Tinea Capitis Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Estimated Burden of Serious Fungal Infections in Ghana
Journal of Fungi Article Estimated Burden of Serious Fungal Infections in Ghana Bright K. Ocansey 1, George A. Pesewu 2,*, Francis S. Codjoe 2, Samuel Osei-Djarbeng 3, Patrick K. Feglo 4 and David W. Denning 5 1 Laboratory Unit, New Hope Specialist Hospital, Aflao 00233, Ghana; [email protected] 2 Department of Medical Laboratory Sciences, School of Biomedical and Allied Health Sciences, College of Health Sciences, University of Ghana, P.O. Box KB-143, Korle-Bu, Accra 00233, Ghana; [email protected] 3 Department of Pharmaceutical Sciences, Faculty of Health Sciences, Kumasi Technical University, P.O. Box 854, Kumasi 00233, Ghana; [email protected] 4 Department of Clinical Microbiology, School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi 00233, Ghana; [email protected] 5 National Aspergillosis Centre, Wythenshawe Hospital and the University of Manchester, Manchester M23 9LT, UK; [email protected] * Correspondence: [email protected] or [email protected] or [email protected]; Tel.: +233-277-301-300; Fax: +233-240-190-737 Received: 5 March 2019; Accepted: 14 April 2019; Published: 11 May 2019 Abstract: Fungal infections are increasingly becoming common and yet often neglected in developing countries. Information on the burden of these infections is important for improved patient outcomes. The burden of serious fungal infections in Ghana is unknown. We aimed to estimate this burden. Using local, regional, or global data and estimates of population and at-risk groups, deterministic modelling was employed to estimate national incidence or prevalence. Our study revealed that about 4% of Ghanaians suffer from serious fungal infections yearly, with over 35,000 affected by life-threatening invasive fungal infections. -

Fungal Infections from Human and Animal Contact
Journal of Patient-Centered Research and Reviews Volume 4 Issue 2 Article 4 4-25-2017 Fungal Infections From Human and Animal Contact Dennis J. Baumgardner Follow this and additional works at: https://aurora.org/jpcrr Part of the Bacterial Infections and Mycoses Commons, Infectious Disease Commons, and the Skin and Connective Tissue Diseases Commons Recommended Citation Baumgardner DJ. Fungal infections from human and animal contact. J Patient Cent Res Rev. 2017;4:78-89. doi: 10.17294/2330-0698.1418 Published quarterly by Midwest-based health system Advocate Aurora Health and indexed in PubMed Central, the Journal of Patient-Centered Research and Reviews (JPCRR) is an open access, peer-reviewed medical journal focused on disseminating scholarly works devoted to improving patient-centered care practices, health outcomes, and the patient experience. REVIEW Fungal Infections From Human and Animal Contact Dennis J. Baumgardner, MD Aurora University of Wisconsin Medical Group, Aurora Health Care, Milwaukee, WI; Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, WI; Center for Urban Population Health, Milwaukee, WI Abstract Fungal infections in humans resulting from human or animal contact are relatively uncommon, but they include a significant proportion of dermatophyte infections. Some of the most commonly encountered diseases of the integument are dermatomycoses. Human or animal contact may be the source of all types of tinea infections, occasional candidal infections, and some other types of superficial or deep fungal infections. This narrative review focuses on the epidemiology, clinical features, diagnosis and treatment of anthropophilic dermatophyte infections primarily found in North America. -

Ringworm & Other Human Fungal Infections
Ringworm & Other Human Fungal Infections McKenzie Pediatrics Ringworm, medically known as Tinea Corporis, is a common skin infection of childhood, and is not caused by a worm at all, but rather by a fungus. It is usually easily treated, and should not be seen as a source of social stigma. It is just one of many types of Tinea infections that affect humans. Tinea is a widespread group of fungal infections caused by dermatophytes. It is second to acne as the most frequently reported skin disease in the United States. Infection may occur through contact with infected humans (by way of shared combs, brushes, hats, pillows, clothing, or bedding) and animals (especially dogs and cats), soil, or inanimate objects. Tinea should be suspected in any red, scaly, itchy, and enlarging rash. Tinea is a superficial infection of the skin (Tinea Corporis), scalp (Tinea Capitis), nails (Tinea Unguium), groin (Tinea Cruris), hands (Tinea Manuum) or feet (Tinea Pedis). There are three types and 27 varieties of dermatophytes that cause human Tinea: Trichophyton, Epidermophyton, and Microsporum. Tinea Corporis (Ringworm) causes smooth and bare skin, typically surrounded by a raised, red, scaly “ring”. Lesions are often solitary, though may be multiple, and even overlapping. It is not nearly as common as what it is most often mistaken for: nummular eczema, a variety of eczema that causes round or oval scaly patches but without a clear area in the center. Nummular eczema tends to be more numerous, and is often less itchy than Ringworm. Topical treatments that are available over-the-counter usually work quite well for Tinea Corporis. -

Diagnosis and Treatment of Tinea Versicolor Ronald Savin, MD New Haven, Connecticut
■ CLINICAL REVIEW Diagnosis and Treatment of Tinea Versicolor Ronald Savin, MD New Haven, Connecticut Tinea versicolor (pityriasis versicolor) is a common imidazole, has been used for years both orally and top superficial fungal infection of the stratum corneum. ically with great success, although it has not been Caused by the fungus Malassezia furfur, this chronical approved by the Food and Drug Administration for the ly recurring disease is most prevalent in the tropics but indication of tinea versicolor. Newer derivatives, such is also common in temperate climates. Treatments are as fluconazole and itraconazole, have recently been available and cure rates are high, although recurrences introduced. Side effects associated with these triazoles are common. Traditional topical agents such as seleni tend to be minor and low in incidence. Except for keto um sulfide are effective, but recurrence following treat conazole, oral antifungals carry a low risk of hepato- ment with these agents is likely and often rapid. toxicity. Currently, therapeutic interest is focused on synthetic Key Words: Tinea versicolor; pityriasis versicolor; anti “-azole” antifungal drugs, which interfere with the sterol fungal agents. metabolism of the infectious agent. Ketoconazole, an (J Fam Pract 1996; 43:127-132) ormal skin flora includes two morpho than formerly thought. In one study, children under logically discrete lipophilic yeasts: a age 14 represented nearly 5% of confirmed cases spherical form, Pityrosporum orbicu- of the disease.3 In many of these cases, the face lare, and an ovoid form, Pityrosporum was involved, a rare manifestation of the disease in ovale. Whether these are separate enti adults.1 The condition is most prevalent in tropical tiesN or different morphologic forms in the cell and semitropical areas, where up to 40% of some cycle of the same organism remains unclear.: In the populations are affected. -

(Sporanox Capsules) 280-A
PRIOR AUTHORIZATION CRITERIA BRAND NAME (generic) SPORANOX ORAL CAPSULES (itraconazole) Status: CVS Caremark Criteria Type: Initial Prior Authorization Policy FDA-APPROVED INDICATIONS Sporanox (itraconazole) Capsules are indicated for the treatment of the following fungal infections in immunocompromised and non-immunocompromised patients: 1. Blastomycosis, pulmonary and extrapulmonary 2. Histoplasmosis, including chronic cavitary pulmonary disease and disseminated, non-meningeal histoplasmosis, and 3. Aspergillosis, pulmonary and extrapulmonary, in patients who are intolerant of or who are refractory to amphotericin B therapy. Specimens for fungal cultures and other relevant laboratory studies (wet mount, histopathology, serology) should be obtained before therapy to isolate and identify causative organisms. Therapy may be instituted before the results of the cultures and other laboratory studies are known; however, once these results become available, antiinfective therapy should be adjusted accordingly. Sporanox Capsules are also indicated for the treatment of the following fungal infections in non-immunocompromised patients: 1. Onychomycosis of the toenail, with or without fingernail involvement, due to dermatophytes (tinea unguium), and 2. Onychomycosis of the fingernail due to dermatophytes (tinea unguium). Prior to initiating treatment, appropriate nail specimens for laboratory testing (KOH preparation, fungal culture, or nail biopsy) should be obtained to confirm the diagnosis of onychomycosis. Compendial Uses Coccidioidomycosis2,3 -

Tinea Capitis 2014 L.C
BJD GUIDELINES British Journal of Dermatology British Association of Dermatologists’ guidelines for the management of tinea capitis 2014 L.C. Fuller,1 R.C. Barton,2 M.F. Mohd Mustapa,3 L.E. Proudfoot,4 S.P. Punjabi5 and E.M. Higgins6 1Department of Dermatology, Chelsea & Westminster Hospital, Fulham Road, London SW10 9NH, U.K. 2Department of Microbiology, Leeds General Infirmary, Leeds LS1 3EX, U.K. 3British Association of Dermatologists, Willan House, 4 Fitzroy Square, London W1T 5HQ, U.K. 4St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust, St Thomas’ Hospital, Westminster Bridge Road, London SE1 7EH, U.K. 5Department of Dermatology, Hammersmith Hospital, 150 Du Cane Road, London W12 0HS, U.K. 6Department of Dermatology, King’s College Hospital, Denmark Hill, London SE5 9RS, U.K. 1.0 Purpose and scope Correspondence Claire Fuller. The overall objective of this guideline is to provide up-to- E-mail: [email protected] date, evidence-based recommendations for the management of tinea capitis. This document aims to update and expand Accepted for publication on the previous guidelines by (i) offering an appraisal of 8 June 2014 all relevant literature since January 1999, focusing on any key developments; (ii) addressing important, practical clini- Funding sources cal questions relating to the primary guideline objective, i.e. None. accurate diagnosis and identification of cases; suitable treat- ment to minimize duration of disease, discomfort and scar- Conflicts of interest ring; and limiting spread among other members of the L.C.F. has received sponsorship to attend conferences from Almirall, Janssen and LEO Pharma (nonspecific); has acted as a consultant for Alliance Pharma (nonspe- community; (iii) providing guideline recommendations and, cific); and has legal representation for L’Oreal U.K. -

Tinea Capitis: Unusual Chronic Presentation in an Elderly Woman
ISSN: 2474-3658 Salazar et al. J Infect Dis Epidemiol 2018, 4:048 DOI: 10.23937/2474-3658/1510048 Volume 4 | Issue 1 Journal of Open Access Infectious Diseases and Epidemiology CASE REPORT Tinea Capitis: Unusual Chronic Presentation in an Elderly Woman Elizabeth Salazar1*, Daniel Asz-Sigall2, Diana Vega3 and Roberto Arenas4 1Dermato-Oncologist, Private Practice, Mexico City, Mexico 2 Check for Dermatologist, Dermato-Oncology and Trichology Clinic, National University of Mexico, Mexico City, Mexico updates 3Mycologist, Mycology Section, Hospital General “Dr. Manuel Gea González”, Mexico City, Mexico 4Dermatologist and Mycologist, Mycology Section, General Hospital “Dr. Manuel Gea González”, Mexico City, Mexico *Corresponding authors: Elizabeth Salazar, Dermato-Oncologist, Private Practice, Mexico City, Mexico, E-mail: dra. [email protected] The non-inflammatory clinical presentation can be Abstract found in 90% of affected children. It is more frequent in Tinea capitis is a superficial fungal infection of the scalp tropical regions with low socioeconomic conditions and and hair caused by dermatophytes such as Trichophyton and Microsporum. Tinea capitis is very rare in adults, and affects almost exclusively children (98%). The inflamma- may affect those with immunosuppressive diseases or tory form is observed only in 10% and most commonly menopausal elderly women. Clinical manifestations along seen in prepubescent children. Tinea capitis is caused with trichoscopy and Wood’s light, can help the clinician to by dermatophytes that use keratin as a nutrient source. determine the correct diagnosis, in order to reduce irrevers- Scalp erythema, scaling, and crusting are typical signs of ible sequelae and decrease multiple contagion. KOH direct exam and culture confirm diagnosis and aetiology. -

Geophilic Dermatophytes and Other Keratinophilic Fungi in the Nests of Wetland Birds
ACTA MyCoLoGICA Vol. 46 (1): 83–107 2011 Geophilic dermatophytes and other keratinophilic fungi in the nests of wetland birds Teresa KoRnIŁŁoWICz-Kowalska1, IGnacy KIToWSKI2 and HELEnA IGLIK1 1Department of Environmental Microbiology, Mycological Laboratory University of Life Sciences in Lublin Leszczyńskiego 7, PL-20-069 Lublin, [email protected] 2Department of zoology, University of Life Sciences in Lublin, Akademicka 13 PL-20-950 Lublin, [email protected] Korniłłowicz-Kowalska T., Kitowski I., Iglik H.: Geophilic dermatophytes and other keratinophilic fungi in the nests of wetland birds. Acta Mycol. 46 (1): 83–107, 2011. The frequency and species diversity of keratinophilic fungi in 38 nests of nine species of wetland birds were examined. nine species of geophilic dermatophytes and 13 Chrysosporium species were recorded. Ch. keratinophilum, which together with its teleomorph (Aphanoascus fulvescens) represented 53% of the keratinolytic mycobiota of the nests, was the most frequently observed species. Chrysosporium tropicum, Trichophyton terrestre and Microsporum gypseum populations were less widespread. The distribution of individual populations was not uniform and depended on physical and chemical properties of the nests (humidity, pH). Key words: Ascomycota, mitosporic fungi, Chrysosporium, occurrence, distribution INTRODUCTION Geophilic dermatophytes and species representing the Chrysosporium group (an arbitrary term) related to them are ecologically classified as keratinophilic fungi. Ke- ratinophilic fungi colonise keratin matter (feathers, hair, etc., animal remains) in the soil, on soil surface and in other natural environments. They are keratinolytic fungi physiologically specialised in decomposing native keratin. They fully solubilise na- tive keratin (chicken feathers) used as the only source of carbon and energy in liquid cultures after 70 to 126 days of growth (20°C) (Korniłłowicz-Kowalska 1997). -
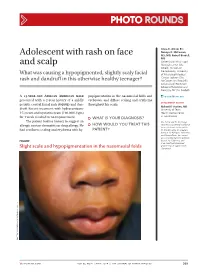
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Tinea Capitis
BCCH Pediatric Dermatology Clinic Joseph M Lam, MD TINEA CAPITIS What is tinea capitis? Treatment Tinea capitis (also called “ringworm of the scalp) is the most Even though the scale is seen on common fungus infection in children, and usually affects the surface of the scalp, the infection goes deep to the root children from 2 to 10 years of age. Fewer than 5 percent of of the hair, under the skin. cases of ringworm of the scalp occur in adults. Most cases of Because of this, just using creams ringworm involving the scalp are due to a fungus that is or shampoos will not clear the passed from person to person, although pets can also pass on infection. the fungus. 1.Terbinafine (pill for scalp The fungal infection can begin fungus) as dandruff, areas of baldness, A pill needs to be taken once a day for about 4 weeks to clear or areas of redness on the scalp the fungus infection. Based on with swelling and pus bumps. your child’s weight, it will be either 1/2, 3/4 or a full pill. Even In some cases, big bumps if the scalp looks better, you (lymph nodes) in the neck may need to take the medicine until Scaly areas of hair loss finished. Unfortunately, there is be felt. no liquid version of terbinafine in The diagnosis of fungus infection is suspected by the Canada. appearance of the scalp and can be verified by fungal 2.Medicated shampoos cultures. The fungal culture usually grows the fungus in four Even though a medicated weeks. -
Ringworm of the Scalp (Tinea Capitis) N
n Ringworm of the Scalp (Tinea Capitis) n Can ringworm of the scalp Ringworm is infection with certain types of fungi called dermatophytes. The name comes from the be prevented? distinct, circle-shaped rash formed when the in- There are some things you can do to help prevent ring- fection involves the skin. When ringworm infects worm of the scalp. However, the infection is difficult to pre- the scalp and hair, it can look several different ways. vent because it is easily passed from person to person—for The scalp can look scaly (like dandruff) and have example, children playing together. (See under “How is bald spots or sores. Treatment with antifungal ringworm of the scalp treated?”) medications is effective. If bald patches are pres- Family members and other people with whom your child ent, the hair will usually grow back once the infec- has been in contact should be checked for infection. Other tion is eliminated. family members, including adults, can carry the infection without having any symptoms. They can be treated with medicated shampoo, as described later. What is ringworm of the scalp? How is ringworm of the Ringworm of the scalp is a common infection caused by scalp diagnosed? certain fungi called dermatophytes. Ringworm of the scalp is also called “tinea capitis.” Dermatophytes also cause infec- The doctor often suspects the diagnosis from the appear- tions of the feet (athlete’s foot) or groin (jock itch). Ring- ance of the rash on the scalp. However, it may be worm of the scalp is most common in young children, confused with other conditions, such as dandruff. -

Epidemiology of Superficial Fungal Diseases in French Guiana: a Three
Medical Mycology August 2011, 49, 608–611 Epidemiology of superfi cial fungal diseases in French Guiana: a three-year retrospective analysis CHRISTINE SIMONNET * , FRANCK BERGER * & JEAN-CHARLES GANTIER † * Institut Pasteur de la Guyane , Cayenne , France , and † Institut Pasteur , Paris , France A three-year retrospective analysis of fungi isolated from specimens of patients with superfi cial fungal infections in French Guiana is presented. Clinical samples from 726 Downloaded from https://academic.oup.com/mmy/article/49/6/608/972117 by guest on 27 September 2021 patients with presumptive diagnoses of onychomycosis (28.2% of the patients), tinea capitis (27.8%), superfi cial cutaneous mycoses of the feet (22.0%), and of other areas of the body (21.9%), were assessed by microscopic examination and culture. Dermato- phytes accounted for 59.2% of the isolates, followed by yeasts (27.5%) and non-der- matophytic molds (13.1%). Trichophyton rubrum was the most common dermatophyte recovered from cases of onychomycosis (67.4%), tinea pedis (70.6%) and tinea corporis (52.4%). In contrast, Trichophyton tonsurans was the predominant species associated with tinea capitis (73.9%). Yeasts were identifi ed as the principal etiologic agents of onychomycosis of the fi ngernails (74.2%), whereas molds were found mainly in cases of onychomycosis of the toenails. In such instances, Neo s cytalidium dimidiatum (70.8%) was the most common mold recovered in culture. In conclusion, the prevalence of T. rubrum and the occurrence of onychomycosis and fungal infections of the feet in French Guiana are similar to results reported from Europe, whereas the frequency of tinea capi- tis and the importance of T.