New Sedation and General Anesthesia Guidelines Why the Changes?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diazepam - Alcohol Withdrawal
Diazepam - alcohol withdrawal Why have I been prescribed diazepam? If a person stops drinking alcohol after a time of drinking too much they can experience withdrawal effects. These include “the shakes”, sweating, having fits, seeing things which are not there (hallucinations) and feeling anxious and low in mood. They can feel wound up and find it difficult to sleep. These withdrawal effects can be very uncomfortable and in extreme cases can be dangerous if they persist into “DTs” (delirium tremens). Diazepam is used to help reduce these withdrawal symptoms. It relieves anxiety and tension and aids sleep. Diazepam can also prevent fits. It controls the withdrawal symptoms until the body is free of alcohol and has settled down. This usually takes three to seven days from the time you stop drinking. What exactly is diazepam? Diazepam is a benzodiazepine. This group of medicines is also called anxiolytics or minor tranquillisers. Diazepam has many uses. It can be used to reduce symptoms of anxiety and insomnia, as well as to help people come off alcohol. Diazepam should only be prescribed and taken as a short course. Is diazepam safe to take? Diazepam is safe to take for a short period of time, but it doesn’t suit everyone. Below are a few conditions where diazepam may be less suitable. If any of these apply to you please tell your doctor or key-worker. If you have depression or a mental illness If you have lung disease or breathing problems, or suffer from liver or kidney trouble If you take any other medicines or drugs, including those on prescription and bought from a chemist If you take illicit drugs bought “on the street” If you are pregnant or breast-feeding What is the usual dose of diazepam? The dose of diazepam will usually be started at 10-20mg four times a day. -
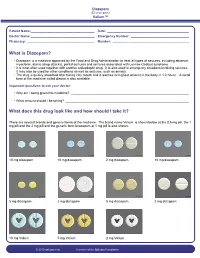
What Is Diazepam?
Diazepam (Di-a-ze-pam) Valium™ Patient Name: ___________________________________ Date: _____________________________________________ Doctor Name: ___________________________________ Emergency Number: ________________________________ Pharmacy: _____________________________________ Number: __________________________________________ What is Diazepam? • Diazepam is a medicine approved by the Food and Drug Administration to treat all types of seizures, including absence, myoclonic, atonic (drop attacks), partial seizures and seizures associated with Lennox-Gastaut syndrome. • It is most often used together with another antiepileptic drug. It is also used in emergency situations involving seizures. It may also be used for other conditions as well as seizures, such as anxiety. • The drug is quickly absorbed after taking it by mouth and it reaches its highest amount in the body in 1-2 hours. A rectal form of the medicine called diastat is also available. Important questions to ask your doctor: • Why am I being given this medicine? _________________________________________________________________ • What amount should I be taking? ____________________________________________________________________ What does this drug look like and how should I take it? There are several brands and generic forms of the medicine. The brand name Valium is shown below at the 0.5 mg pill, the 1 mg pill and the 2 mg pill and the generic form lorazepam at 1 mg pill is also shown. 10 mg diazepam 10 mg diazepam 2 mg diazepam 10 mg diazepam 5 mg diazepam 2 mg diazepam 5 mg diazepam 2 mg diazepam 10 mg Valium 5 mg Valium 2 mg Valium © 2010 epilepsy.com A service of the Epilepsy Foundation Diazepam (Di-a-ze-pam) Valium™ Frequently Asked Questions: How do I take Diazepam? To use the tablet form: chew tablets and swallow or swallow the tablet whole. -

Early Morning Insomnia, Daytime Anxiety, and Organic Mental Disorder Associated with Triazolam
Early Morning Insomnia, Daytime Anxiety, and Organic Mental Disorder Associated with Triazolam Tjiauw-Ling Tan, MD, Edward 0. Bixler, PhD, Anthony Kales, MD, Roger J. Cadieux, MD, and Amy L. Goodman, MD Hershey, Pennsylvania A psychiatric syndrome characterized by agita Sleep Disorders Clinic. He began taking triazolam tion, paranoid ideation, depersonalization, and de at bedtime in a 0.5-mg dose eight months before pression, as well as paresthesias and hyperacusis, his referral. Although the drug was effective ini has been attributed to administration of triazolam tially, tolerance developed, causing the patient to (Halcion).1 The occurrence of these reactions led gradually increase the dosage until eventually he to the removal of the drug from the market in the was taking a total of 1.5 mg nightly. Netherlands. Isolated behavioral side effects that The physical examination revealed no contribu include amnesia2-4 and hallucinations5 have also tory conditions. However, assessment of the pa been reported with administration of triazolam. tient’s mental status revealed that he was extreme Rebound insomnia6 and early morning insom ly guarded and suspicious and preoccupied with nia,7 both associated with increases in daytime his sleeplessness to the degree that this hypochon anxiety,7,8 are withdrawal syndromes known driacal concern had a delusional quality. He also to occur with rapidly eliminated benzodiazepine described two episodes indicating memory impair hypnotics such as triazolam. Rebound insomnia ment; both incidents occurred in the late afternoon consists of a marked increase in wakefulness and involved preparing to eat certain foods, which above baseline levels following drug withdrawal. -

Triazolam (Halcion®) Instructions
Mark Sebastian, DMD 33516 Ninth Ave. South, #2 Federal Way, WA 98003 (253) 941-6242 --or -- (253) 952-2005 [email protected] www.MarkSebastianDMD.com Triazolam (Halcion®) instructions If prescribed, take the diazepam (Valium®) pill just before bed the night before your dental surgery for a better night’s sleep. If you take other sleeping medications, take those instead of the diazepam (Valium®). Do not mix the two. If you have a morning appointment, you should to fast from solid foods after midnight. If you have an afternoon appointment, have a light breakfast. Unless you have a medical reason to eat (diabetic, etc.), do not eat anything for 6 hours before your appointment time. Water, apple juice, and black decaffeinated coffee/tea are OK for 3 hours before your appointment. Triazolam (Halcion®) is absorbed better on an empty stomach. Do not take caffeine or sugar) for 3 hours before your appointment, as all are stimulants that decrease the effectiveness of triazolam (Halcion®). No tobacco use for 8 hours before, as it is a stimulant. Take the triazolam (Halcion®) or diazepam (Valium®) pill(s) with a glass of water. Sparkling water makes them absorb better. Alcohol---do not drink within 24 hours before to 24 hours after taking triazolam (Halcion®) or diazepam (Valium®). Recreational/illegal drugs---Do not use for 7 days before your dental surgery and until 7 days after (never if you are taking narcotic pain medication). Example—using cocaine and then having local anesthetics (novocaine) can kill you. Do not take triazolam (Halcion®) or diazepam (Valium®) if you are allergic to triazolam (Halcion®), alprazolam (Xanax®), chlordiazepoxide (Librium®, Librax®), clonazepam (Klonopin®), clorazepate (Tranxene®), diazepam (Valium®), estazolam (ProSom®), flurazepam (Dalmane®), lorazepam (Ativan®), oxazepam (Serax®), prazepam (Centrax®), temazepam (Restoril®). -

Effects of Benzodiazepines on Sleep and Wakefulness
Br. J. clin. Pharmac. (1981), 11, 31S-35S EFFECTS OF BENZODIAZEPINES ON SLEEP AND WAKEFULNESS T. ROTH, F. ZORICK, JEANNE SICKLESTEEL & E. STEPANSKI Sleep Disorders and Research Center, Henry Ford Hospital, Detroit, Michigan The differential effects of short and long acting benzodiazepines on sleeping and waking behaviour are discussed, with particular reference to hypnotic efficacy, and their effects on the structure ofsleep and daytime function. Introduction THE evaluation of any drug requires an understand- et al., 1979), and triazolam (Metzler et al., 1977) have ing of the conditions in which it is going to be used come into clinical use. The present report will present clinically. In the case of hypnotics, the most appro- the differential effects of short- and long-acting ben- priate use is symptomatic relief for the complaint of zodiazepines on sleeping and waking behaviour. insomnia. To understand fully the safety and efficacy ofthese drugs, we must first be aware of the constella- tion of symptoms associated with the complaint of Sleep parameters insomnia, as well as what these drugs do to each of these symptoms. In evaluating the effects of hypnotics on sleep, two Insomnia is a complaint. Although all of the types of parameters should be considered. The first aetiological factors which give rise to this symptom set of parameters deal with hypnotic efficacy and are not currently well understood, there is an accepted include measures such as latency to sleep onset, total diagnostic system for the various disorders associated sleep time, number and duration of awakenings, and with disturbed nocturnal sleep (Association of Sleep sleep efficiency. -

Comparison of Short-And Long-Acting Benzodiazepine-Receptor Agonists
J Pharmacol Sci 107, 277 – 284 (2008)3 Journal of Pharmacological Sciences ©2008 The Japanese Pharmacological Society Full Paper Comparison of Short- and Long-Acting Benzodiazepine-Receptor Agonists With Different Receptor Selectivity on Motor Coordination and Muscle Relaxation Following Thiopental-Induced Anesthesia in Mice Mamoru Tanaka1, Katsuya Suemaru1,2,*, Shinichi Watanabe1, Ranji Cui2, Bingjin Li2, and Hiroaki Araki1,2 1Division of Pharmacy, Ehime University Hospital, Shitsukawa, Toon, Ehime 791-0295, Japan 2Department of Clinical Pharmacology and Pharmacy, Neuroscience, Ehime University Graduate School of Medicine, Shitsukawa, Toon, Ehime 791-0295, Japan Received November 7, 2007; Accepted May 15, 2008 Abstract. In this study, we compared the effects of Type I benzodiazepine receptor–selective agonists (zolpidem, quazepam) and Type I/II non-selective agonists (zopiclone, triazolam, nitrazepam) with either an ultra-short action (zolpidem, zopiclone, triazolam) or long action (quazepam, nitrazepam) on motor coordination (rota-rod test) and muscle relaxation (traction test) following the recovery from thiopental-induced anesthesia (20 mg/kg) in ddY mice. Zolpidem (3 mg/kg), zopiclone (6 mg/kg), and triazolam (0.3 mg/kg) similarly caused an approximately 2-fold prolongation of the thiopental-induced anesthesia. Nitrazepam (1 mg/kg) and quazepam (3 mg/kg) showed a 6- or 10-fold prolongation of the anesthesia, respectively. Zolpidem and zopiclone had no effect on the rota-rod and traction test. Moreover, zolpidem did not affect motor coordination and caused no muscle relaxation following the recovery from the thiopental-induced anesthesia. However, zopiclone significantly impaired the motor coordination at the beginning of the recovery. Triazolam significantly impaired the motor coordination and muscle relaxant activity by itself, and these impairments were markedly exacerbated after the recovery from anesthesia. -

Red with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Monotonous Simulated Driving
109 A 1986 The Carry-over Effects of Triazolam Compa- red with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Mono- tonous Simulated Driving Hans Laurell and Jan Törnroos Reprint from Acta Pharmacologica et toxicologica 1986 v Väg06/7 Efi/( Statens väg- och trafikinstitut (VTI) * 581 01 Linköping [St]tlltet Swedish Road and Traffic Research Institute * S-581 01 Linköping Sweden Acta pharmacol. et toxicol. 1986, 58, 182186. From the National Swedish Road and Traffic Research Institute, (V.T.I.), S-58 101 Linköping, Sweden The Carry-over Effects of Triazolam Compared with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Monotonous Simulated Driving Hans Laurell and Jan Törnros (Received October 9, 1985; Accepted January 9, 1986) Abstract: Eighteen healthy volunteers of both sexes, aged 2034, were tested in the morning while undertaking real car driving avoidance manoeuvres and during monotonous simulated driving after 1 and 3 nights of medication with triazolam 0.25 mg, nitrazepam 5 mg or placebo. The study was a double-blind, randomized, cross-over study, where a minimum of 7 days wash-out separated the 3 treatment periods. Nitrazepam was found to impair performance in the simulated task after 1 but not after 3 nights of medication. Performance in the triazolam condition was not signicantly different from the other conditions on this task on either day. However, after one night of medication triazolam tended to score worse than placebo but better than nitrazepam. In real car driving a tendency was noted for nitrazepam to score worst, whereas the difference between placebo and triazolam was hardly noticeable. -

Oral Sedation Instructions
Following your child’s appointment (Cont’d) DIET DO NOT feed your child until he/she is completely awake. Begin feeding with clear, pulp-free liquids such as water, apple juice, jello, popsicles or “sports” drinks. Start your child on semi-solid foods (such as soup, noodles, porridge, INSTRUCTIONS FOR PATIENTS WHO WILL BE oatmeal) for easy chewing and digestion. Only feed your child if RECEIVING ORAL SEDATION he/she is hungry and has tolerated clear liquids without vomiting. Avoid feeding your child large portions of food or fatty foods such as French fries. Goals of conscious sedation If your child vomits, stop feeding for 30-60 minutes then gradually resume clear fluids in sips. The goals of sedation in the pediatric patient for diagnostic and therapeutic Normal diet can be resumed as soon as he/she is ready for it. procedures are: 1) to guard the patient’s safety and welfare; 2) to minimize physical discomfort and pain; 3) to control anxiety, minimize psychological PAIN trauma, and maximize the potential for amnesia; 4) to control behavior and/or movement so as to allow the safe completion of the procedure; and 5) You will be notified if local anesthetic has been used during the to return the patient to a state in which safe discharge from medical procedure. It usually takes 2-3 hours to completely wear off. Make supervision, as determined by recognized criteria, is possible. sure you monitor your child closely to avoid any soft tissue trauma. The sedatives If he/she complains of pain, regular strength children’s Tylenol or Advil/Motrin is usually sufficient. -

Calculating Equivalent Doses of Oral Benzodiazepines
Calculating equivalent doses of oral benzodiazepines Background Benzodiazepines are the most commonly used anxiolytics and hypnotics (1). There are major differences in potency between different benzodiazepines and this difference in potency is important when switching from one benzodiazepine to another (2). Benzodiazepines also differ markedly in the speed in which they are metabolised and eliminated. With repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues) (2). The degree of sedation that they induce also varies, making it difficult to determine exact equivalents (3). Answer Advice on benzodiazepine conversion NB: Before using Table 1, read the notes below and the Limitations statement at the end of this document. Switching benzodiazepines may be advantageous for a variety of reasons, e.g. to a drug with a different half-life pre-discontinuation (4) or in the event of non-availability of a specific benzodiazepine. With relatively short-acting benzodiazepines such as alprazolam and lorazepam, it is not possible to achieve a smooth decline in blood and tissue concentrations during benzodiazepine withdrawal. These drugs are eliminated fairly rapidly with the result that concentrations fluctuate with peaks and troughs between each dose. It is necessary to take the tablets several times a day and many people experience a "mini-withdrawal", sometimes a craving, between each dose. For people withdrawing from these potent, short-acting drugs it has been advised that they switch to an equivalent dose of a benzodiazepine with a long half life such as diazepam (5). Diazepam is available as 2mg tablets which can be halved to give 1mg doses. -

Drugs of Abuse: Benzodiazepines
Drugs of Abuse: Benzodiazepines What are Benzodiazepines? Benzodiazepines are central nervous system depressants that produce sedation, induce sleep, relieve anxiety and muscle spasms, and prevent seizures. What is their origin? Benzodiazepines are only legally available through prescription. Many abusers maintain their drug supply by getting prescriptions from several doctors, forging prescriptions, or buying them illicitly. Alprazolam and diazepam are the two most frequently encountered benzodiazepines on the illicit market. Benzodiazepines are What are common street names? depressants legally available Common street names include Benzos and Downers. through prescription. Abuse is associated with What do they look like? adolescents and young The most common benzodiazepines are the prescription drugs ® ® ® ® ® adults who take the drug Valium , Xanax , Halcion , Ativan , and Klonopin . Tolerance can orally or crush it up and develop, although at variable rates and to different degrees. short it to get high. Shorter-acting benzodiazepines used to manage insomnia include estazolam (ProSom®), flurazepam (Dalmane®), temazepam (Restoril®), Benzodiazepines slow down and triazolam (Halcion®). Midazolam (Versed®), a short-acting the central nervous system. benzodiazepine, is utilized for sedation, anxiety, and amnesia in critical Overdose effects include care settings and prior to anesthesia. It is available in the United States shallow respiration, clammy as an injectable preparation and as a syrup (primarily for pediatric skin, dilated pupils, weak patients). and rapid pulse, coma, and possible death. Benzodiazepines with a longer duration of action are utilized to treat insomnia in patients with daytime anxiety. These benzodiazepines include alprazolam (Xanax®), chlordiazepoxide (Librium®), clorazepate (Tranxene®), diazepam (Valium®), halazepam (Paxipam®), lorzepam (Ativan®), oxazepam (Serax®), prazepam (Centrax®), and quazepam (Doral®). -

HYPAM Tablet Contains 0.125 Mg Or 0.25 Mg of Triazolam
NEW ZEALAND DATA SHEET HYPAM 1. Product Name HYPAM, 0.125 mg, 0.25mg, tablets. 2. Qualitative and Quantitative Composition Each HYPAM tablet contains 0.125 mg or 0.25 mg of triazolam. HYPAM tablets contain lactose. For the full list of excipients, see section 6.1. 3. Pharmaceutical Form HYPAM 0.125mg tablets are oval, flat, bevelled edged white tablets marked TZ on one side and scored on the other. HYPAM 0.25mg tablets are oval, flat, bevelled edged blue tablets marked TZ on one side and scored on the other. Dimensions (both strengths): 7.9mm x 5.6mm. The score line is not intended for breaking the tablet. 4. Clinical Particulars 4.1 Therapeutic indications Triazolam is useful in the management of patients with transient up to 7 days, and short term 2 to 4 weeks, severe or disabling insomnia. It is also useful as a short term, intermittent adjunctive treatment in the management of selected patients with long term insomnia. 4.2 Dose and method of administration Dose The lowest effective dose of triazolam should be used. Treatment with triazolam should not exceed 7-10 consecutive days. Use for more than 2-3 consecutive weeks requires complete re-evaluation of the patient. The starting dose in all patients should be 0.125mg; for many patients this dose immediately before retiring should be sufficient. A dose of 0.25mg should not be exceeded. For elderly or debilitated patients and patients with disturbed liver/kidney function, the dose should not exceed 0.125mg before retiring. The 0.25mg dose should be used only for exceptional patients who do not respond to a trial of the lower dose. -

Antioxidative and Neuroprotective Effects of Leea Macrophylla
Ferdousy et al. Clinical Phytoscience (2016) 2:17 DOI 10.1186/s40816-016-0031-6 ORIGINAL CONTRIBUTION Open Access Antioxidative and neuroprotective effects of Leea macrophylla methanol root extracts on diazepam-induced memory impairment in amnesic Wistar albino rat Sakia Ferdousy1, Md Atiar Rahman1*, Md Mamun Al-Amin2, Jannatul Aklima1 and J. M. Kamirul Hasan Chowdhury1 Abstract Background: A neurological disorder is becoming one of the major health problems worldwide. Synthetic drugs for neurological disorders often produce unwanted effects while traditional plant- derived drugs offer a unique strategy in combating the neurological diseases. This study investigated how the antioxidative properties of Leea macrophylla root extracts integratively help as neuroprotective and antiamnesic in animal model. Methods: Leea macrophylla root methanol extract (LM) was assessed by open field test, hole cross test, elevated plus maze test and thiopental sodium induced sleeping time test for screening neuropharmacological effect on Wistar albino rats using the LM at 100 & 200 mg/kg body weight. Antiamnesic effect of LM was studied on diazepam induced anterograde amnesia in Wistar albino rats. Morris water maze test was performed to evaluate whether the learning and memory of rats are impaired by amnesia produced by diazepam. The antioxidative enzymes superoxide dismutase, catalase, glutathione peroxidase and oxidative biomarkers malondialdehyde, nitric oxide, advanced oxidation protein product from the hippocampus of decapitated animals were measured to assess the antioxidative potential of the extract. Results: LM was found to show significant (p <0.05) reduction in locomotor activity and increase in the duration of sleeping of animals. Morris water maze test showed that animals treated with LM significantly (p <0.05) decreased the mean escape latency compared to animals in diazepam group.