Patient-Monitoring Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dec 3 1 2013
X 133704. DEC 3 1 2013 510(K) Summary for M1 Capnography Mask 1. Submission Sponsor Monitor Mask, Inc. 551543 dAvenue NE Seattle WA, 98105 USA Phone: 877.226.1776 Contact: JW Beard MD, MBA, Founder and CEO 2. Submission Correspondent Emergo, Group, Inc. 816 Congress Avenue, Suite 1400 Austin, TX 78701 office Phone: (512) 327.9997 Fax: (512) 327.9998 Contact: Stuart RGoldman, Senior Consultant, RA/QA Email: oroiect.manapement~emerpogroup.com 3. Date Prepared September 20, 2013 4. Device Identification Trade/Proprietary Name: M1 Capnography Mask Common/Usual Name: oxygen/capnography mask Classification Name: analyzer, gas, carbon-dioxide, gaseous-phase Classification Regulation: §868.1400 Product Code: CCK (primary); BYG (secondary) Device Class: Class 11 Classification Panel: Anesthesiology 5. Legally Marketed Predicate Device CapnoxygenO Mask (K(971229) manufactured by Medlsys (Southmedic) 6. Device Description The M1 Capnography Mask is connected to a gas source for delivering low flow oxygen through flexible tubing to the patient, and at the same time provides a means to attach a capnograph for monitoring exhaled carbon dioxide during nose and mouth breathing. The capnograph gas sample tube attaches to a standard female Luer connector on either the left or right side of the M1 Capnography Mask. The M1 Capnography Mask will initially be made available in only one size, adult large (Model #001). Page 5-1 7. Indication for Use Statement The M1 Capnography Mask is a single-use device intended for delivering supplemental oxygen and monitoring exhaled carbon dioxide in non-intubated spontaneously breathing patients. Standard oxygen tubing and two female Luer ports for gas sample line attachment are included. -

Capnography 101 Oxygenation and Ventilation
It’s Time to Start Using it! Capnography 101 Oxygenation and Ventilation What is the difference? Oxygenation and Ventilation Ventilation O Oxygenation (capnography) 2 (oximetry) CO Cellular 2 Metabolism Capnographic Waveform • Capnograph detects only CO2 from ventilation • No CO2 present during inspiration – Baseline is normally zero CD AB E Baseline Capnogram Phase I Dead Space Ventilation • Beginning of exhalation • No CO2 present • Air from trachea, posterior pharynx, mouth and nose – No gas exchange occurs there – Called “dead space” Capnogram Phase I Baseline A B I Baseline Beginning of exhalation Capnogram Phase II Ascending Phase • CO2 from the alveoli begins to reach the upper airway and mix with the dead space air – Causes a rapid rise in the amount of CO2 • CO2 now present and detected in exhaled air Alveoli Capnogram Phase II Ascending Phase C Ascending II Phase Early A B Exhalation CO2 present and increasing in exhaled air Capnogram Phase III Alveolar Plateau • CO2 rich alveolar gas now constitutes the majority of the exhaled air • Uniform concentration of CO2 from alveoli to nose/mouth Capnogram Phase III Alveolar Plateau Alveolar Plateau CD III AB CO2 exhalation wave plateaus Capnogram Phase III End-Tidal • End of exhalation contains the highest concentration of CO2 – The “end-tidal CO2” – The number seen on your monitor • Normal EtCO2 is 35-45mmHg Capnogram Phase III End-Tidal End-tidal C D AB End of the the wave of exhalation Capnogram Phase IV Descending Phase • Inhalation begins • Oxygen fills airway • CO2 level quickly -

Serious Adverse Event Reporting Under Directives 90/385/Eec and 93/42/Eec
EUROPEAN COMMISSION DG Internal Market, Industry, Entrepreneurship and SMEs Consumer, Environmental and Health Technologies Health technology and Cosmetics MEDDEV 2.7/3 revision 3 May 2015 GUIDELINES ON MEDICAL DEVICES CLINICAL INVESTIGATIONS: SERIOUS ADVERSE EVENT REPORTING UNDER DIRECTIVES 90/385/EEC AND 93/42/EEC. Note The present Guidelines are part of a set of Guidelines relating to questions of application of EC-Directives on medical Devices. They are legally not binding. The Guidelines have been carefully drafted through a process of intensive consultation of the various interested parties (competent authorities, Commission services, industries, other interested parties) during which intermediate drafts where circulated and comments were taken up in the document. Therefore, this document reflects positions taken by representatives of interest parties in the medical devices sector. These guidelines incorporate changes introduced by Directive 2007/47/EC amending Council Directive 90/385/EEC and Council Directive 93/42/EEC. 1 MEDICAL DEVICES DIRECTIVES CLINICAL INVESTIGATION GUIDELINES FOR ADVERSE EVENT REPORTING UNDER DIRECTIVES 90/385/EEC AND 93/42/EEC Index 1. INTRODUCTION 2. SCOPE 3. DEFINITIONS 4. REPORTABLE EVENTS 5. REPORT BY WHOM 6. REPORT TO WHOM 7. REPORTING TIMELINES 8. CAUSALITY ASSESSMENT 9. REPORTING FORM Appendix – Summary Reporting Form 2 1. INTRODUCTION This guidance defines Serious Adverse Event (SAE) reporting modalities and includes a summary tabulation reporting format. Individual reporting should be performed in accordance with national requirements. The objective of this guidance is to contribute to the notification of SAEs to all concerned National Competent Authorities (NCAs ) 1 in the context of clinical investigations in line with the requirements of Annex 7 of Directive 90/385/EEC and Annex X of Directive 93/42/EEC, as amended by Directive 2007/47/EC. -

Monitoring Anesthetic Depth
ANESTHETIC MONITORING Lyon Lee DVM PhD DACVA MONITORING ANESTHETIC DEPTH • The central nervous system is progressively depressed under general anesthesia. • Different stages of anesthesia will accompany different physiological reflexes and responses (see table below, Guedel’s signs and stages). Table 1. Guedel’s (1937) Signs and Stages of Anesthesia based on ‘Ether’ anesthesia in cats. Stages Description 1 Inducement, excitement, pupils constricted, voluntary struggling Obtunded reflexes, pupil diameters start to dilate, still excited, 2 involuntary struggling 3 Planes There are three planes- light, medium, and deep More decreased reflexes, pupils constricted, brisk palpebral reflex, Light corneal reflex, absence of swallowing reflex, lacrimation still present, no involuntary muscle movement. Ideal plane for most invasive procedures, pupils dilated, loss of pain, Medium loss of palpebral reflex, corneal reflexes present. Respiratory depression, severe muscle relaxation, bradycardia, no Deep (early overdose) reflexes (palpebral, corneal), pupils dilated Very deep anesthesia. Respiration ceases, cardiovascular function 4 depresses and death ensues immediately. • Due to arrival of newer inhalation anesthetics and concurrent use of injectable anesthetics and neuromuscular blockers the above classic signs do not fit well in most circumstances. • Modern concept has two stages simply dividing it into ‘awake’ and ‘unconscious’. • One should recognize and familiarize the reflexes with different physiologic signs to avoid any untoward side effects and complications • The system must be continuously monitored, and not neglected in favor of other signs of anesthesia. • Take all the information into account, not just one sign of anesthetic depth. • A major problem faced by all anesthetists is to avoid both ‘too light’ anesthesia with the risk of sudden violent movement and the dangerous ‘too deep’ anesthesia stage. -
Medical Device Software Regulation Software Qualification And
AHWP/WG1/R001:2014 REFERENCE DOCUMENT (DRAFT for Public Comments) Title: White Paper on Medical Device Software Regulation – Software Qualification and Classification Author: Work Group 1, Pre-Market Submission and CSDT Date 22 May 2014 Copyright © 2014 by the Asian Harmonization Working Party Table of Contents 1. Introduction ............................................................................................................................. 2 2. Definitions ................................................................................................................................ 2 3. Types of Software that are Regulated as Medical Devices ........................................... 4 4. Forms of Medical Device Software .................................................................................... 4 5. SaMD Medical Device Software Classification Globally .............................................. 6 5.1. International Medical Device Regulatory Forum (IMDRF) .................................... 6 5.1.1. IMDRF qualification criteria .......................................................................................... 6 5.2. Australia TGA ..................................................................................................................... 7 5.2.2. Risk classification of software in TGA ...................................................................... 7 5.3. China .................................................................................................................................... -

Ministry of Medical Services Pharmacy and Poisons Board Kenya
MINISTRY OF MEDICAL SERVICES PHARMACY AND POISONS BOARD KENYA GUIDELINES ON SUBMISSION OF DOCUMENTATION FOR REGISTRATION OF MEDICAL DEVICES FIRST EDITION September, 2011 ACKNOWLEDGEMENTS PREFACE Medical Device Regulation in Kenya will be supervised and directed by Kenya Pharmacy and Poisons Board (PPB). Classification, requirements and evaluation of Medical Devices will be mainly simulation of rules and regulations recognized by the international regulatory benchmarks, which are mainly: a. The Pharmacy and Poisons Act Chapter 244 of 2002 b. Global Harmonization Task Force (GHTF) for Medical Device c. EU Medical Device Directives 93/42/EEC, EU In Vitro Diagnostic Device Directive Ministry of Medical Services Page 2 of 2 Pharmacy and Poisons Board Kenya (IVDD) 98/79/EC and EU Active Implantable Medical Device Directive (AIMDD) 90/385/EEC. d. US FDA (United States Food & Drug Administration) e. Australia TGA (Therapeutics Goods Act) The regulation of medical devices in Kenya is aimed at maintaining balance between ensuring product safety, quality and effectiveness and providing the public with timely access to medical devices and preventing the entrance of unsafe or ineffective devices into the market. SCOPE These guidelines shall apply to medical devices and their accessories. For the purposes of these guidelines, accessories shall be treated as medical devices in their own right. Where a device is intended to administer a medicinal product, that device shall be governed by this guideline, without prejudice to the corresponding regulations for registration of medicinal products for human use set by the PPB. If, however, such a device is placed on the market in such a way that the device and the medicinal product form a single integral product which is intended exclusively for use in the given combination and which is not reusable, that single product shall be governed by corresponding regulations for registration of medicinal products for human use set by the PPB. -

Data Protection on Pharmacovigilance and Medical Device Safety
DATA PROTECTION ON PHARMACOVIGILANCE AND MEDICAL DEVICE SAFETY General Galena Pharma Oy, founded in 1996, is a pharmaceutical company specialising in contract manufacturing and packaging. A significant part of the service includes product development, registration & marketing authorization and post-market surveillance. The wide range of our products comprises human and veterinary medicinal products, medical devices in Classes IIa and IIb, cosmetics, food supplements, animal care products and nutritional supplements. The products we manufacture are sold mainly in pharmacies. Galena Pharma has a legal obligation to monitor the adverse events and the effects of their products in the countries where they are getting sold and carry out a continuous risk-benefit assessment. It is called pharmacovigilance and medical device safety operation. With the help of this system and quality assurance management, Galena Pharma can manage adverse events and protect public health. Thanks to this, the safety of Galena Pharma's products is guaranteed. It is the responsibility of the competent authority to inspect and evaluate the pharmacovigilance and medical device safety activities of the company and validate it. Pharmacovigilance and medical device safety obligate Galena Pharma to process the information of the patient and/or the notifier of the adverse reaction, based on which a person can be directly or indirectly identified. These are personal data whose processing is mandatory for Galena Pharma in order to comply with its pharmacovigilance and medical device safety obligations and report any adverse reactions or events that come to their notice to the competent authorities in a relevant and appropriate manner. This privacy statement describes how personal data gets processed for pharmacovigilance and medical device safety purposes under applicable data protection laws and the obligations set out in the EU Data Protection Regulation (EU 2016/679). -

Air & Surface Transport Nurses Association Position Statement
Air & Surface Transport Nurses Association Position Statement Advanced Airway Management Background In the early 1970s, civilian flight nursing became a recognized nursing specialty and an integral element in the care of critically ill and injured patients. Advanced airway management is an essential procedure in meeting those patient care goals. The procedure can be performed safely and effectively by properly trained transport teams; however, it is not without risks and complications. Individual state Boards of Nursing regulate registered nursing licensure. ASTNA believes transport providers and teams must work collegially and collaboratively with these regulatory bodies. Registered nurses who perform advanced airway management provide care under the direction and protocols of their medical directors. In addition, Registered Nurses who perform advanced airway management skills must have comprehensive initial and ongoing education to optimize clinical knowledge, skill, and decision-making ability. Education programs teaching these advanced airway management skills should include at least the following components: • Comprehensive review of airway/respiratory anatomy and physiology • Basic airway skills and techniques • Clinical assessment skills to evaluate the need for escalated intervention • Extraglottic airway devices • Tracheal intubation using a variety of devices • Surgical airway techniques • Pharmacology and clinical application of sedative, analgesic, hypnotic, and neuromuscular blocking agents used in advanced airway management • Patient safety monitoring equipment, including continuous pulse oximetry, continuous heart rate, and continuous monitoring of waveform capnography • Teamwork and crisis resource management, as applied to the clinical environment both as team leaders and team members Clinical best practices evolve continuously.1 Transport programs performing advanced airway should adopt policies that ensure clinical education and practice components remain current. -
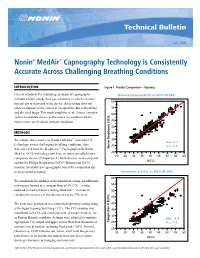
Nonin® Medair™ Capnography Technology Is Consistently Accurate Across Challenging Breathing Conditions
Technical Bulletin July 2009 Nonin® MedAir™ Capnography Technology is Consistently Accurate Across Challenging Breathing Conditions INTRODUCTION Figure 1: Product Comparison – Accuracy Current standards for evaluating accuracy of capnographs NoninNonin RespSense RespSense EtCOEtCO2 vs NICONICO (N-364)(N=364) includes simple, steady flow gas validation in which a known 60 percent gas is delivered to the device. Such testing does not allow evaluation of the effects of complexities due to breathing 55 and diseased lungs. This study sought to create a more complex 2 50 system to evaluate device performance in conditions which better represented realistic patient conditions. 45 40 METHODS 35 Resp EtCO2 To evaluate the accuracy of Nonin’s MedAir™ end-tidal CO 30 2 Bias: 0.2 technology across challenging breathing conditions, data 25 Arms: 2.6 was collected from the RespSense™ Capnograph with Nonin Nonin RespSense EtCO 20 MedAir EtCO2 technology and from an internationally known 20 25 30 35 40 45 50 55 60 competitor device (Competitor A). Both devices were compared ® NICO against the Philips Respironics NICO Mainstream EtCO2 monitor, a mainstream capnograph chosen for comparison due Root Mean Square Error 2.563916 Mean of Response 0.178683 to its accepted accuracy. CompetitorNellcor EtCO A EtCO2 vs2 NICOvs NICO (N=364) (N-364) 60 To compliment the findings of the simulation testing, an additional 55 test was performed at a constant flow of 5% CO2—a value required in medical device testing standards1—in order to 50 validate the accuracy of the devices at a static CO2 level. 2 45 The tests were performed in a controlled laboratory setting using 40 a Michigan Training Test Lung (TTL). -

An Introduction to Anaesthesia
What You Need to KNoW about An introduction to anaesthesia Introduction divided into three stages: induction, main- n Central neuraxial block, e.g. spinal or Anaesthetic experience in the undergradu- tenance and emergence. epidural (Figure 1 and Table 1). ate timetable is often very limited so it can In regional anaesthesia, nerve transmis- remain somewhat of a mysterious practice sion is blocked, and the patient may stay Components of a general well into specialist training. This introduc- awake or be sedated or anaesthetized dur- anaesthetic tion to the components of an anaesthetic ing a procedure. Techniques used include: A general anaesthetic always involves an will help readers to get more from clinical n Local anaesthetic field block hypnotic agent, usually an analgesic and attachments in surgery and anaesthetics or n Peripheral nerve block may also include muscle relaxation. The serve as an introduction to the topic for n Nerve plexus block combination is referred to as the ‘triad of novice or non-anaesthetists. anaesthesia’. Figure 1. Schematic vertical longitudinal section The relative importance of each com- Types and sites of anaesthesia of vertebral column and structures encountered ponent depends on surgical and patient The term anaesthesia comes from the when performing central neuraxial blocks. * factors: the intervention planned, site, Greek meaning loss of sensation. negative pressure space filled with fat and surgical access requirement and the Anaesthetic practice has evolved from a venous plexi. † extends to S2, containing degree of pain or stimulation anticipated. need for pain relief and altered conscious- arachnoid mater, CSF, pia mater, spinal cord The technique is tailored to the individu- ness to allow surgery. -

Inpatient Sepsis Management
Inpatient Sepsis Management - Adult Page 1 of 6 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PRESENTATION EVALUATION TREATMENT Call Code Blue Team1 Patient exhibits at least two of the Yes following modified SIRS criteria: ● Temperature < 36 or > 38.4°C Is patient ● MERIT team1 to evaluate and notify Primary MD/APP STAT ● Heart rate > 110 bpm unresponsive? ● Prepare transfer to ICU See Page 2: Sepsis ● Respiratory rate > 24 bpm ● Assess for presence of infection (see Appendix A) Management ● WBC count < 3 or > 15 K/microliter ● Assess for organ dysfunction (see Appendix B) No Yes ● Primary team to consider goals of care discussion if appropriate Is 1,2 the patient ● Sepsis APP to notify unstable? Primary MD/APP 1,2 ● Sepsis APP to evaluate ● See Page 2: Sepsis No ● Assess for presence of infection (see Yes Management Appendix A) Sepsis? ● Assess for organ dysfunction (see ● For further work up, Appendix B) No initiate Early Sepsis Order Set ● Follow up evaluation by SIRS = systemic inflammatory response syndrome Primary Team APP = advanced practice provider 1 For patients in the Acute Cancer -
Adequate Interval for the Monitoring of Vital Signs During Endotracheal Intubation J.Y
Min et al. BMC Anesthesiology (2017) 17:110 DOI 10.1186/s12871-017-0399-y RESEARCHARTICLE Open Access Adequate interval for the monitoring of vital signs during endotracheal intubation J.Y. Min1, H.I. Kim1, S.J Park1, H. Lim2, J.H. Song2 and H. J. Byon1* Abstract Background: In the perioperative period, it may be inappropriate to monitor vital signs during endotracheal intubation using the same interval as during a hemodynamically stable period. The aim of the present study was to determine whether it is appropriate to use the same intervals used during the endotracheal intubation and stable periods to monitor vital signs of patients under general anesthesia. Methods: The mean arterial pressure (MAP) and heart rate (HR) were continuously measured during endotracheal intubation (15 min after intubation) and hemodynamically stable (15 min before skin incision) periods in 24 general anesthesia patients. Data was considered “unrecognized” when continuously measured values were 30% more or less than the monitored value measured at 5- or 2.5-min intervals. The incidence of unrecognized data during endotracheal intubation was compared to that during the hemodynamically stable period. Result: ThereweresignificantlymoreunrecognizedMAPdatameasured at 5-min intervals during endotracheal intubation than during the hemodynamically stable period (p value <0.05). However, there was no difference in the incidence of unrecognized MAP data at 2.5 min intervals or HR data at 5 or 2.5 min intervals between during the endotracheal intubation and hemodynamically stable periods. Conclusion: A 5-min interval throughout the operation period was not appropriate for monitoring vital signs. Therefore, , a 2.5-min interval is recommended for monitoring the MAP during endotracheal intubation.