Extracellular Matrix Remodeling in the Retina and Optic Nerve of a Novel Glaucoma Mouse Model
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recombinant Laminin Α5 LG1-3 Domains Support the Stemness of Human Mesenchymal Stem Cells
EXPERIMENTAL AND THERAPEUTIC MEDICINE 21: 166, 2021 Recombinant laminin α5 LG1-3 domains support the stemness of human mesenchymal stem cells SUJIN LEE1*, DONG‑SUNG LEE2* and JUN‑HYEOG JANG1 1Department of Biochemistry, College of Medicine, Inha University, Incheon 22212; 2College of Pharmacy, Chosun University, Gwangju 61452, Republic of Korea Received April 23, 2020; Accepted November 24, 2020 DOI: 10.3892/etm.2020.9597 Abstract. The extracellular matrix components laminin and be met by mimicking the in vivo extracellular matrix (ECM) elastin serve key roles in stem cell therapy. Elastin‑like poly‑ configuration, thereby modulating the activity of stem cells peptides (ELPs), derived from a soluble form of elastin, affect in vitro (2). The principle behind this hypothesis is that the the proliferation and differentiation of various types of cells. ECM not only functions as structural support for stem cells In the present study, a novel protein was designed containing in vivo but also provides biochemical cues for their mainte‑ globular domains 1‑3 of laminin α5 (Lα5LG1‑3) fused to nance versus directed differentiation (3). ELPs (Lα5LG1‑3/ELP). Lα5LG1‑3/ELP was expressed in Basement membranes (BMs) are a subgroup of the ECM Escherichia coli and displayed a molecular size of ~70 kDa that is necessary for cell differentiation during early devel‑ on 12% SDS‑polyacrylamide gels. The cellular activities, opmental processes. In addition, BMs are critical for the such as cellular adhesion (adhesion assay) and proliferation formation and maintenance of mature tissues (4,5). Laminin, (MTT cytotoxicity assay), of human mesenchymal stem one of the components of BMs, consists of three genetically cells (hMSCs) treated with 1 µg/ml of Lα5LG1‑3/ELP were distinct subunits called α, β and γ chains, which are assembled enhanced compared with those of untreated cells. -

Collagen and Elastin Fibres
J Clin Pathol: first published as 10.1136/jcp.s3-12.1.49 on 1 January 1978. Downloaded from J. clin. Path., 31, Suppl. (Roy. Coll. Path.), 12, 49-58 Collagen and elastin fibres A. J. BAILEY From the Agricultural Research Council, Meat Research Institute, Langford, Bristol Although an understanding of the intracellular native collagen was generated from type I pro- biosynthesis of both collagen and elastin is of collagen. Whether this means that the two pro- considerable importance it is the subsequent extra- collagens are converted by different enzyme systems cellular changes involving fibrogenesis and cross- and the type III enzyme was deficient in these linking that ensure that these proteins ultimately fibroblast cultures, or that the processing of pro become the major supporting tissues of the body. type III is extremely slow, is not known. The latter This paper summarises the formation and stability proposal is consistent with the higher proportion of collagen and elastin fibres. of soluble pro type III extractable from tissue (Lenaers and Lapiere, 1975; Timpl et al., 1975). Collagen Basement membrane collagens, on the other hand, do not form fibres and this property may be The non-helical regions at the ends of the triple due to the retention of the non-helical extension helix of procollagen probably provide a number of peptides (Kefalides, 1973). In-vivo biosynthetic different intracellular functions-that is, initiating studies showing the absence of any extension peptide rapid formation of the triple helix; inhibiting intra- removal support this (Minor et al., 1976), but other cellular fibrillogenesis; and facilitating transmem- workers have reported that there is some cleavage brane movement. -

Immunohistochemical Expression of Tenascin and Elastin In
Clinical Obstetrics, Gynecology and Reproductive Medicine Research Article ISSN: 2059-4828 Immunohistochemical expression of tenascin and elastin in women with pelvic organ prolapse and/or without stress urinary incontinence Ilias Liapis1, Panagiotis Bakas2, Pafiti-Kondi Agatha3, Matrona Frangou-Plemenou4, Charalampos Karachalios5*, Dimos Sioutis6 and Aggelos Liapis2 1Birmingham Women’s and Children’s Hospital, NHS Foundation Trust, Health Education England Midlands and East-West Midlands, Birmingham, England, United Kingdom 2Second Department of Obstetrics and Gynecology, Aretaieio University Hospital, School of Health Sciences, Medical School, National and Kapodistrian University of Athens, Athens, Attica, Greece 3Pathology Laboratory, Aretaieio University Hospital, School of Health Sciences, Medical School, National and Kapodistrian University of Athens, Athens, Attica, Greece 4Microbiology Laboratory, Aretaieio University Hospital, School of Health Sciences, Medical School, National and Kapodistrian University of Athens, Athens, Attica, Greece 5Second Department of Obstetrics and Gynecology, Aretaieio University Hospital, School of Health Sciences, Medical School, National and Kapodistrian University of Athens, Athens, Attica, Greece 6Third Department of Obstetrics and Gynecology, Attikon University Hospital, School of Health Sciences, Medical School, National and Kapodistrian University of Athens, Athens, Attica, Greece Abstract Background and aim: Pelvic organ prolapse (POP) and stress urinary incontinence (SUI) constitute entities of pelvic floor disorders and most often occur simultaneously in the same patient, adversely affecting women’s quality of life. The pathogenesis of pelvic organ prolapse and stress urinary incontinence is not fully understood. The pelvic viscera are maintained in their place thanks to interconnection of levator ani muscles, cardinal and uterosacral ligaments, and pubocervical and rectovaginal fascia. Ligaments and fascia consist mainly of connective tissue. -

Evaluation of Elastin/Collagen Content in Human Dermis In-Vivo by Multiphoton Tomography—Variation with Depth and Correlation with Aging
Cosmetics 2014, 1, 211-221; doi:10.3390/cosmetics1030211 OPEN ACCESS cosmetics ISSN 2079-9284 www.mdpi.com/journal/cosmetics Article Evaluation of Elastin/Collagen Content in Human Dermis in-Vivo by Multiphoton Tomography—Variation with Depth and Correlation with Aging Jean-Christophe Pittet 1,*, Olga Freis 2,†, Marie-Danielle Vazquez-Duchêne 2,†, Gilles Périé 2,† and Gilles Pauly 2,† 1 Orion Concept, 100 Rue de Suède, 37100 Tours, France 2 BASF Beauty Care Solutions France SAS, 3 Rue de Seichamps, CS 71040 Pulnoy, 54272 Essey-lès-Nancy Cedex, France; E-Mails: [email protected] (O.F.); [email protected] (M.-D.V.-D.); [email protected] (G.Pé.); [email protected] (G.Pa.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +33-247-052-316; Fax: +33-610-786-695. Received: 14 March 2014; in revised form: 31 July 2014 / Accepted: 1 August 2014 / Published: 20 August 2014 Abstract: The aim of this study was to evaluate the influence of the depth of the dermis on the measured collagen and elastin levels and to establish the correlation between the amount of these two extracellular matrix (ECM) components and age. Multiphoton Microscopy (MPM) that measures the autofluorescence (AF) and second harmonic generation (SHG) was used to quantify the levels of elastin and collagen and to determine the SAAID (SHG-to-AF Aging Index of Dermis) at two different skin depths. A 50 MHz ultrasound scanner was used for the calculation of the Sub Epidermal Non Echogenic Band (SENEB). -
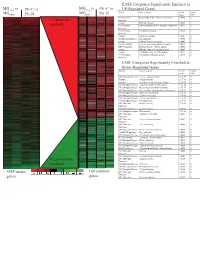
Supplement 1 Microarray Studies
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

The Beneficial Regulation of Extracellular Matrix
cosmetics Article The Beneficial Regulation of Extracellular Matrix and Heat Shock Proteins, and the Inhibition of Cellular Oxidative Stress Effects and Inflammatory Cytokines by 1α, 25 dihydroxyvitaminD3 in Non-Irradiated and Ultraviolet Radiated Dermal Fibroblasts Neena Philips *, Xinxing Ding, Pranathi Kandalai, Ilonka Marte, Hunter Krawczyk and Richard Richardson School of Natural Sciences, Fairleigh Dickinson University, Teaneck, NJ 07601, USA * Correspondence: [email protected] or [email protected] Received: 30 June 2019; Accepted: 20 July 2019; Published: 1 August 2019 Abstract: Intrinsic skin aging and photoaging, from exposure to ultraviolet (UV) radiation, are associated with altered regulation of genes associated with the extracellular matrix (ECM) and inflammation, as well as cellular damage from oxidative stress. The regulatory properties of 1α, 25dihydroxyvitamin D3 (vitamin D) include endocrine, ECM regulation, cell differentiation, photoprotection, and anti-inflammation. The goal of this research was to identify the beneficial effects of vitamin D in preventing intrinsic skin aging and photoaging, through its direct effects as well as its effects on the ECM, associated heat shock proteins (HSP-47, and -70), cellular oxidative stress effects, and inflammatory cytokines [interleukin (IL)-1 and IL-8] in non-irradiated, UVA-radiated, UVB-radiated dermal fibroblasts. With regard to the ECM, vitamin D stimulated type I collagen and inhibited cellular elastase activity in non-irradiated fibroblasts; and stimulated type I collagen and HSP-47, and inhibited elastin expression and elastase activity in UVA-radiated dermal fibroblasts. With regard to cellular protection, vitamin D inhibited oxidative damage to DNA, RNA, and lipids in non-irradiated, UVA-radiated and UVB-radiated fibroblasts, and, in addition, increased cell viability of UVB-radiated cells. -

Binding of Recombinant Human Cytokeratin 19 to Laminin
CELL STRUCTURE AND FUNCTION 25: 171–175 (2000) © 2000 by Japan Society for Cell Biology Binding of Recombinant Human Cytokeratin 19 to Laminin: A Possible Role in Interaction between Intermediate Filament Derived from Epithelial Cells and Extracellular Matrixes Naomi Dobashi1, Jiro Fujita1,*, Masayuki Murota2, Yuji Ohtsuki3, Shuji Bandoh1, Yutaka Ueda1, Kazutaka Dohmoto1, Satoko Hojo1, Mikio Nishioka2, Toshihiko Ishida, and Jiro Takahara1 1First Department of Internal Medicine, Kagawa Medical University, Kagawa 2Third Department of Internal Medicine, Kagawa Medical University, Kagawa 3Department of Pathology, Kochi Medical School, Kochi, Japan ABSTRACT. Cytokeratin 8 (CK8) and cytokeratin 19 (CK19) is a specific cytoskeletal component of simple epi- thelia, including bronchial epithelial cells. We hypothesized that CK8 or CK19 released from epithelial cells may bind to and cause damage to extracellular matrixes through binding of anti-CK8 or anti-CK19 autoantibodies. In the present study, bindings of recombinant human CK8 and CK19 to laminin (both derived from mouse sarcoma cells and human), collagen, gelatin, and fibronectin were evaluated by a modified enzyme-linked immunosorbent assay (ELISA). In addition, binding of CK19 to laminin was also confirmed by inhibition assay. As a result, CK19 strongly bound to mouse laminin as well as human laminin. Pretreatment with laminin significantly reduced the binding of CK19 to laminin. However, binding of recombinant CK19 to laminin was not demonstrated by Western immunoblot, suggesting that SDS treatment of laminin diminished the binding. These results suggest that released CK19 from epithelial cells may have played a role in the damage of basement membrane by accumulation of an immune complex composed by CK19 and anti-CK19 autoantibody. -

Proteins and Peptides As Important Modifiers of the Polymer Scaffolds
polymers Review Proteins and Peptides as Important Modifiers of the Polymer Scaffolds for Tissue Engineering Applications—A Review Katarzyna Klimek * and Grazyna Ginalska Chair and Department of Biochemistry and Biotechnology, Medical University of Lublin, Chodzki 1 Street, 20-093 Lublin, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-81-448-7028; +48-81-448-7020 Received: 29 January 2020; Accepted: 2 April 2020; Published: 6 April 2020 Abstract: Polymer scaffolds constitute a very interesting strategy for tissue engineering. Even though they are generally non-toxic, in some cases, they may not provide suitable support for cell adhesion, proliferation, and differentiation, which decelerates tissue regeneration. To improve biological properties, scaffolds are frequently enriched with bioactive molecules, inter alia extracellular matrix proteins, adhesive peptides, growth factors, hormones, and cytokines. Although there are many papers describing synthesis and properties of polymer scaffolds enriched with proteins or peptides, few reviews comprehensively summarize these bioactive molecules. Thus, this review presents the current knowledge about the most important proteins and peptides used for modification of polymer scaffolds for tissue engineering. This paper also describes the influence of addition of proteins and peptides on physicochemical, mechanical, and biological properties of polymer scaffolds. Moreover, this article sums up the major applications of some biodegradable natural and synthetic polymer scaffolds modified with proteins and peptides, which have been developed within the past five years. Keywords: bioactive construct; biocompatibility; biomolecules; cytotoxicity; ECM; hydrogels; protein carrier; regenerative medicine; stem cells; tissue repair 1. Introduction: The Role of Proteins and Peptides in TE Tissue engineering (TE) is a multidisciplinary field, which constitutes an alternative and promising approach for grafts, i.e., autografts, allografts, and xenografts [1–3]. -

Congenital Muscular Dystrophy Due to Laminin Α2 (Merosin) Deficiency (MDC1A) in an Ethnic Malay Girl 1MK Thong, 3Sofiah Ali,4 YE Park, 5DS Kim, 6KJ Goh, 2KT Wong
Neurology Asia 2017; 22(2) : 155 – 159 Congenital muscular dystrophy due to laminin α2 (merosin) deficiency (MDC1A) in an ethnic Malay girl 1MK Thong, 3Sofiah Ali, 4YE Park, 5DS Kim, 6KJ Goh, 2KT Wong 1Departments of Paediatrics, 2Pathology and 6Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia; 3Sime Darby Medical Centre, Subang Jaya, Selangor, Malaysia; 4Department of Neurology and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea; 5Department of Neurology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea Abstract We report the first known ethnic Malay patient with laminin alpha-2 (merosin) deficiency (MDC1A), a subtype of congenital muscular dystrophy (CMD)as a result of novel LAMA2 gene mutations. The 21-month-old female presented with hypotonia at birth and gross motor delay of her distal lower limbs. Physical examination showed generalised hypotonia, hyporeflexia and myopathic facies but good cognitive functions. Serum creatine kinase was elevated and white matter changes were detected in the brain MRI. Muscle biopsy showed dystrophic changes with complete laminin α2 deficiency by immunohistochemistry. Mutation analysis of LAMA2 showed compound heterozygote at exon 21, c.2888delG(p.Gly963Alafs*111) and exon 34, c.4886dupC(p.Pro1629Profs*40) leading to premature stop codon for each of the frameshift mutations. Patient review at seven years of age showed satisfactory cognitive functions despite having contractures and weakness. Genetic testing of LAMA2 related muscular dystrophy facilitated the earlier diagnosis of MDC1A and genetic counselling for this family. Keywords: laminin alpha-2 deficiency; merosin deficiency. LAMA2, Malaysia, congenital muscular dystrophy, MDC1A INTRODUCTION mutations in the laminin alpha-2 (LAMA2)gene. -

Elastin Biology and Tissue Engineering with Adult Cells
DOI 10.1515/bmc-2012-0040 BioMol Concepts 2013; 4(2): 173–185 Review Cassandra B. Saitow * , Steven G. Wise, Anthony S. Weiss , John J. Castellot Jr. and David L. Kaplan Elastin biology and tissue engineering with adult cells Abstract: The inability of adult cells to produce well-organ- collagen to allow for repeated cycles of expansion and ized, robust elastic fibers has long been a barrier to the contraction in response to pulsatile flow (3) . This review successful engineering of certain tissues. In this review, focuses primarily on blood vessel tissue engineering, we focus primarily on elastin with respect to tissue-engi- particularly the challenge of inducing sufficient elastin neered vascular substitutes. To understand elastin regu- expression from cells that colonize vascular constructs. lation during normal development, we describe the role Developmental regulation of elastin dictates that of various elastic fiber accessory proteins. Biochemical synthesis is predominantly in utero and early childhood pathways regulating expression of the elastin gene are (4) . New elastic fibers are not produced in appreciable addressed, with particular focus on tissue-engineering amounts under normal physiological circumstances in research using adult-derived cells. adult cells. This deficit presents a significant challenge in tissue engineering of vascular constructs that seek Keywords: elastin; heparin; smooth muscle cell; vascular to replicate the elastin content of natural vessels. This tissue engineering. review considers factors involved in elastic fiber forma- tion during normal development and addresses recent advances in the induction of elastin expression by cells *Corresponding author : Cassandra B. Saitow, Tufts University, from adult donors. Department of Biomedical Engineering, Medford, MA, 02155 , USA, e-mail: [email protected] Steven G. -

Blood Vitronectin Is a Major Activator of LIF and IL-6 in the Brain Through Integrin–FAK and Upar Signaling Matthew P
© 2018. Published by The Company of Biologists Ltd | Journal of Cell Science (2018) 131, jcs202580. doi:10.1242/jcs.202580 RESEARCH ARTICLE Blood vitronectin is a major activator of LIF and IL-6 in the brain through integrin–FAK and uPAR signaling Matthew P. Keasey1, Cuihong Jia1, Lylyan F. Pimentel1,2, Richard R. Sante1, Chiharu Lovins1 and Theo Hagg1,* ABSTRACT Microglia and astrocytes express the VTN receptors αvβ3 and α β We defined how blood-derived vitronectin (VTN) rapidly and potently v 5 integrin (Herrera-Molina et al., 2012; Kang et al., 2008; activates leukemia inhibitory factor (LIF) and pro-inflammatory Milner, 2009; Welser-Alves et al., 2011). Microglia and astrocytes, interleukin 6 (IL-6) in vitro and after vascular injury in the brain. as well as endothelial cells, are major producers of pro- α in vitro Treatment with VTN (but not fibrinogen, fibronectin, laminin-111 or inflammatory cytokines, such as IL-6 and TNF , and collagen-I) substantially increased LIF and IL-6 within 4 h in after traumatic or ischemic injury to the brain (Banner et al., 1997; C6-astroglioma cells, while VTN−/− mouse plasma was less effective Erta et al., 2012; Lau and Yu, 2001) or upon self-induction by IL-6 than that from wild-type mice. LIF and IL-6 were induced by (Van Wagoner and Benveniste, 1999). IL-6 is a major regulator of a intracerebral injection of recombinant human (rh)VTN in mice, but variety of inflammatory disorders and a target for therapies (Hunter induction seen upon intracerebral hemorrhage was less in VTN−/− and Jones, 2015). -

Tenascins in Stem Cell Niches
MATBIO-01031; No of Pages 12 Matrix Biology xxx (2014) xxx–xxx Contents lists available at ScienceDirect Matrix Biology journal homepage: www.elsevier.com/locate/matbio Tenascins in stem cell niches Ruth Chiquet-Ehrismann a,b,⁎,1,GertraudOrendc,d,e,f,1, Matthias Chiquet g,1, Richard P. Tucker h,1, Kim S. Midwood i,1 a Friedrich Miescher Institute of Biomedical Research, Novartis Research Foundation, Maulbeerstrasse 66 CH-4058 Basel, Switzerland b Faculty of Sciences, University of Basel, Switzerland c Inserm U1109, The Microenvironmental Niche in Tumorigenesis and Targeted Therapy (MNT3) Team, 3 av. Molière, 67200 Strasbourg, France d Université de Strasbourg, 67000 Strasbourg, France e LabEx Medalis, Université de Strasbourg, 67000 Strasbourg, France f Fédération de Médecine Translationnelle de Strasbourg (FMTS), 67000 Strasbourg, France g Department of Orthodontics and Dentofacial Orthopedics, University of Bern, Freiburgstrasse 7, CH-3010 Bern, Switzerland h Department of Cell Biology and Human Anatomy, University of California Davis, Davis, CA 95616, USA i The Kennedy Institute of Rheumatology, University of Oxford, Roosevelt Drive, Headington, Oxford OX3 7FY, United Kingdom article info abstract Available online xxxx Tenascins are extracellular matrix proteins with distinct spatial and temporal expression during development, tissue homeostasis and disease. Based on their expression patterns and knockout phenotypes an important Keywords: role of tenascins in tissue formation, cell adhesion modulation, regulation of proliferation and