicted through the use of the tangram. Arranged O into the shape of a butterfly, it is used to signify the transformation and place emphasis on metamorphosis of the primary care ecosystem. The tangram also represents the ecosystem where every piece of the structure supports each other and come together in forming the desired goal. This tangram consists of seven pieces which symbolises the seven chapters within the report. Each piece is coloured according to the dividers to create the sense of “continuity of transformation” throughout the book. OUR VISION, MISSION AND CONTENTS VALUES OUR VISioN OUR VALUES To be the leading health-promoting Integrity institution that helps advance We are committed to the highest Family Medicine and transform standards of ethical conduct. 06 08 10 12 Group CEO’s CEO’s Message NHGP Senior About NHGP primary healthcare in Singapore. Message Management Compassion Our paramount concern is OUR MISSioN the welfare and well-being of our fellow human beings. We We will improve health and reduce sympathise with those struck illness through patient-centred with illness and suffering quality primary healthcare and will do our best to help that is accessible, seamless, alleviate their condition. comprehensive, appropriate and 16 22 30 42 cost-effective in an environment Professionalism Chapter 1: Chapter 2: Chapter 3: Chapter 4: of continuous learning and We are committed to being Beyond Beyond Beyond Beyond relevant research. the best in what we do and NHGP 15 Boundaries Satisfaction Potential achieving the best possible outcome for our patients. -

Supplementary Guide on Open-Access Spirometry in Singapore
Updated: 23 Nov 2019 SUPPLEMENTARY GUIDE www.ace-hta.gov.sg Open-access spirometry in Singapore Patients from primary care or other specialists without onsite spirometry can be referred directly to the following pulmonary laboratories for spirometry. The doctor needs to provide a referral letter or memo, and the spirometry report will be sent to the referring doctor. Institution Location Contact details for booking appointments Changi General Hospital (CGH) 2 Simei Street 3 Tel: 6788 3003 Singapore 529889 Frontier Family Medicine Clinic 3151 Commonwealth Ave West Tel: 6778 8362 04-01 Grantral Mall@Clementi Email: [email protected] Singapore 129581 Jurong East Community Health 229 Jurong East St 21, 01-701 Tel: 6665 1290 Centre (JECHC) Singapore 600229 Fax: 6896 1832 Keat Hong Family Medicine Clinic 2 Choa Chu Kang Loop, 03-02 Tel: 6769 0750 Singapore 689687 Email: [email protected] KhooTeck Puat Hospital (KTPH) 90 Yishun Central Tel: 6602 3491 for appointments Pulmonary Function Laboratory Tower C, Level 5, Clinic C52 Email encrypted memo to: Singapore 768828 [email protected] National Healthcare Group •Ang Mo Kio Polyclinic Tel: 6496 6633 Polyclinics (NHGP) •Geylang Polyclinic Email: [email protected] •Hougang Polyclinic •Toa Payoh Polyclinic •Woodlands Polyclinic •Yishun Polyclinic National University Hospital 13b Medicine Clinic Tel: 6772 2244 (NUH) NUH Medical Centre, Level 13 5 Lower Kent Ridge Singapore 119074 National University Polyclinics •Bukit Batok Polyclinic Tel: 6496 6633 -

Reorganisation of Healthcare System Into Three Integrated Clusters to Better Meet Future Healthcare Needs
REORGANISATION OF HEALTHCARE SYSTEM INTO THREE INTEGRATED CLUSTERS TO BETTER MEET FUTURE HEALTHCARE NEEDS Primary care system integrated in each cluster, for more patient-centric care deeper into community The Ministry of Health (MOH) will reorganise the public healthcare system into three integrated clusters to better meet Singaporeans’ future healthcare needs. 2 The three integrated clusters formed will be as follows. The list of the institutions within each cluster can be found in Annex A. Central region – National Healthcare Group (NHG) and Alexandra Health System (AHS) will be merged. Eastern region –Singapore Health Services (SingHealth) and Eastern Health Alliance (EHA) will be merged. Western region – National University Health System (NUHS) and Jurong Health Services (JurongHealth) will be merged. 3 The polyclinics will also be reorganised, in line with the three new clusters. The National University Polyclinics group will be formed under NUHS, joining SingHealth Polyclinics and NHG Polyclinics as Singapore’s third polyclinic group. 4 The integrated clusters will each be headed by a Group Chief Executive Officer (CEO), namely Prof Philip Choo (Group CEO, NHG); Prof Ivy Ng (Group CEO, SingHealth); and Prof John Wong Eu Li (Group CEO, NUHS). Dr Lew Yii Jen (currently Senior Director, Clinical Services, NHG Polyclinics) will be the CEO for the new National University Polyclinics. 5 Our public healthcare system is currently organised into six regional health systems - Alexandra Health System, Eastern Health Alliance, Jurong Health Services, National Healthcare Group, National University Health System and Singapore Health Services. They operate a range of healthcare institutions, and build partnerships among healthcare providers in their respective region, including acute and community hospitals, primary care providers, nursing homes and other long term care providers.