Glypressin Ferring Pharmaceuticals Pty Ltd PM-2010-03182-3-3 Final 26 November 2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vasopressin in Pediatric Critical Care
182 Review Article Vasopressin in Pediatric Critical Care Karen Choong1 1 Department of Pediatrics, Critical Care, Epidemiology and Address for correspondence Karen Choong, MB, BCh, MSc, Biostatistics, McMaster University, Hamilton, Ontario, Canada Department of Pediatrics, Critical Care, Epidemiology and Biostatistics, McMaster University, 1280 Main Street West, Room 3E20, J Pediatr Intensive Care 2016;5:182–188. Hamilton, Ontario, Canada L8S4K1 (e-mail: [email protected]). Abstract Vasopressin is a unique hormone with complex receptor physiology and numerous physiologic functions beyond its well-known vascular actions and osmoregulation. While vasopressin has in the past been primarily used in the management of diabetes insipidus and acute gastrointestinal bleeding, an increased understanding of the physiology of refractory shock, and the role of vasopressin in maintaining cardiovascular homeostasis prompted a renewed interest in the therapeutic roles for this hormone in the critical care setting. Identifying vasopressin-deficient individuals for the purposes of assessing responsiveness to exogenous hormone and prognosticating outcome has expanded research into the evaluation of vasopressin and its precursor, copeptin as Keywords useful biomarkers. This review summarizes the current evidence for vasopressin in ► vasopressin critically ill children, with a specific focus on its use in the management of shock. We ► pediatrics outline important considerations and current guidelines, when considering the use of ► shock vasopressin or its -
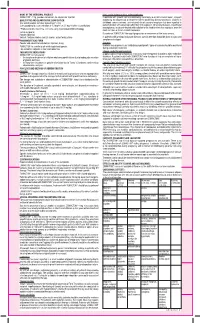
ZOMACTON Powder and Solvent for Solution for Injection 4Mg Package
NAME OF THE MEDICINAL PRODUCT Intra‑cranial lesions or other active neoplasms ZOMACTON® 4 mg, powder and solvent for solution for injection In patients with growth hormone deficiency secondary to an intra‑cranial lesion, frequent QUALITATIVE AND QUANTITATIVE COMPOSITION monitoring for progression or recurrence of the underlying disease process is advised. In One vial of powder contains: Somatropin* 4 mg childhood cancer survivors, an increased risk of a second neoplasm has been reported in (corresponding to a concentration of 1.3 mg/ml or 3.3 mg/ml after reconstitution) patients treated with somatropin after their first neoplasm. Intracranial tumours, in particular meningiomas, in patients treated with radiation to the head for their first neoplasm, were the * Produced in Escherichia coli cells using recombinant DNA technology most common of these second neoplasms. List of excipients: Discontinue ZOMACTON® therapy if progression or recurrence of the lesion occurs. Powder: Mannitol Solvent: Sodium chloride, benzyl alcohol, water for injections In patients with previous malignant diseases special attention should be given to signs and symptoms of relapse. PHARMACEUTICAL FORM Powder and solvent for solution for injection, 4 mg Scoliosis ZOMACTON® is a white to off‑white lyophilised powder. Scoliosis may progress in any child during rapid growth. Signs of scoliosis should be monitored The solvent in ampoule is clear and colourless. during somatropin treatment. THERAPEUTIC INDICATIONS Slipped capital femoral epiphysis ® Slipped capital femoral epiphysis may occur more frequently in patients with endocrine ZOMACTON is indicated for: ® - the long‑term treatment of children who have growth failure due to inadequate secretion disorders. A patient treated with ZOMACTON who develops a limp or complains of hip or of growth hormone knee pain should be evaluated by a physician. -

Largescale Synthesis of Peptides
Lars Andersson1 Lennart Blomberg1 Large-Scale Synthesis of Martin Flegel2 Ludek Lepsa2 Peptides Bo Nilsson1 Michael Verlander3 1 PolyPeptide Laboratories (Sweden) AB, Malmo, Sweden 2 PolyPeptide Laboratories SpoL, Prague, Czech Republic 3 PolyPeptide Laboratories, Inc., Torrance, CA, 90503 USA Abstract: Recent advances in the areas of formulation and delivery have rekindled the interest of the pharmaceutical community in peptides as drug candidates, which, in turn, has provided a challenge to the peptide industry to develop efficient methods for the manufacture of relatively complex peptides on scales of up to metric tons per year. This article focuses on chemical synthesis approaches for peptides, and presents an overview of the methods available and in use currently, together with a discussion of scale-up strategies. Examples of the different methods are discussed, together with solutions to some specific problems encountered during scale-up development. Finally, an overview is presented of issues common to all manufacturing methods, i.e., methods used for the large-scale purification and isolation of final bulk products and regulatory considerations to be addressed during scale-up of processes to commercial levels. © 2000 John Wiley & Sons, Inc. Biopoly 55: 227–250, 2000 Keywords: peptide synthesis; peptides as drug candidates; manufacturing; scale-up strategies INTRODUCTION and plants,5 have all combined to increase the avail- ability and lower the cost of producing peptides. For For almost half a century, since du Vigneaud first many years, however, the major obstacle to the suc- presented his pioneering synthesis of oxytocin to the cess of peptides as pharmaceuticals was their lack of world in 1953,1 the pharmaceutical community has oral bioavailability and, therefore, relatively few pep- been excited about the potential of peptides as “Na- tides reached the marketplace as approved drugs. -
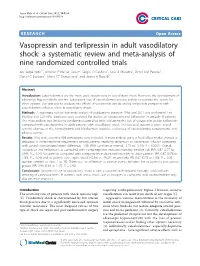
Vasopressin and Terlipressin in Adult Vasodilatory Shock: a Systematic Review and Meta-Analysis of Nine Randomized Controlled Tr
Serpa Neto et al. Critical Care 2012, 16:R154 http://ccforum.com/content/16/4/R154 RESEARCH Open Access Vasopressin and terlipressin in adult vasodilatory shock: a systematic review and meta-analysis of nine randomized controlled trials Ary Serpa Neto1*, Antônio P Nassar Júnior2, Sérgio O Cardoso1, José A Manetta1, Victor GM Pereira1, Daniel C Espósito1, Maria CT Damasceno1 and James A Russell3 Abstract Introduction: Catecholamines are the most used vasopressors in vasodilatory shock. However, the development of adrenergic hyposensitivity and the subsequent loss of catecholamine pressor activity necessitate the search for other options. Our aim was to evaluate the effects of vasopressin and its analog terlipressin compared with catecholamine infusion alone in vasodilatory shock. Methods: A systematic review and meta-analysis of publications between 1966 and 2011 was performed. The Medline and CENTRAL databases were searched for studies on vasopressin and terlipressin in critically ill patients. The meta-analysis was limited to randomized controlled trials evaluating the use of vasopressin and/or terlipressin compared with catecholamine in adult patients with vasodilatory shock. The assessed outcomes were: overall survival, changes in the hemodynamic and biochemical variables, a decrease of catecholamine requirements, and adverse events. Results: Nine trials covering 998 participants were included. A meta-analysis using a fixed-effect model showed a reduction in norepinephrine requirement among patients receiving terlipressin or vasopressin infusion compared with control (standardized mean difference, -1.58 (95% confidence interval, -1.73 to -1.44); P < 0.0001). Overall, vasopressin and terlipressin, as compared with norepinephrine, reduced mortality (relative risk (RR), 0.87 (0.77 to 0.99); P = 0.04). -

Hemmo Pharmaceuticals Private Limited
Global Supplier of Quality Peptide Products Hemmo Pharmaceuticals Private Limited Corporate Presentation Privileged & Confidential Privileged & Confidential Corporate Overview Privileged & Confidential 2 Company at a glance • Commenced operations in 1966 as a Key Highlights trading house, focusing on Oxytocin amongst other products Amongst the largest Indian peptide manufacturing company • In 1979, ventured into manufacturing of Oxytocin Competent team of 154 people including 6 PhDs, 60+ chemistry graduates/post graduates and 3 engineers • Privately held family owned company Portfolio – Generic APIs, Custom Peptides for Research and Clinical Development and Peptide • Infrastructure Fragments − State of art manufacturing facility in Developed 21 generic products in-house. Navi Mumbai, 5 more in progress − R&D facilities at Thane and Spain − Corporate office at Worli First and the only independent Indian company to have a US FDA approved peptide manufacturing site Privileged & Confidential 3 Transition from a trading house to a research based manufacturing facility Commenced Commenced Investment in State of the Art Opened R& D Expanded operations manufacturing greenfield project facility at Navi Centre in manufacturing as a trading of peptides intended for Mumbai Girona,Spain capacity House regulated markets commissioned R&D center set up in Infrastructure Mumbai 1966 1979 2005 2007 2008 2010 2011 2012 2014 2015 Oxytocin Oxytocin Desmopressin Buserelin Triptorelin Goserelin Linaclotide Glatiramer amongst Gonadorelin Decapeptide Cetrorelix -

NDA 22-231 Terlipressin for the Treatment of HRS Type 1
NDA 22-231 Terlipressin for the Treatment of HRS Type 1 Cardiovascular and Renal Drugs Advisory Committee July 15, 2020 CC-1 Introduction Khurram Jamil, MD Khurram Jamil, MD Vice President, Clinical Research in Hepatology Critical Care Division Mallinckrodt CC-2 Hepatorenal Syndrome Type 1 (HRS-1) • Rare condition: estimated US incidence ~ 35,000 • Functional renal failure with structurally normal kidney – Portal hypertension leads to splanchnic vasodilation – Compensatory renal vasoconstriction • Occurs in the setting of decompensated cirrhosis – Primary etiologies: NASH, hepatitis C or alcoholic liver disease NASH=Non-Alcoholic Steato-Hepatitis CC-3 Diagnosis of HRS-1 • Diagnosis of exclusion • Rapid intervention is critical • Requires interdisciplinary approach – Hepatologists – Nephrologists – Intensivists – Transplant surgeons CC-4 Treatment of HRS-1 • Goals of treatment – Improve renal function – Reverse HRS-1 • Successful treatment – Facilitates medical management of critically ill patient – Allows recovery of patients with reversible component of liver disease – Improves outcomes of patients with liver transplant • No approved treatment for HRS-1 in the US CC-5 Terlipressin • A synthetic vasopressin analogue • V1 receptor selectivity: splanchnic vasculature • Restores effective blood volume and improves renal perfusion • Improves renal function, HRS reversal, clinical outcomes • Approved in EU, Asia, Australia, Africa and Latin America • Recommended for use in combination with albumin1,2 1. Angeli P. et al. J Hepatol. 2015;62(4):968-74. -

Auspar Attachment 1: Product Information for Lucassin (Terlipressin)
Attachment 1: Product information for AusPAR Lucassin Terlipressin Ikaria Australia Pty Ltd Sponsor PM-2010-02975-3-1 Date of finalisation 27 August 2013. This Product Information was approved at the time this AusPAR was published. PRODUCT INFORMATION LUCASSIN® (Terlipressin 0.85 mg powder for injection) NAME OF THE MEDICINE: Terlipressin. Structure: Terlipressin is a 12-amino acid peptide with the chemical name N-(N- (N-glycylglycyl)glycyl)- 8-L-lysinevasopressin. Terlipressin has the following amino acid sequence: H-Gly-Gly-Gly-Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Lys-Gly-NH2 |_________________ | Molecular formula: C52 H74 N16 O15 S2 (terlipressin free base). Molecular weight: 1227.4 (terlipressin free base) CAS number: 14636-12-5 pKa: 10.01 calculated DESCRIPTION: LUCASSIN is provided as a sterile, lyophilized powder in a clear glass vial for intravenous administration; mannitol is used as the caking agent. Glacial acetic acid and/or sodium hydroxide are used to adjust the pH to achieve a final product pH of 4.3 - 7.5. Each vial of LUCASSIN contains 0.85 mg terlipressin free base and approximately two equivalents (0.084 mg) of acetic acid. Thus, the drug substance is present mainly in the form of terlipressin diacetate. Terlipressin diacetate is freely soluble in water. Each vial must be reconstituted with 5mL of 0.9% sodium chloride injection prior to use. PHARMACOLOGY: Mechanism of Action: Hepatorenal syndrome (HRS) is caused by intra-renal vasoconstriction and circulatory dysfunction characterised by vasodilation in the splanchnic circulation leading to hypoperfusion of the kidneys. As a result, renal perfusion and glomerular filtration rate are greatly reduced, but tubular function is preserved. -

< MOH Approved Drugs List >
Ministry Of Health Directorate General of Medical Supplies Rep_Id : App_Drugs_List_Who.rdf < MOH Approved Drugs List > DATE : 12/08/2009 Page : 1 of 108 VED Flag <S.No> < Item Code > < I T E M D E S C ROF I P- T I O N > < U N I T > DATE : ABC Flag H/C Flag Category : DRUGS 1 Ph. System : GASTRO-INTESTINAL SYSTEM 1 Main Group : ANTACIDS 1 Sub Group : ALUMINIUM COMPOUNDS 1 03000000105 ALUMINIUM HYDROXIDE GEL, DRIED 475 MG. CAPSULE Desirable Cat_C Not H/C Item 2 Sub Group : ANTACID COMPOUND PREPARATIONS 2 02000000079 ANTACID SUSPENSION (ALUMINIUM HYDROXIDE + BOTTLE Desirable MAGNESIUM HYDROXIDE OR TRISILICATE) 100 - 200 Cat_A ML. B0TTLE. H/C Item 3 03000000173 ANTACID TABLET (ALUMINIUM HYDROXIDE + TABLET/CAP Desirable MAGNESIUM HYDROXIDE OR TRISILICATE). Cat_A H/C Item 2 Main Group : ANTISPASMODICS 1 Sub Group : ANTIMUSCARINICS 4 01000000304 HYOSCINE N BUTYLBROMIDE 20MG/ML. 1ML. AMPOULE Essantial Cat_A H/C Item 5 03000000640 HYOSCINE N BUTYL BROMIDE 10MG. TABLET/CAP Essantial Cat_A H/C Item 6 020D0000063 ANTISPASMODIC DROPS 15ML-25ML. BOTTLE Desirable Cat_C Not H/C Item 2 Sub Group : OTHER ANTISPASMODIC AND MOTILITY STIMULANT 7 03000001245 MEBEVERINE HYDROCHLORIDE 100 MG - 135 MG. TABLET/CAP Essantial Cat_B Not H/C Item Ministry Of Health Directorate General of Medical Supplies Rep_Id : App_Drugs_List_Who.rdf < MOH Approved Drugs List > DATE : 12/08/2009 Page : 2 of 108 VED Flag <S.No> < Item Code > < I T E M D E S C ROF I P- T I O N > < U N I T > DATE : ABC Flag H/C Flag Category : DRUGS 1 Ph. -

Effects of Terlipressin As Early Treatment for Protection of Brain in A
Ida et al. Critical Care (2015) 19:107 DOI 10.1186/s13054-015-0825-9 RESEARCH Open Access Effects of terlipressin as early treatment for protection of brain in a model of haemorrhagic shock Keila Kazue Ida1,2*, Denise Aya Otsuki1, Adolfo Toshiro Cotarelli Sasaki1, Emilyn Silva Borges1, Letícia Urbano Cardoso Castro3, Talita Rojas Sanches3, Maria-Heloisa Massola Shimizu3, Lúcia Conceição Andrade3, José-Otávio Costa Auler Jr1, Alex Dyson4, Kenneth John Smith2, Joel Avancini Rocha Filho5 and Luiz-Marcelo Sá Malbouisson1 Abstract Introduction: We investigated whether treatment with terlipressin during recovery from hypotension due to haemorrhagic shock (HS) is effective in restoring cerebral perfusion pressure (CPP) and brain tissue markers of water balance, oxidative stress and apoptosis. Methods: In this randomised controlled study, animals undergoing HS (target mean arterial pressure (MAP) 40 mmHg for 30 minutes) were randomised to receive lactated Ringer’s solution (LR group; n =14; volume equal to three times thevolumebled),terlipressin(TERLIgroup;n =14; 2-mg bolus), no treatment (HAEMO group; n =12) or sham (n =6). CPP, systemic haemodynamics (thermodilution technique) and blood gas analyses were registered at baseline, shock and 5, 30, 60 (T60), 90 and 120 minutes after treatment (T120). After the animals were killed, brain tissue samples were obtained to measure markers of water balance (aquaporin-4 (AQP4)), Na+-K+-2Cl− co-transporter (NKCC1)), oxidative stress (thiobarbituric acid reactive substances (TBARS) and manganese superoxide dismutase (MnSOD)) and apoptotic damage (Bcl-x and Bax). Results: Despite the HS-induced decrease in cardiac output (CO) and hyperlactataemia, resuscitation with terlipressin recovered MAP and resulted in restoration of CPP and in cerebral protection expressed by normalisation of AQP4, NKCC1, TBARS and MnSOD expression and Bcl-x/Bax ratio at T60 and T120 compared with sham animals. -

Respiratory Medication Use in Australia 2003–2013
This report describes patterns of dispensing of respiratory medications in Australia through detailed analyses of Respiratory medication use in Australia Pharmaceutical Benefits Scheme (PBS) data, as well as other sources, to draw inferences about respiratory 2003–2013 medication use among patients with asthma and COPD. It provides a valuable update and new information Treatment of asthma and COPD about the use of medicines for asthma and COPD, thus improving our knowledge and understanding about how these diseases are managed in Australia. ACAM Australian Centre for Airways disease Monitoring Respiratory medication use in Australia 2003–2013 Treatment of asthma and COPD Australian Institute of Health and Welfare Canberra Cat. no. ACM 31 The Australian Institute of Health and Welfare is a major national agency which provides reliable, regular and relevant information and statistics on Australia’s health and welfare. The Institute’s mission is authoritative information and statistics to promote better health and wellbeing. © Australian Institute of Health and Welfare and Woolcock Institute of Medical Research Limited 2015 This product, excluding the AIHW logo, Commonwealth Coat of Arms and any material owned by a third party or protected by a trademark, has been released under a Creative Commons BY 3.0 (CC-BY 3.0) licence. Excluded material owned by third parties may include, for example, design and layout, images obtained under licence from third parties and signatures. We have made all reasonable efforts to identify and label material owned by third parties. You may distribute, remix and build upon this work. However, you must attribute the AIHW as the copyright holder of the work in compliance with our attribution policy available at <www.aihw.gov.au/copyright/>. -

Queensland Health List of Approved Medicines
Queensland Health List of Approved Medicines Drug Form Strength Restriction abacavir * For use in accord with PBS Section 100 indications * oral liquid See above 20 mg/mL See above tablet See above 300 mg See above abacavir + lamivudine * For use in accord with PBS Section 100 indications * tablet See above 600 mg + 300 mg See above abacavir + lamivudine + * For use in accord with PBS Section 100 indications * zidovudine tablet See above 300 mg + 150 mg + 300 mg See above abatacept injection 250 mg * For use in accord with PBS Section 100 indications * abciximab (a) Interventional Cardiologists for complex angioplasty (b) Interventional and Neuro-interventional Radiologists for rescue treatment of thromboembolic events that occur during neuroendovascular procedures. * Where a medicine is not TGA approved, patients should be made fully aware of the status of the medicine and appropriate consent obtained * injection See above 10 mg/5 mL See above abiraterone For use by medical oncologists as per the PBS indications for outpatient and discharge use only tablet See above 250 mg See above 500 mg See above acamprosate Drug and alcohol treatment physicians for use with a comprehensive treatment program for alcohol dependence with the goal of maintaining abstinence. enteric tablet See above 333 mg See above acarbose For non-insulin dependent diabetics with inadequate control despite diet; exercise and maximal tolerated doses of other anti-diabetic agents tablet See above 50 mg See above 100 mg See above acetazolamide injection 500 mg tablet 250 mg acetic acid ear drops 3% 15mL solution 2% 100mL green 3% 1 litre 6% 1 Litre 6% 200mL Generated on: 30-Aug-2021 Page 1 of 142 Drug Form Strength Restriction acetylcysteine injection For management of paracetamol overdose 2 g/10 mL See above 6 g/30 mL See above aciclovir cream Infectious disease physicians, haematologists and oncologists 5% See above eye ointment For use on the advice of Ophthalmologists only. -
ATC) Classification and the Defined Daily Dose (DDD
Anatomical Therapeutic Chemical (ATC) classification T and the Defined Daily Dose AF DR (DDD): principles for classifying and quantifying drug use Yong Chen Merck, Whitehouse Station, NJ USA Disclosure • Author is an employee of Merck • A lot of slides are adopted from a prior ICPE English short course on drug utilization by Hege Salvesen Blix 2 Outline • The ATC/DDD methodology – definitions, purpose, structure and principles • Real world applications of ATC/DDD 3 What is ATC/DDD? • ATC (Anatomical Therapeutic Chemical) classification –Don’t confuse it with Anatomical Therapeutic (AT) classification developed by European Pharmaceutical Market Research Association (EPhMRA) • DDD (Defined Daily Dose) The assumed average maintenance dose per day for a drug used for its main indication in adults Introduction to Drug Utilization Research, WHO 2003 4 Main Purpose • “International language for drug utilization research” –to serve as a tool for presenting drug utilization research in order to improve quality of drug use –to compare data within a country and between countries 5 The WHO Collaborating Centre for Drug Statistics Methodology • Established in 1982 as a European WHO Centre • Since 1996 a global WHO Centre • Located in the Department of Pharmacoepidemiology at the Norwegian Institute of Public Health • The staff of the Centre is responsible for drug consumption statistics in Norway 6 The WHO Centre • To classify drugs according to the ATC system and assign DDDs • To review and revise as necessary the ATC classification system and DDDs • To stimulate and influence the practical use of the ATC system • To organize training courses in the ATC/DDD methodology 7 ATC Main Group • A Alimentary tract and metabolism • B Blood and blood forming organs • C Cardiovascular system • D Dermatologicals • G Genito urinary system and sex hormones • H Systemic hormonal preparations, excl.