Keratoacanthoma: Understanding by Immune Responses International Case Reports Journal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NWDC Mohs & Dermatology Associates: Wound Care After Cryosurgery LIQUID NITROGEN/CRYOTHERAPY WOUND CARE INSTRUCTIONS
NWDC Mohs & Dermatology Associates: Wound care after Cryosurgery Dermatology (Adult & Pediatric), Dermatopathology, Mohs & Dermatologic Surgery, Phlebology LIQUID NITROGEN/CRYOTHERAPY WOUND CARE INSTRUCTIONS Cryosurgery is a procedure in which skin is quickly frozen by applying a spray of liquid nitrogen to the area being treated. Liquid nitrogen is very cold. Cryosurgery may be an alternative to regular surgery. It takes a few minutes and may be used to treat precancerous or noncancerous (benign) growths (warts, skin tags, large oil glands, etc.). Procedure Liquid nitrogen is applied directly on the skin as a spray or with a cotton-tipped applicator. Several applications may be needed to treat the area. You may feel a stinging or burning sensation during cryosurgery. The area treated will become swollen, turn pink, then red, and may blister. As the skin peels, the treated lesion will peel off as well. Occasionally, several treatment sessions may be needed to treat your condition. A black eye is not uncommon if you had cryosurgery near or above the eyes. Home Care Instructions Wounds heal best when kept covered and moist. Avoid crusting or scabbing. 1. If the skin is opened, clean the area twice a day with clean water (clean tap water or normal saline) and apply an ointment (Vaseline petrolatum or Aquaphor ). 2. Do not use Polysporin , Neosporin , or Bacitracin other antibiotic ointments. 3. Do not use hydrogen peroxide to clean the wound. 4. If a blister forms and causes pain, you may lance the blister with a sterilized needle (boil a sewing needle and let it cool before using) and use a clean gauze to express out the blister fluid. -

2Nd Quarter 2001 Medicare Part a Bulletin
In This Issue... From the Intermediary Medical Director Medical Review Progressive Corrective Action ......................................................................... 3 General Information Medical Review Process Revision to Medical Record Requests ................................................ 5 General Coverage New CLIA Waived Tests ............................................................................................................. 8 Outpatient Hospital Services Correction to the Outpatient Services Fee Schedule ................................................................. 9 Skilled Nursing Facility Services Fee Schedule and Consolidated Billing for Skilled Nursing Facility (SNF) Services ............. 12 Fraud and Abuse Justice Recovers Record $1.5 Billion in Fraud Payments - Highest Ever for One Year Period ........................................................................................... 20 Bulletin Medical Policies Use of the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Codes on Contractors’ Web Sites ................................................................................. 21 Outpatient Prospective Payment System January 2001 Update: Coding Information for Hospital Outpatient Prospective Payment System (OPPS) ......................................................................................................................... 93 he Medicare A Bulletin Providers Will Be Asked to Register Tshould be shared with all to Receive Medicare Bulletins and health care -
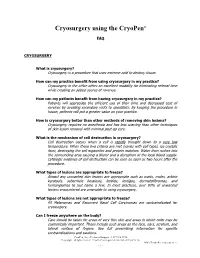
Cryosurgery Using the Cryopen®
Cryosurgery using the CryoPen® FAQ CRYOSURGERY What is cryosurgery? Cryosurgery is a procedure that uses extreme cold to destroy tissue. How can my practice benefit from using cryosurgery in my practice? Cryosurgery in the office offers an excellent modality for eliminating referral time while creating an added source of revenue. How can my patients benefit from having cryosurgery in my practice? Patients will appreciate the efficient use of their time and decreased cost of services by avoiding secondary visits to specialists. By keeping the procedure in house, patients will put a greater value on your practice. How is cryosurgery better than other methods of removing skin lesions? Cryosurgery requires no anesthesia and has less scarring than other techniques of skin lesion removal with minimal post-op care. What is the mechanism of cell destruction in cryosurgery? Cell destruction occurs when a cell is rapidly brought down to a very low temperature. When these two criteria are met (varies with cell type), ice crystals form, destroying the cell organelles and protein matrixes. Water then rushes into the surrounding area causing a blister and a disruption of the local blood supply. Cytologic evidence of cell destruction can be seen as soon as two hours after the procedure. What types of lesions are appropriate to freeze? Almost any unwanted skin lesions are appropriate such as warts, moles, actinic keratosis, seborrheic keratosis, keloids, lentigos, dermatofibromas, and hemangiomas to just name a few. In most practices, over 90% of unwanted lesions encountered are amenable to using cryosurgery. What types of lesions are not appropriate to freeze? All Melanomas and Recurrent Basal Cell Carcinomas are contraindicated for cryosurgery. -

The Costs and Benefits of Moving to the ICD-10 Code Sets
CHILDREN AND ADOLESCENTS This PDF document was made available from www.rand.org as a public CIVIL JUSTICE service of the RAND Corporation. EDUCATION ENERGY AND ENVIRONMENT Jump down to document HEALTH AND HEALTH CARE 6 INTERNATIONAL AFFAIRS POPULATION AND AGING The RAND Corporation is a nonprofit research PUBLIC SAFETY SCIENCE AND TECHNOLOGY organization providing objective analysis and effective SUBSTANCE ABUSE solutions that address the challenges facing the public TERRORISM AND HOMELAND SECURITY and private sectors around the world. TRANSPORTATION AND INFRASTRUCTURE U.S. NATIONAL SECURITY Support RAND Purchase this document Browse Books & Publications Make a charitable contribution For More Information Visit RAND at www.rand.org Explore RAND Science and Technology View document details Limited Electronic Distribution Rights This document and trademark(s) contained herein are protected by law as indicated in a notice appearing later in this work. This electronic representation of RAND intellectual property is provided for non-commercial use only. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. This product is part of the RAND Corporation technical report series. Reports may include research findings on a specific topic that is limited in scope; present discus- sions of the methodology employed in research; provide literature reviews, survey instruments, modeling exercises, guidelines for practitioners and research profes- sionals, and supporting documentation; -

Cryocarboxy Surgery: a New Addition to the Armamentarium for the Treatment of Congenital Melanocytic Nevi of the Face Nader Elmelegy*
FM Publisher Frontiers Journal of Surgery (FJS) Volume 01, Issue 01, Article ID FJS-2020-02 Research Article Open Access Cryocarboxy Surgery: A New Addition to the Armamentarium for the Treatment of Congenital Melanocytic Nevi of the Face Nader Elmelegy* Professor of plastic surgery at Tanta University, Egypt Corresponding author: Elmelegy N, Professor of plastic surgery at Tanta University, Egypt. E-mail: [email protected] Citation: Elmelegy N (2020) Cryocarboxy surgery: A new addition to the armamentarium for the treatment of congenital melanocytic nevi of the face. Front J Surg Vol.1 No.1:2. Copyright: © 2020 Elmelegy N. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Received Date: 09 January 2020; Accepted Date: 17 January 2020; Published Date: 24 January 2020. ABSTRACT Background: Congenital melanocytic nevi (CMN) of the face cause substantial psychological and cosmetic problems in affected patients. The treatment of giant congenital nevi has been a longstanding challenge, but currently, various treatment options, such as cryotherapy, chemical peeling, electrical cautery, laser therapy, and surgery, have been tried for the treatment of CMN. In this article, we present our experience and the outcomes of the use of controlled CO2 gas as a cryogen in the treatment of CMN. Methods: This study included 28 patients with varying sizes of CMN seen from January 2014 to December 2017. Cryocarboxy surgery was performed in all cases. Results: The average evaluation score of our patients was excellent in 22 (78.6%) cases, good in 4 (14.3%) cases, satisfactory in two (7.1%) cases, and we had no poor results. -

A Case Report of Keratoacanthoma (KA) of the Alveolar Ridge of the Maxilla
Journal of Dental Health Oral Disorders & Therapy Case Report Open Access A case report of Keratoacanthoma (KA) of the alveolar ridge of the maxilla Abstract Volume 9 Issue 2 - 2018 Keratoacanthoma (KA) is a case related to skin squamous cell carcinoma but it is a self- limited case. It is usually seen in areas of exposed skin and rarely to be seen intra-orally. Sarraj Faysal,1,2 Sarraj Ayman,1 Pierrard Loïc,2 Here we present a case of oral keratoacanthoma on the alveolar ridge of the maxillae, Hafian Hilal,2 Lefevre Benoit2 which may arise as a result of trauma or unknown stimulus. The case was treated with 1Faculty of Dentistry, University of Aleppo, Syria liquid nitrogen for six sessions and completely resolving of the lesion was recorded without 2Faculty of Dentistry, Reims University, France a scar formation. Cryosurgery for exophytic lesions either benign or malignant (well differentiated) is worthy to be recommended than traditional surgery. Correspondence: Sarraj Faysal, Department of Odontology, Reims Champagne-Ardennes University, 2 rue du General Keywords: Keratoacanthoma (KA), squamous cell carcinoma, intraoral, cryosurgery, Koenig, 51100 Reims, France, Tel +33788543508, Fax liquid nitrogen +33326913480, Email [email protected], [email protected] Received: January 11, 2018 | Published: March 13, 2018 Abbreviations: KA, Keratoacanthoma; SCC, squamous cell be present as solitary or multiple lesions (Table 1).5 The etiological carcinoma factors for this lesion are sunlight exposure, viruses and possibly other suspected factors such as chemical carcinogens, trauma, and Introduction disordered cellular immunity.6 The lesion usually begins as a small red macule that soon becomes a firm papule. -

What to Expect Following Cryosurgery “Freezing”
What to Expect Following CryoSurgery “Freezing” What is Cryosurgery? Cryosurgery is a technique for removing skin lesions that primarily involve the surface of the skin, such as warts, seborrheic keratosis, or actinic keratosis. It is a quick method of removing the lesions with minimal scarring. The liquid nitrogen needs to be applied long enough to freeze the affected skin. By freezing the skin, a blister is created underneath the lesion. Ideally, as the new skin forms underneath the blister, the abnormal skin on the roof of the blister peels off. Occasionally if the lesion is very thick (such as a large wart), only the surface is blistered off. The base or residual lesion may need to be frozen at another visit. What to Expect Over the Next Few Weeks? During Treatment – Area being treated will sting, burn and then possibly itch. Immediately After Treatment – Area will be red sore and swollen. Next Day- Blister or blood blister has formed, tenderness starts to subside. Apply a Band-Aid if necessary. 7 Days- Surface is dark red/brown and scab-like. Apply Vaseline or an antibacterial ointment if necessary. 2 to 4 Weeks- The surface starts to peel off. This may be encouraged gently during bathing, when the scab is softened. No makeup should be applied until area is fully healed. How to Take care of the Skin after Cryosurgery A Band-Aid can be used for larger blisters or blisters in areas that are more likely to be traumatized- such as fingers and toes. If the area becomes dry or crusted, an ointment (Vaseline, Aquaphor) can also be applied. -

Slide Courtesy of Jeff North, MD
3/17/2017 Basic Dermatology Procedures Basic Dermatology Procedures for the Non‐dermatologist • Liquid Nitrogen • Skin Biopsies Lindy P. Fox, MD • Electrocautery Associate Professor Director, Hospital Consultation Service Department of Dermatology University of California, San Francisco [email protected] I have no conflicts of interest to disclose 1 Liquid Nitrogen Cryosurgery 1 3/17/2017 Liquid Nitrogen Cryosurgery Liquid Nitrogen Cryosurgery Principles • Indications • ‐ 196°C (−320.8°F) – Benign, premalignant, in situ malignant lesions • Temperatures of −25°C to −50°C (−13°F to −58°F) within 30 seconds with spray or probe • Objective – Selective tissue necrosis • Benign lesions: −20°C to −30°C (−4°F to −22°F) • Reactions predictable • Malignant lesions: −40°C to −50°C. – Crust, bulla, exudate, edema, sloughing • Post procedure hypopigmentation • Rapid cooling intracellular ice crystals • Slow thawing tissue damage – Melanocytes are more sensitive to freezing than • Duration of THAW (not freeze) time is most keratinocytes important factor in determining success Am Fam Physician. 2004 May 15;69(10):2365‐2372 Liquid Nitrogen Cryosurgery • Fast freeze, slow thaw cycles – Times vary per condition (longer for deeper lesion) – One cycle for benign, premalignant – Two cycles for warts, malignant (not commonly done) • Lateral spread of freeze (indicates depth of freeze) – Benign lesions 1‐2mm beyond margins – Actinic keratoses‐ 2‐3mm beyond margins – Malignant‐ 3‐5+mm beyond margins (not commonly done) From: Bolognia, Jorizzo, and Schaffer. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Revised Mohs Surgery Care Guidelines for Squamous Cell Carcinoma In-Situ Are Overdue
Volume 25 Number 3| March 2019| Dermatology Online Journal || Commentary 25(3):2 Revised Mohs surgery care guidelines for squamous cell carcinoma in-situ are overdue Sama K Carley1 MD, Anthony Dixon2 PhD MBBS, Christopher B Zachary1 MBBS FRCP, Howard K Steinman3,4 MD Affiliations: 1University of California Irvine, Department of Dermatology, Irvine, California, USA, 2Australasian College of Cutaneous Oncology, Docklands, Victoria, Australia, 3Campbell University School of Osteopathic Medicine, Lillington, NC, USA, 4US Dermatology Partners, Grapevine, Texas, USA Corresponding Author: Christopher B. Zachary MBBS FRCP, University of California, Irvine, Department of Dermatology, 118 Med Surge I, Irvine, California 92697, Tel: 949-824-4405, Email: [email protected] Surgery Appropriate Use Criteria (MAUC), [1]. We Abstract discuss the rationale for a change in the MAUC for The treatment of cutaneous squamous cell SCCis. carcinoma in situ by Mohs micrographic surgery is currently deemed as appropriate by the Mohs Discussion Appropriate Use Criteria. However, squamous cell carcinoma in situ is a very superficial, indolent, low- Cutaneous SCCis is a common, intra-epidermal, low- risk tumor amenable to destructive and non-surgical risk, indolent malignancy [2, 3]. Many involve the treatments. It is uncommon for squamous cell superficial hair follicle [4]. However, risk of progression carcinoma in situ to have progressed to invasive to invasive SCC is only 3-5%, and SCCis has a negligible malignancy subsequent to definitive management. risk of metastasis [5, 6]. This low risk of progression to The suggestion that squamous cell carcinoma in situ SCC and metastasis exists despite the reported on certain anatomic locations has a poorer prognosis presence of invasive SCC in 9.8% of biopsies diagnosed is widely assumed but lacks an evidence base. -

Basal Cell Carcinoma-A Review of Treatment Results with Special Reference to Cryotherapy D. R. OSBORNE A. K. C. LI* K. E. F
Postgrad Med J: first published as 10.1136/pgmj.59.697.698 on 1 November 1983. Downloaded from Postgraduate Medical Journal (November 1983) 59, 698-701 PAPERS Basal cell carcinoma-a review of treatment results with special reference to cryotherapy G. S. MCINTOSH D. R. OSBORNE M.B., F.R.C.S. M.B., F.R.C.S. A. K. C. LI* K. E. F. HOBBS M.D., F.R.C.S. Ch.M., F.R.C.S. Academic Department of Surgery, Royal Free Hospital School of Medicine, London NW3 Summary skin tumour in Caucasians (Sanderson and Mackie, A retrospective study has been undertaken of all head 1979), is locally slow growing and in most cases there and neck basal cell cancers treated at the Royal Free is no lymphatic spread. It occurs mostly on the face Hospital between 1976 and 1980 inclusive. and neck and typically presents as a recognizable Four methods of treatment were used during the ulcerated keratotic lesion which fails to heal. Cystic, period: simple excision with primary closure (n= 43), superficial and the very rare morphoeic forms by copyright. may skin grafting or trans-position flap (n- 19), radiother- also occur. apy (n= 99), and cryosurgical ablation (n= 34). The The current commonly used treatments for this methods were compared by observing the immediate condition include curettage with and without dia- results, the subsequent tumour recurrence rate and thermy (Sweet, 1963; Crissey, 1971), surgical excision the length of follow-up. with primary closure or grafting (Bart et al., 1978; Statistical comparison of tumour recurrence rate Battle and Patterson, 1960; Taylor and Barsini, 1973), showed no significant difference between treatment radiotherapy (Bart, Kopf and Petratos, 1970; Free- groups. -

Cryosurgery for the Treatment of Rosacea Emanuel G
REVIEW Cryosurgery for the Treatment of Rosacea Emanuel G. Kuflik, MD Rosacea is a common, chronic condition that occurs in both men and women and mainly is seen on the central portion of the face. It is a clinical diagnosis with a spectrum of clinical signs, including flushing, persistent erythema, papules, pustules, telangiectasia, coarseness of skin, and scaling. Cryosurgery may be administered either as adjunctive treatment or monotherapy for the treatment of rosacea. dvantages of cryosurgery for the treatment on the type of eruption and the character and size of of rosacea include easy treatment, low cost, the lesion. and safety duringCOS pregnancy; it also is use-DERMFor the papulopustular type of rosacea, cryosurgery ful in patients with rosacea for whom oral is used to diminish or clear the papules or pustules by or topical medications are contraindicated reduction of inflammation, as is the case with the treat- Aor undesirable.1,2 ment of acne vulgaris and cystic acne. Cryosurgery for There are 4 types of rosacea: erythematotelangiec- the treatment of rosacea is performed using either the tatic, papulopustular, phymatous,Do and ocularNot rosacea.3 open Copy spray technique or with the “slush” technique. Although the condition can become severe or lead to The former is employed using an acne spray tip. Either disfiguration, most patients with rosacea present to der- the individual lesions or the involved fields are treated for matologists with complaints about cosmetic appearance approximately 4 to 8 seconds. Treatment is administered due to mild or moderate disease. Treatment generally every one to 2 months, or more frequently.