Comprehensive Maternal Serum Proteomics Identifies The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table S1 the Four Gene Sets Derived from Gene Expression Profiles of Escs and Differentiated Cells
Table S1 The four gene sets derived from gene expression profiles of ESCs and differentiated cells Uniform High Uniform Low ES Up ES Down EntrezID GeneSymbol EntrezID GeneSymbol EntrezID GeneSymbol EntrezID GeneSymbol 269261 Rpl12 11354 Abpa 68239 Krt42 15132 Hbb-bh1 67891 Rpl4 11537 Cfd 26380 Esrrb 15126 Hba-x 55949 Eef1b2 11698 Ambn 73703 Dppa2 15111 Hand2 18148 Npm1 11730 Ang3 67374 Jam2 65255 Asb4 67427 Rps20 11731 Ang2 22702 Zfp42 17292 Mesp1 15481 Hspa8 11807 Apoa2 58865 Tdh 19737 Rgs5 100041686 LOC100041686 11814 Apoc3 26388 Ifi202b 225518 Prdm6 11983 Atpif1 11945 Atp4b 11614 Nr0b1 20378 Frzb 19241 Tmsb4x 12007 Azgp1 76815 Calcoco2 12767 Cxcr4 20116 Rps8 12044 Bcl2a1a 219132 D14Ertd668e 103889 Hoxb2 20103 Rps5 12047 Bcl2a1d 381411 Gm1967 17701 Msx1 14694 Gnb2l1 12049 Bcl2l10 20899 Stra8 23796 Aplnr 19941 Rpl26 12096 Bglap1 78625 1700061G19Rik 12627 Cfc1 12070 Ngfrap1 12097 Bglap2 21816 Tgm1 12622 Cer1 19989 Rpl7 12267 C3ar1 67405 Nts 21385 Tbx2 19896 Rpl10a 12279 C9 435337 EG435337 56720 Tdo2 20044 Rps14 12391 Cav3 545913 Zscan4d 16869 Lhx1 19175 Psmb6 12409 Cbr2 244448 Triml1 22253 Unc5c 22627 Ywhae 12477 Ctla4 69134 2200001I15Rik 14174 Fgf3 19951 Rpl32 12523 Cd84 66065 Hsd17b14 16542 Kdr 66152 1110020P15Rik 12524 Cd86 81879 Tcfcp2l1 15122 Hba-a1 66489 Rpl35 12640 Cga 17907 Mylpf 15414 Hoxb6 15519 Hsp90aa1 12642 Ch25h 26424 Nr5a2 210530 Leprel1 66483 Rpl36al 12655 Chi3l3 83560 Tex14 12338 Capn6 27370 Rps26 12796 Camp 17450 Morc1 20671 Sox17 66576 Uqcrh 12869 Cox8b 79455 Pdcl2 20613 Snai1 22154 Tubb5 12959 Cryba4 231821 Centa1 17897 -

Defining Functional Interactions During Biogenesis of Epithelial Junctions
ARTICLE Received 11 Dec 2015 | Accepted 13 Oct 2016 | Published 6 Dec 2016 | Updated 5 Jan 2017 DOI: 10.1038/ncomms13542 OPEN Defining functional interactions during biogenesis of epithelial junctions J.C. Erasmus1,*, S. Bruche1,*,w, L. Pizarro1,2,*, N. Maimari1,3,*, T. Poggioli1,w, C. Tomlinson4,J.Lees5, I. Zalivina1,w, A. Wheeler1,w, A. Alberts6, A. Russo2 & V.M.M. Braga1 In spite of extensive recent progress, a comprehensive understanding of how actin cytoskeleton remodelling supports stable junctions remains to be established. Here we design a platform that integrates actin functions with optimized phenotypic clustering and identify new cytoskeletal proteins, their functional hierarchy and pathways that modulate E-cadherin adhesion. Depletion of EEF1A, an actin bundling protein, increases E-cadherin levels at junctions without a corresponding reinforcement of cell–cell contacts. This unexpected result reflects a more dynamic and mobile junctional actin in EEF1A-depleted cells. A partner for EEF1A in cadherin contact maintenance is the formin DIAPH2, which interacts with EEF1A. In contrast, depletion of either the endocytic regulator TRIP10 or the Rho GTPase activator VAV2 reduces E-cadherin levels at junctions. TRIP10 binds to and requires VAV2 function for its junctional localization. Overall, we present new conceptual insights on junction stabilization, which integrate known and novel pathways with impact for epithelial morphogenesis, homeostasis and diseases. 1 National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK. 2 Computing Department, Imperial College London, London SW7 2AZ, UK. 3 Bioengineering Department, Faculty of Engineering, Imperial College London, London SW7 2AZ, UK. 4 Department of Surgery & Cancer, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Tropomodulin Isoform-Specific Regulation of Dendrite Development and Synapse Formation
This Accepted Manuscript has not been copyedited and formatted. The final version may differ from this version. Research Articles: Cellular/Molecular Tropomodulin Isoform-Specific Regulation of Dendrite Development and Synapse Formation Omotola F. Omotade1,3, Yanfang Rui1,3, Wenliang Lei1,3, Kuai Yu1, H. Criss Hartzell1, Velia M. Fowler4 and James Q. Zheng1,2,3 1Department of Cell Biology, Emory University School of Medicine, Atlanta, GA 30322. 2Department of Neurology 3Center for Neurodegenerative Diseases, Emory University School of Medicine, Atlanta, GA 30322. 4Department of Molecular Medicine, Scripps Research Institute, La Jolla, CA 92037 DOI: 10.1523/JNEUROSCI.3325-17.2018 Received: 22 November 2017 Revised: 25 September 2018 Accepted: 2 October 2018 Published: 9 October 2018 Author contributions: O.F.O. and J.Q.Z. designed research; O.F.O., Y.R., W.L., and K.Y. performed research; O.F.O. and J.Q.Z. analyzed data; O.F.O. and J.Q.Z. wrote the paper; Y.R., H.C.H., V.M.F., and J.Q.Z. edited the paper; V.M.F. contributed unpublished reagents/analytic tools. Conflict of Interest: The authors declare no competing financial interests. This research project was supported in part by research grants from National Institutes of Health to JQZ (GM083889, MH104632, and MH108025), OFO (5F31NS092437-03), VMF (EY017724) and HCH (EY014852, AR067786), as well as by the Emory University Integrated Cellular Imaging Microscopy Core of the Emory Neuroscience NINDS Core Facilities grant (5P30NS055077). We would like to thank Dr. Kenneth Myers for his technical expertise and help throughout the project. We also thank Drs. -

Serum Albumin OS=Homo Sapiens
Protein Name Cluster of Glial fibrillary acidic protein OS=Homo sapiens GN=GFAP PE=1 SV=1 (P14136) Serum albumin OS=Homo sapiens GN=ALB PE=1 SV=2 Cluster of Isoform 3 of Plectin OS=Homo sapiens GN=PLEC (Q15149-3) Cluster of Hemoglobin subunit beta OS=Homo sapiens GN=HBB PE=1 SV=2 (P68871) Vimentin OS=Homo sapiens GN=VIM PE=1 SV=4 Cluster of Tubulin beta-3 chain OS=Homo sapiens GN=TUBB3 PE=1 SV=2 (Q13509) Cluster of Actin, cytoplasmic 1 OS=Homo sapiens GN=ACTB PE=1 SV=1 (P60709) Cluster of Tubulin alpha-1B chain OS=Homo sapiens GN=TUBA1B PE=1 SV=1 (P68363) Cluster of Isoform 2 of Spectrin alpha chain, non-erythrocytic 1 OS=Homo sapiens GN=SPTAN1 (Q13813-2) Hemoglobin subunit alpha OS=Homo sapiens GN=HBA1 PE=1 SV=2 Cluster of Spectrin beta chain, non-erythrocytic 1 OS=Homo sapiens GN=SPTBN1 PE=1 SV=2 (Q01082) Cluster of Pyruvate kinase isozymes M1/M2 OS=Homo sapiens GN=PKM PE=1 SV=4 (P14618) Glyceraldehyde-3-phosphate dehydrogenase OS=Homo sapiens GN=GAPDH PE=1 SV=3 Clathrin heavy chain 1 OS=Homo sapiens GN=CLTC PE=1 SV=5 Filamin-A OS=Homo sapiens GN=FLNA PE=1 SV=4 Cytoplasmic dynein 1 heavy chain 1 OS=Homo sapiens GN=DYNC1H1 PE=1 SV=5 Cluster of ATPase, Na+/K+ transporting, alpha 2 (+) polypeptide OS=Homo sapiens GN=ATP1A2 PE=3 SV=1 (B1AKY9) Fibrinogen beta chain OS=Homo sapiens GN=FGB PE=1 SV=2 Fibrinogen alpha chain OS=Homo sapiens GN=FGA PE=1 SV=2 Dihydropyrimidinase-related protein 2 OS=Homo sapiens GN=DPYSL2 PE=1 SV=1 Cluster of Alpha-actinin-1 OS=Homo sapiens GN=ACTN1 PE=1 SV=2 (P12814) 60 kDa heat shock protein, mitochondrial OS=Homo -

A Novel Phenotype Associated with ACTB Mutations Sharissa
Thrombocytopenia Microcephaly Syndrome - a novel phenotype associated with ACTB mutations Sharissa L. Latham#,*,1, Nadja Ehmke#,2,3, Patrick Y.A. Reinke1,4, Manuel H. Taft1, Michael J. Lyons5, Michael J Friez5, Jennifer A. Lee5, Ramona Hecker6, Michael C. Fruehwald7, Kerstin Becker8, Teresa M. Neuhann8, Denise Horn2, Evelin Schrock9, Katharina Sarnow9, Konrad Grützmann10, Luzie Gawehn9, Barbara Klink9, Andreas Rump9, Christine Chaponnier11, Ralf J. Knöfler12, Dietmar J. Manstein*,1,4 and Natalia Di Donato*,9 Supplementary notes. Variant ACTB mRNA and β-CYA are present in patient primary fibroblasts All ACTB-TMS patients display heterozygous ACTB mutations. We confirm by RNA-Seq that these ACTB-TMS mutations do not result in nonsense-mediated mRNA decay and show that the variant mRNA accounts for 50% of the ACTB mRNA present in P3 and P5 primary fibroblasts (Supplementary Fig. 7a). With mass spectrometry, we can identify the altered C-terminal frame shift peptide in P3 only (Supplementary Fig. 7b). The 4 amino acid deletion of P5 could not be detected by this method. However, this peptide region was also not detected in the control. Whole-transcriptome analysis (RNA-Seq) To further understand the mechanisms of action, we studied the effect of ACTB-TMS mutations on the global gene expression profile of fibroblasts obtained from P3, P5 and a healthy control. RNA was isolated from three independent fibroblast cell culture flasks for each individual and subsequent whole transcriptome sequencing was performed. Principal component analysis showed clear grouping of replicates for one individual and clear separation between samples from different individuals. Sample distance analysis and unsupervised hierarchical clustering showed a clear separation between patient samples and control in two main clusters, with a further separation between the two patients within the ACTB-mutation cluster (Supplementary Figures 8). -
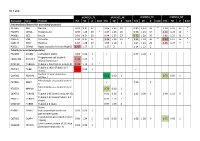
S1 Table Protein
S1 Table dFSHD12_TE dFSHD12_NE aFSHD51_TE aFSHD51_NE Accession Gene Protein H/L SD # bold H/L SD # bold H/L SD # bold H/L SD # bold Intermediate filament (or associated proteins) P17661 DES Desmin 0.91 N.D. 37 1.06 1.35 19 0.89 1,13 33 * 1.20 1.21 17 * P02545 LMNA Prelamin-A/C 0.90 1.25 30 * 1.07 1.26 20 0.96 1.23 34 1.21 1.24 19 * P48681 NES Nestin 0.91 N.D. 60 0.94 1.25 27 0.72 1.20 50 * 0.89 1.27 31 * P08670 VIM Vimentin 1.04 N.D. 35 1.24 1.24 14 * 1.21 1.18 36 * 1.39 1.17 16 * Q15149 PLEC Plectin-1 1.10 1.28 19 1.05 1.10 3 1.07 1.23 26 1.25 1.27 7 * P02511 CRYAB Alpha-crystallin B chain (HspB5) 1.47 1.17 2 1.17 2 1.14 1.12 2 Tubulin (or associated proteins) P62158 CALM1 Calmodulin (CaM) 0.83 0.00 1 0.93 0.00 1 Programmed cell death 6- Q8WUM4 PDCD6IP 1.34 0.00 1 interacting protein Q71U36 TUBA1A Tubulin α-1A chain (α-tubulin 3) 1.44 1.12 3 * Tubulin β chain (Tubulin β-5 P07437 TUBB 1.52 0.00 1 chain) Nuclear mitotic apparatus Q14980 NUMA1 0.68 0.00 1 0.75 0.00 1 protein 1 Microtubule-associated protein P27816 MAP4 1.10 1 4 Microtubule-associated protein P78559 MAP1A 0.76 0.00 1 1A Q6PEY2 TUBA3E Tubulin α-3E chain (α-tubulin 3E) 0.91 0.00 1 1.12 0.00 1 0.98 1.12 3 Tubulin β-2C chain (Tubulin β-2 P68371 TUBB2C 0.93 1.13 7 chain) Q3ZCM7 TUBB8 Tubulin β-8 chain 0.97 1.09 4 Serine P34897 SHMT2 hydroxymethyltransferase 0.93 0.00 1 (serine methylase) Cytoskeleton-associated protein Q07065 CKAP4 0.98 1.24 5 0.96 0.00 1 1.08 1.28 6 0.75 0.00 1 4 (p63) Centrosomal protein of 135 kDa Q66GS9 CEP135 0.84 0.00 1 (Centrosomal protein 4) Pre-B cell leukemia transcription Q96AQ6 PBXIP1 0.74 0.00 1 0.80 1 factor-interacting protein 1 T-complex protein 1 subunit P17897 TCP1 0.84 0.00 1 alpha (CCT-alpha) Cytoplasmic dynein Q13409 DYNC1I2 1.01 0.00 1 intermediate chain 2 (DH IC-2) Dynein heavy chain 3 (Dnahc3- Q8TD57 DNAH3 b) Microtubule-actin cross- linking Q9UPN3 MACF1 factor 1 (Trabeculin-alpha) Actin (or associated including myofibril-associated porteins) P60709 ACTB Actin, cytoplasmic 1 (β-actin) 1.11 N.D. -
Variants in Exons 5 and 6 of ACTB Cause Syndromic Thrombocytopenia
ARTICLE DOI: 10.1038/s41467-018-06713-0 OPEN Variants in exons 5 and 6 of ACTB cause syndromic thrombocytopenia Sharissa L. Latham 1, Nadja Ehmke2,3, Patrick Y.A. Reinke1,4, Manuel H. Taft 1, Dorothee Eicke5, Theresia Reindl1, Werner Stenzel6, Michael J. Lyons7, Michael J. Friez7, Jennifer A. Lee7, Ramona Hecker8, Michael C. Frühwald9, Kerstin Becker10, Teresa M. Neuhann10, Denise Horn2, Evelin Schrock11, Indra Niehaus11, Katharina Sarnow11, Konrad Grützmann12, Luzie Gawehn11, Barbara Klink 11, Andreas Rump11, Christine Chaponnier13, Constanca Figueiredo5, Ralf Knöfler14, Dietmar J. Manstein1,4 & Nataliya Di Donato 11 1234567890():,; Germline mutations in the ubiquitously expressed ACTB, which encodes β-cytoplasmic actin (CYA), are almost exclusively associated with Baraitser-Winter Cerebrofrontofacial syn- drome (BWCFF). Here, we report six patients with previously undescribed heterozygous variants clustered in the 3′-coding region of ACTB. Patients present with clinical features distinct from BWCFF, including mild developmental disability, microcephaly, and thrombo- cytopenia with platelet anisotropy. Using patient-derived fibroblasts, we demonstrate cohort specific changes to β-CYA filament populations, which include the enhanced recruitment of thrombocytopenia-associated actin binding proteins (ABPs). These perturbed interactions are supported by in silico modeling and are validated in disease-relevant thrombocytes. Co- examination of actin and microtubule cytoskeleton constituents in patient-derived mega- karyocytes and thrombocytes indicates that these β-CYA mutations inhibit the final stages of platelet maturation by compromising microtubule organization. Our results define an ACTB- associated clinical syndrome with a distinct genotype-phenotype correlation and delineate molecular mechanisms underlying thrombocytopenia in this patient cohort. 1 Institute for Biophysical Chemistry, Hannover Medical School, Hannover 30625, Germany. -

TPM4 Aggravates the Malignant Progression of Hepatocellular Carcinoma Through Negatively Regulating SUSD2
European Review for Medical and Pharmacological Sciences 2020; 24: 4756-4765 TPM4 aggravates the malignant progression of hepatocellular carcinoma through negatively regulating SUSD2 Z.-G. SHENG, M.-H. CHEN 1Department of Gastroenterology, Weinan Central Hospital, Weinan, China 2Department of Pharmacy, Hanzhong People’s Hospital, Hanzhong, China Abstract. – OBJECTIVE: The aim of this as well as poor prognosis of HCC patients. By study was to elucidate the role of TPM4 in the negatively targeting SUSD2, TPM4 aggravates progression of hepatocellular carcinoma (HCC), the progression of HCC by accelerating the pro- and to explore the potential underlying mecha- liferative and migratory abilities of HCC cells. nism by interacting with SUSD2. PATIENTS AND METHODS: TPM4 expres- Key Words: sion levels in 41 HCC tissues and paracancer- TPM4, SUSD2, Hepatocellular carcinoma (HCC), ous tissues were detected by quantitative Re- Malignancy. al Time-Polymerase Chain Reaction (qRT-PCR). The relationship between TPM4 level with the pathological indexes and overall survival of HCC patients was analyzed. TPM4 overexpression and knockdown models were constructed in Introduction Bel-7402 and Hep3B cells, respectively. Subse- quently, Cell Counting Kit-8 (CCK-8) and tran- Hepatocellular carcinoma (HCC) is the six swell assay were conducted to assess the ef- most prevalent tumor globally, which ranks fects of TPM4 on the proliferative and migra- third among tumor-related deaths1,2. The number tory abilities of HCC cells. Dual-Luciferase re- of newly onset HCC in China accounts for 54% porter gene assay was performed to verify the 3,4 binding relationship between TPM4 and SUSD2. of global HCC cases . Improvement of surgical In addition, the xenograft model was conducted procedures has largely enhanced the survival in HCC-bearing mice administrated with Hep3B rate of HCC patients. -

Host Cell Factors Necessary for Influenza a Infection: Meta-Analysis of Genome Wide Studies
Host Cell Factors Necessary for Influenza A Infection: Meta-Analysis of Genome Wide Studies Juliana S. Capitanio and Richard W. Wozniak Department of Cell Biology, Faculty of Medicine and Dentistry, University of Alberta Abstract: The Influenza A virus belongs to the Orthomyxoviridae family. Influenza virus infection occurs yearly in all countries of the world. It usually kills between 250,000 and 500,000 people and causes severe illness in millions more. Over the last century alone we have seen 3 global influenza pandemics. The great human and financial cost of this disease has made it the second most studied virus today, behind HIV. Recently, several genome-wide RNA interference studies have focused on identifying host molecules that participate in Influen- za infection. We used nine of these studies for this meta-analysis. Even though the overlap among genes identified in multiple screens was small, network analysis indicates that similar protein complexes and biological functions of the host were present. As a result, several host gene complexes important for the Influenza virus life cycle were identified. The biological function and the relevance of each identified protein complex in the Influenza virus life cycle is further detailed in this paper. Background and PA bound to the viral genome via nucleoprotein (NP). The viral core is enveloped by a lipid membrane derived from Influenza virus the host cell. The viral protein M1 underlies the membrane and anchors NEP/NS2. Hemagglutinin (HA), neuraminidase Viruses are the simplest life form on earth. They parasite host (NA), and M2 proteins are inserted into the envelope, facing organisms and subvert the host cellular machinery for differ- the viral exterior. -

Supplementary Table 5A
CE2/+ f/f CA/+ CE2/+ f/f Supplementary Table 5A: Pathway enrichment analysis for differentially expressed genes between Nkx3.1 ; Pten ; Braf and Nkx3.1 ; Pten mouse prostate tumors Pathway Gene Number Enrichment Normalized p-value False Family-wise Rank Leading Edge Genes Set of genes Score enrichment Discovery Error Rate at Details in the score Rate p-value Max pathway q-value TPM2 ACTG2 MYL9 ACTA2 VCL DES MYLK ITGA1 Details TPM4 SORBS1 CALM2 ITGB5 PXN LMOD1 TNNC2 1 REACTOME_MUSCLE_CONTRACTION ... 30 0.78 2.58 0 0 0 2180 MYL1 MYH11 Details TPM2 ACTG2 MYL9 ACTA2 VCL MYLK ITGA1 2 REACTOME_SMOOTH_MUSCLE_CONTRACTION ... 20 0.81 2.39 0 0 0 1609 TPM4 SORBS1 CALM2 ITGB5 PXN LMOD1 MYH11 ITGA3 LAMB3 ITGB4 THBS1 LAMA3 CD44 ITGA6 ITGAV ITGB1 SPP1 LAMC2 ITGA1 SDC1 RELN LAMC1 FN1 ITGB5 THBS2 COL1A2 ITGA9 ITGB6 SDC2 HSPG2 TNC COL6A1 COL4A2 COL6A2 Details COL4A6 ITGA5 COL4A1 LAMA1SV2B COL5A1 3 KEGG_ECM_RECEPTOR_INTERACTION ... 59 0.63 2.32 0 0 0 3812 COL6A3 COL3A1 ITGA11 COL5A2 ITGA10 Details ACTIN1 FLNC FBLIM1 ITGB1 FLNA RSU1 FERMT2 4 REACTOME_CELLEXTRACELLULAR_MATRIX_INTERACTIONS ... 13 0.81 2.16 0 0 0.001 1193 PXN ILK ITGA3 ITGB4 THBS1 ITGA6 ITGAV ITGB1 SPP1 ITGA1 LAMC1 FN1 ITGB5 COL1A2 CDH1 BCRAR1 ITGA9 ITGB6 COL4A5 TNC COL4A2 ITGA5 COL4A1 Details LAMA1 PTPN1 FGG PECAM1 FGA FBN1 ITGA11 5 REACTOME_INTEGRIN_CELL_SURFACE_INTERACTIONS ... 62 0.57 2.09 0 0 0.002 3812 ITGA10 COL1A1 LAMA2 LAMB2 ITGA3 CCND1 LAMB3 ITGB4 THBS1 FLNB LAMA3 ACTN1 IGF1R CCND2 ITGA6 ITGAV FLNC MYL9 CAV1 ITGB1 VEGF1 PDGFRA SPP1 FLNA MAP2K1 PDGFC VCL PPP1CC MYLK LAMC2 CAPN2 CDC42 ITGA1 RELN LAMC1 AKT3 FN1 CAV2 PDGFRB ITGB5 PXN ILK PDGFB THBS2 DOCK1 COL1A2 FLT1 FIGF BCAR1 ITGA9 ITGB6 PAK3 TNC COL6A1 COL4A2 COL6A2 COL4A6 ITGA5 COL4A1 LAMA1 Details BCL2 COL5A1 PGF ZYX COL6A3 COL3A1 ITGA11 6 KEGG_FOCAL_ADHESION .. -

Transdifferentiation of Human Mesenchymal Stem Cells
Transdifferentiation of Human Mesenchymal Stem Cells Dissertation zur Erlangung des naturwissenschaftlichen Doktorgrades der Julius-Maximilians-Universität Würzburg vorgelegt von Tatjana Schilling aus San Miguel de Tucuman, Argentinien Würzburg, 2007 Eingereicht am: Mitglieder der Promotionskommission: Vorsitzender: Prof. Dr. Martin J. Müller Gutachter: PD Dr. Norbert Schütze Gutachter: Prof. Dr. Georg Krohne Tag des Promotionskolloquiums: Doktorurkunde ausgehändigt am: Hiermit erkläre ich ehrenwörtlich, dass ich die vorliegende Dissertation selbstständig angefertigt und keine anderen als die von mir angegebenen Hilfsmittel und Quellen verwendet habe. Des Weiteren erkläre ich, dass diese Arbeit weder in gleicher noch in ähnlicher Form in einem Prüfungsverfahren vorgelegen hat und ich noch keinen Promotionsversuch unternommen habe. Gerbrunn, 4. Mai 2007 Tatjana Schilling Table of contents i Table of contents 1 Summary ........................................................................................................................ 1 1.1 Summary.................................................................................................................... 1 1.2 Zusammenfassung..................................................................................................... 2 2 Introduction.................................................................................................................... 4 2.1 Osteoporosis and the fatty degeneration of the bone marrow..................................... 4 2.2 Adipose and bone