Annual Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Study-Newcastle-Lonely-Planet.Pdf
Produced by Lonely Planet for Study NT NewcastleDO VIBRAne of Lonely Planet’s Top 10 Cities in Best in Travel 2011 N CREATIVE A LANET Y P ’S EL TO N P O 1 L 0 F TOP C O I T TOP E I E N S O 10 CITY I N 10 CITY ! 1 B 1 E 0 S 2 2011 T L I E N V T A R 2011 PLANE LY T’S NE T O O P L F 1 O 0 C E I N T I O E S ! 1 I 1 N 0 B 2 E L S E T V I A N R T LANET Y P ’S EL TO N P O 1 TOP L 0 F TOP C O I T 10 CITY E I E N S O 10 CITY I N ! 2011 1 B 1 E 0 LAN S P E 2 Y T 2011 T L L ’ I S E N E V T A R N T O O P L F 1 O 0 C E I N T I O E S ! 1 I 1 N 0 B 2 E L S E T V I A N R T E W RE HANI AKBAR st VER I » Age 22 from Saudi Arabia OL » From Saudi Arabia » Studying an International Foundation program What do you think of Newcastle? It’s so beautiful, not big not small, nice. It’s a good place for students who are studying, with a lot of nice people. -

Hunter Investment Prospectus 2016 the Hunter Region, Nsw Invest in Australia’S Largest Regional Economy
HUNTER INVESTMENT PROSPECTUS 2016 THE HUNTER REGION, NSW INVEST IN AUSTRALIA’S LARGEST REGIONAL ECONOMY Australia’s largest Regional economy - $38.5 billion Connected internationally - airport, seaport, national motorways,rail Skilled and flexible workforce Enviable lifestyle Contact: RDA Hunter Suite 3, 24 Beaumont Street, Hamilton NSW 2303 Phone: +61 2 4940 8355 Email: [email protected] Website: www.rdahunter.org.au AN INITIATIVE OF FEDERAL AND STATE GOVERNMENT WELCOMES CONTENTS Federal and State Government Welcomes 4 FEDERAL GOVERNMENT Australia’s future depends on the strength of our regions and their ability to Introducing the Hunter progress as centres of productivity and innovation, and as vibrant places to live. 7 History and strengths The Hunter Region has great natural endowments, and a community that has shown great skill and adaptability in overcoming challenges, and in reinventing and Economic Strength and Diversification diversifying its economy. RDA Hunter has made a great contribution to these efforts, and 12 the 2016 Hunter Investment Prospectus continues this fine work. The workforce, major industries and services The prospectus sets out a clear blueprint of the Hunter’s future direction as a place to invest, do business, and to live. Infrastructure and Development 42 Major projects, transport, port, airports, utilities, industrial areas and commercial develpoment I commend RDA Hunter for a further excellent contribution to the progress of its region. Education & Training 70 The Hon Warren Truss MP Covering the extensive services available in the Hunter Deputy Prime Minister and Minister for Infrastructure and Regional Development Innovation and Creativity 74 How the Hunter is growing it’s reputation as a centre of innovation and creativity Living in the Hunter 79 STATE GOVERNMENT Community and lifestyle in the Hunter The Hunter is the biggest contributor to the NSW economy outside of Sydney and a jewel in NSW’s rich Business Organisations regional crown. -
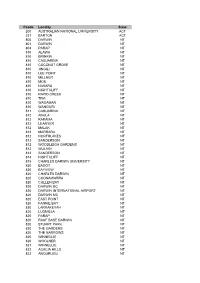
Pcode Locality State 200 AUSTRALIAN NATIONAL
Pcode Locality State 200 AUSTRALIAN NATIONAL UNIVERSITY ACT 221 BARTON ACT 800 DARWIN NT 801 DARWIN NT 804 PARAP NT 810 ALAWA NT 810 BRINKIN NT 810 CASUARINA NT 810 COCONUT GROVE NT 810 JINGILI NT 810 LEE POINT NT 810 MILLNER NT 810 MOIL NT 810 NAKARA NT 810 NIGHTCLIFF NT 810 RAPID CREEK NT 810 TIWI NT 810 WAGAMAN NT 810 WANGURI NT 811 CASUARINA NT 812 ANULA NT 812 KARAMA NT 812 LEANYER NT 812 MALAK NT 812 MARRARA NT 812 NORTHLAKES NT 812 SANDERSON NT 812 WOODLEIGH GARDENS NT 812 WULAGI NT 813 SANDERSON NT 814 NIGHTCLIFF NT 815 CHARLES DARWIN UNIVERSITY NT 820 BAGOT NT 820 BAYVIEW NT 820 CHARLES DARWIN NT 820 COONAWARRA NT 820 CULLEN BAY NT 820 DARWIN DC NT 820 DARWIN INTERNATIONAL AIRPORT NT 820 DARWIN MC NT 820 EAST POINT NT 820 FANNIE BAY NT 820 LARRAKEYAH NT 820 LUDMILLA NT 820 PARAP NT 820 RAAF BASE DARWIN NT 820 STUART PARK NT 820 THE GARDENS NT 820 THE NARROWS NT 820 WINNELLIE NT 820 WOOLNER NT 821 WINNELLIE NT 822 ACACIA HILLS NT 822 ANGURUGU NT 822 ANNIE RIVER NT 822 BATHURST ISLAND NT 822 BEES CREEK NT 822 BORDER STORE NT 822 COX PENINSULA NT 822 CROKER ISLAND NT 822 DALY RIVER NT 822 DARWIN MC NT 822 DELISSAVILLE NT 822 FLY CREEK NT 822 GALIWINKU NT 822 GOULBOURN ISLAND NT 822 GUNN POINT NT 822 HAYES CREEK NT 822 LAKE BENNETT NT 822 LAMBELLS LAGOON NT 822 LIVINGSTONE NT 822 MANINGRIDA NT 822 MCMINNS LAGOON NT 822 MIDDLE POINT NT 822 MILIKAPITI NT 822 MILINGIMBI NT 822 MILLWOOD NT 822 MINJILANG NT 822 NGUIU NT 822 OENPELLI NT 822 PALUMPA NT 822 POINT STEPHENS NT 822 PULARUMPI NT 822 RAMINGINING NT 822 SOUTHPORT NT 822 TORTILLA -

The University News, Vol. 6, No. 3, March 20, 1980
'f\.-~\r.,v-eo VOL 6 NO 3 20 MARCH 80 Newsletter for ( The University of Newcastle U /G PASS RATES a ""mber of ho"" per week that a REPRODU CTIVE M EDICIN E full-time student is advised to The Vice-Chancellor. Professor At its meeting on March 5, the spend on study. Members of staff . Don George, has announced the Senate considered the Report of will be advised to take reasonable appOintment of Dr. Jeffrey the Committee to Consider Under care to ensure that attendance at Robfnson of Oxford UniYersity to graduate Pass Rates. classes, set work and required the Foundation Chair of Reproduct- Senate recognised the com reading for each subject can be iye Medicine in the. Faculty of plexity of the problems. which accomplished within the appropriate Medicine in the University. are by no means confined to this fraction of the total number of Dr. Robinson. who 1s 37 years University alone. Senate was an hours recommended. of age. was educated at Queen's xious to treat the matter serious The Senate also supported the University. Belfast, where he ly. whilst keeping the issues in appointment of external examiners graduated in 1967 as· B.Sc. (Anat- proportion. It considered that for all Departments. An examin-- omy) with 1st Class Honours and positive action could be taken on ation result "terminating pass" in 1967 as M.B., B.A .• B.A.O. In 'several levels. In principle, was approved for introduction at 1970 he took up a Nufffeld Fellow- the Senate believes that the pro the discretion of Faculty and ship in the Nuffield Institute blems can only be solved at Departmental Boards. -

The Shoreline, Visiting Places That Once Formed a Crucial Part of Newcastle’S Working Harbour and Maritime Culture
FITZROY STREET FERN STREET YOUNG STREET COWPER STREET COAL ST WILSON STREET DENISON STREET MAITLAND ROAD HUDSON STREET ALBERT STREET DONALD STREET GREENWAY STREET E S U Heavy O H T WALKING Trail 3hrs / 3.2km H CLEARY STREET IG CHURCH STREET L & S Y B B O N LINDSAY STREET O THROSBY STREET Newcastle/Stockton Newcastle Harbour T Ferry RAILWAY STREET SAMDON STREET LINDUS STREET JAMES STREET CAMERON STREET THE 7 Destiny 6 BREAKWALL TUDOR STREET BISHOPGATE STREET Nobbys Beach WHARF ROAD 5 DIXON STREET ELCHO STREET SHORELINE BRIDGE STREET 1 4 MILTON STREET WILLIAM STREET 2 8 MURRAY STREET DENISON STREET EXPLORE NEWCASTLE’SHONEYSUCKLE MARITIME DRIVE AND WORKSHOP PARRY STREET WAY STEEL STREET CENTENARY RD WHARF ROAD ARGYLE ST SURF CULTURE THROUGH A SELF-GUIDED NOBBYS ROAD SCOTT STREET FORT DR MEREWETHER ST SHEPERDS PL WOOD ST 3 BOND ST STEVENSON PLACE VEDA STREET WALKING TOUR OF THE CITY. HUNTER STREET HUNTER STREET ALFRED ST HUNTER STREET BEACH ST SKELTON ST AUCKLAND STREET SHORTLAND ESP CHAUCER STREET KING STREET KING STREET KING STREET STEEL ST EVERTON STREET WARRAH STREET BROWN STREET PARNELL PL DARBY STREET TELFORD STREET PERKINS STREET AVE KING STREET MURRAY HEBBURN STREET OCEAN ST SILSOE STREET UNION STREET CHURCH STREET ZAARA ST DUMARESQ STREET PACIFIC STREET GIBSON STREET AVE BROWN STREET STEEL STREET MORONEY TYRRELL STREET CORONA STREET BOLTON STREET 10 LAMAN STREET 9 KEMP STREET HALL ST DICK ST RAVENSHAW STREET Newcastle Beach QUEEN STREET BULL STREET GLOVERS LN COUNCIL STREET ALEXANDER STREET S W WATT STREET ARNOTT STREET PITT STREET -

Destination NSW Annual Report 2019/2020
INDEX & ACCESS Heading H2 Heading H3 DestinationUnt a cus, optia consequas volupidis voluptas alitasp NSW eribeaquame officab orehentio to magnate nonecabore, odita ilit quias que modita perum alibus. Henitiis dollut aperrovitin rererup tatur, sandit invel magnatus. Ame volorit veniscium voles dolumquodic tem rerum necus ANNUALsant fuga. Name rerum unt, eaqueREPORT re net ullaturenet ipsant ma comnis sit a vendeli genureius ma niendis plignih illabo. Ita ipitati onseque nemquibus aut aute cusdae voluptate nat rat. Cil il is rest platest et rate aliquam dolum faceseque derovit, atissusam quis eum re volorep edipsan daector eprorepelest 2019-2020verum que sintureperor simaximus et andis eat as dusa poriatium ant, qui andi consequam ima volo essit, nus cuptati busdaeria aborectibus, odi conseque esecus dolorem iunt as conseque voluptaturit laccus dolorit ipiet quaepro totatur epernatum enitatust, solorum eveliqu asperum is magnata turiorro quuntiam quostem porepe volum rem videnet ut quibus aut enistrum quaepro rerfera temquam autem etur audam faccusa nullam, undi quatibus eos simus re perroreictem eos sunt, ut volest, to ipsam quas ea conem lacerum exerae. Uptis endias estrum que pe pra DESTINATION NSW // Annual Report 2019-2020 Page 1 Destination NSW ANNUAL REPORT 2019-2020 The Hon. Stuart Ayres MP Minister for Jobs, Investment, Tourism and Western Sydney 52 Martin Place SYDNEY NSW 2000 30 November 2020 Dear Minister, We are pleased to submit the Annual Report of Destination NSW for the financial year ended 30 June 2020 for presentation to the NSW Parliament. This report has been prepared in accordance with the provisions of the Annual Reports (Statutory Bodies) Act 1984, the Annual Reports (Statutory Bodies) Regulation 2015, the Government Sector Employment Act 2013, the Public Finance and Audit Act 1983, and the Public Finance and Audit Regulation 2015. -

OFFICIAL POCKET GUIDE and MAP and GUIDE POCKET OFFICIAL Bars with Spectacular Harbour Views
visitnewcastle.com.au Welcome to Newcastle Discover See & Do Newcastle is one of Australia's oldest and most Despite having inspired Lonely Planet's admiration, interesting cities,offering a blend of new and old Newcastle is yet to be detected by the mass tourism architecture, a rich indigenous history, and one of radar. The seaside city of Newcastle is a great holiday the busiest ports in the world. The land and waters destination with a rich history, quirky arts culture and a of Newcastle are acknowledged as the country of thriving dining and shopping scene. Embark on one of the the Awabakal and Worimi peoples, whose culture many self-guided walking tours or learn how to surf. Spot is celebrated in community events, place naming, local marine life aboard Moonshadow Cruises or Nova signage and artworks. To learn more about Newcastle’s Cruises or get up close to Australian animals at Blackbutt history, take a walk through Newcastle Museum, 5 ways to experience Newcastle like a local Reserve, 182 hectares of natural bushland where you can walk the trails and discover the wildlife. Take a family day Eat & Drink Newcastle Maritime Centre, or visit Fort Scratchley Get your caffeine fix - Over the past few years, Newcastle Historic Site, at its commanding position guarding out to swing and climb like Tarzan at Tree Top Adventure Newcastle has an emerging food scene that makes it has created a coffee culture that gives Melbourne a run for the Hunter River Estuary. Explore Christ Church Park, or for something more relaxing, pack up the picnic an appealing spot to indulge in quality food and wine. -

Community News
KOORAGANG ISLAND ISSUE 1, 2020 COMMUNITY NEWS SURFEST’S TEAM CHALLENGE The 2020 Orica Team Challenge will be held at North Stockton Surfest Organiser Warren Smith said the Orica Team Beach on Saturday 1 and Sunday 2 February. Hosted by the Challenge has developed into a major event for Newcastle’s Northside Boardriders, the event will feature some of the best Surfest carnival. surfboard riding clubs in New South Wales competing for “The competition between the clubs is always very strong and $10,000 in prize money. exciting to watch. In addition, the hospitality of the Northside Orica Kooragang Island’s Manufacturing Centre Manager, Paul Boardriders is fantastic, as is the welcoming vibe from the Hastie, said: “This will mark our eighth year supporting the Stockton people.” Team Challenge at Stockton. The event is certainly a highlight in “We wish all teams the best of luck and hope for great waves our calendar. Not only does it showcase local surfing talent, it and weather.” also connects us with our community.” Pictured: 2019 Team Challenge winners with Orica’s Paul Hastie FRIDAY CHILL Are you looking for a way to unwind at the end of the week? Head Chill. From January through to the end of March, Friday Chill will down to Pacific Park Newcastle East every Friday until 27 March for beautifully activate Pacific Park with live music, fantastic food Soul Café’s Friday Chill, proudly sponsored by Orica. The family- and fun. As a local charity, this is our way of giving back to our friendly events which run from 6.30pm to 8.30pm will feature local community that supports us so well.” musicians, food trucks and lots of relaxed vibes. -

Newcastle Destination Management Plan 2021-2025 V Message from Our Lord Mayor
Newcastle Destination 2021-2025 Management Plan newcastle.nsw.gov.au Acknowledgment City of Newcastle acknowledges that we operate on the grounds of the traditional country of the Awabakal and Worimi peoples. We recognise and respect their cultural heritage, beliefs and continuing relationship with the land and waters, and that they are the proud survivors of more than two hundred years of dispossession. City of Newcastle reiterates its commitment to address disadvantages and attain justice for Aboriginal and Torres Strait Islander peoples of this community. City of Newcastle gratefully acknowledges the contribution made by stakeholders who took part in the consultation phase by attending workshops and meetings, including: Community members; Local businesses; and Regional and State Government Organisations Acronyms AAGR Average Annual Growth Rate LGA Local Government Area ABS Australian Bureau of Statistics LTO Local Toursim Organisation AHA Australian Hotels Association LQ Location Quotient BIA Business Improvement Association MICE Meetings, Incentives, CN City of Newcastle Conferences & Events DMP Destination Management Plan MTB Mountain Bike DNSW Destination NSW NBN National Broadband Network DPIE NSW Government - Department of NBT Nature-Based Tourism Planning, Industry and Environment NTIG Newcastle Tourism Industry Group DSSN Destination Sydney Surrounds North NVS National Visitor Survey EDS Economic Development Strategy PON Port of Newcastle FTE Full Time Equivalent TAA Tourism Accommodation Association HCCDC Hunter & Central Coast -

Government Gazette of the STATE of NEW SOUTH WALES Number 73 Friday, 15 May 2009 Published Under Authority by Government Advertising
2233 Government Gazette OF THE STATE OF NEW SOUTH WALES Number 73 Friday, 15 May 2009 Published under authority by Government Advertising LEGISLATION Online notification of the making of statutory instruments Week beginning 4 May 2009 THE following instruments were officially notified on the NSW legislation website (www.legislation.nsw.gov.au) on the dates indicated: Regulations and other statutory instruments Supreme Court Rules (Amendment No. 416) 2009 (2009-165) — published LW 8 May 2009 Uniform Civil Procedure Rules (Amendment No. 26) 2009 (2009-166) — published LW 8 May 2009 Environmental Planning Instruments Hornsby Shire Local Environmental Plan 1994 (Amendment No. 96) (2009-167) – published LW 8 May 2009 Lake Macquarie Local Environmental Plan 2004 (Amendment No. 34) (2009-168) – published LW 8 May 2009 Penrith Local Environmental Plan (Glenmore Park Stage 2) 2009 (2009-170) — published LW 8 May 2009 Penrith Local Environmental Plan No. 188 (Amendment No. 6) (2009-169) — published LW 8 May 2009 2234 LEGISLATION 15 May 2009 Acts of Parliament Assented To Legislative Assembly Office, Sydney 13 May 2009 IT is hereby notified, for general information, that Her Excellency the Governor has, in the name and on behalf of Her Majesty, this day assented to the undermentioned Acts passed by the Legislative Assembly and Legislative Council of New South Wales in Parliament assembled, viz.: Act No. 15 2009 – An Act to make miscellaneous amendments to various Acts administered by the Minister for Health; and for other purposes. [Health Legislation Amendment Bill] Act No. 16 2009 – An Act to amend the Telecommunications (Interception and Access) (New South Wales) Act 1987 to harmonise its provisions with those of the Telecommunications (Interception and Access) Act 1979 of the Commonwealth; and for other purposes. -

Live Afl Live and Exclusive Exclusively Live Monday
FRIDAY 1 JUNE SATURDAY 2 JUNE SUNDAY 3 JUNE MONDAY 4 JUNE 9.00am 11.30am 6.00am 8.30am 8.00am 6.00am 8.30am 9.30am 6.00am 9.00am 9.00am 6.00am GOLF ATHLETICS TENNIS LIVE: GOLF RUGBY LEAGUE TENNIS LIVE: GOLF RUGBY UNION TENNIS LIVE: GOLF RUGBY LEAGUE TENNIS Wales Open Round 1 IAAF Athletics Weekly French Open Replays Champions Tour Titans v Cowboys Replay French Open Replays Champions Tour Waratahs v Hurricanes Replay French Open Replays Principal Classic Final Round Sea Eagles v Dragons Replay French Open Replays 12.00pm 12.00pm 7.00pm Principal Charity Round 1 9.30am 5.30pm Principal Classic Round 2 10.30am 7.00pm 11.30am 10.30am 7.00pm CRICKET RUGBY UNION LIVE: TENNIS 12.00pm RUGBY UNION LIVE: RUGBY UNION 1.30pm RUGBY LEAGUE LIVE: TENNIS GOLF RUGBY LEAGUE LIVE: TENNIS Hampshire v Nottinghamshire The Rugby Club French Open Day 6 GOLF Crusaders v Highlanders Replay Blues v Chiefs FOOTBALL Bulldogs v Rabbitohs Replay French Open Day 8 Wales Open Final Round Titans v Cowboys Replay French Open Day 9 2.30pm 1.00pm Wales Open Round 2 10.30am 7.30pm Denmark v Australia Replay 11.30am Replay 12.00pm RUGBY LEAGUE RUGBY UNION 2.00pm RUGBY UNION LIVE: RUGBY UNION 3.00pm LIVE: RUGBY LEAGUE 1.30pm RUGBY LEAGUE LIVE: AFL LIVE: AFL CRICKET NRL Highlights Show Head To Head Rebels v Brumbies Replay Waratahs v Hurricanes Toyota Cup Raiders v Wests Tigers Replay Hawthorn v North Melbourne Sydney v Bulldogs Warriors v Storm Durham v Nottinghamshire 3.30pm 2.30pm 10.00am 12.00pm 9.30pm 11.00am 1.30pm 5.00am 5.00pm 6.00pm 2.00pm Replay RUGBY LEAGUE RUGBY -

NSW Central Coast
PDF Australia NSW Central Coast (PDF Chapter) Edition 18th Edition, Nov 2015 Pages 16 COVERAGE INCLUDES: Page Range 143–156 • Central Coast • Australian Reptile Useful Links Park Want more guides? • Brisbane Water Head to our shop National Park Trouble with your PDF? • Newcastle Trouble shoot here • Hunter Valley Need more help? Head to our FAQs Stay in touch Contact us here © Lonely Planet Publications Pty Ltd. To make it easier for you to use, access to this PDF chapter is not digitally restricted. In return, we think it’s fair to ask you to use it for personal, non-commercial purposes only. In other words, please don’t upload this chapter to a peer-to-peer site, mass email it to everyone you know, or resell it. See the terms and conditions on our site for a longer way of saying the above – ‘Do the right thing with our content’. ©Lonely Planet Publications Pty Ltd NSW Central Coast Includes ¨ Why Go? Central Coast .......145 After limping through the traffic of Sydney’s northern sub- Newcastle ..........146 urbs it would be forgivable to make a break for the freeway Hunter Valley ........151 as soon as it begins. Truth be told, much of the heavily pop- ulated Central Coast is a family-orientated suburbia-on-sea. But if you only have a couple of days to escape the big smoke, you will find some delightful diversions along this 100km stretch of coast. There are golden surf beaches, hid- Best Places to Eat den hamlets and languid inland lakes, the largest of which, ¨ Pearls on the Beach (p145) Lake Macquarie, covers four times the area of Sydney Har- bour.