Muscle Structure and Function in Older Adults with a Rotator
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Build a Plane That Cuts Smooth and Crisp Raised Panels With, Against Or Across the Grain – the Magic Is in the Spring and Skew
Fixed-width PanelBY WILLARD Raiser ANDERSON Build a plane that cuts smooth and crisp raised panels with, against or across the grain – the magic is in the spring and skew. anel-raising planes are used Mass., from 1790 to 1823 (Smith may to shape the raised panels in have apprenticed with Joseph Fuller doors, paneling and lids. The who was one of the most prolific of the profile has a fillet that defines early planemakers), and another similar Pthe field of the panel, a sloped bevel example that has no maker’s mark. to act as a frame for the field and a flat Both are single-iron planes with tongue that fits into the groove of the almost identical dimensions, profiles door or lid frame. and handles. They differ only in the I’ve studied panel-raising planes spring angles (the tilt of the plane off made circa the late 18th and early 19th vertical) and skew of the iron (which centuries, including one made by Aaron creates a slicing cut across the grain to Smith, who was active in Rehoboth, reduce tear-out). The bed angle of the Smith plane is 46º, and the iron is skewed at 32º. Combined, these improve the quality of cut without changing the tool’s cutting angle – which is what happens if you skew Gauges & guides. It’s best to make each of these gauges before you start your plane build. In the long run, they save you time and keep you on track. Shaping tools. The tools required to build this plane are few, but a couple of them – the firmer chisel and floats – are modified to fit this design. -

De Quervain's Tenosynovitis
GUIDE TO THE DIAGNOSIS OF WORK-RELATED MUSCULOSKELETAL 2 DISORDERS Work-related musculoskeletal injuries are one of the most common occupational health problems for which physicians are consulted. There is solid scientific evidence that these injuries may be occupational in origin. This guide was designed to help physicians interpret the results of a medical examination. By combining the standard clinical assessment procedure with guidelines concerning the identification of etiological factors, it helps physicians identify the cause of injury. AUTHORS Louis Patry holds a degree in medicine from Laval University and a diploma in ergonomics from the Conservatoire National des Arts De Quervain’s et Metiers de Paris (CNAM). He is a specialist in occupational medi- De Quervain’s cine, an associate member of the Royal College of Physicians and Surgeons of Canada, a professor in McGill University’s Department of Epidemiology and Biostatistics and Occupational Health, and con- sulting physician to the Direction de la santé publique (Public Health Department), first in Québec City and currently at the Montréal- TenosynovitisTenosynovitis Centre board. Michel Rossignol holds degrees in biochemistry and medicine from the University of Sherbrooke, in epidemiology and community Louis PATRY, Occupational Medecine Physician, Ergonomist health from McGill University, and in occupational medicine from Michel ROSSIGNOL, Occupational Medecine Physician, Epidemiologist John Hopkins University. He is a professor in McGill University’s Department of Epidemiology and Biostatistics and Occupational Marie-Jeanne COSTA, Nurse, Ergonomist Health, co-director of the Centre for Clinical Epidemiology of the Jewish General Hospital of Montréal, and physician-epidemiologist Martine BAILLARGEON, Plastic Surgeon at the Montréal-Centre board of the Direction de la santé publique (Public Health Department). -

Howard Brady
Howard Brady WOOD DESIGNS Copyright © 2019 by Howard L. Brady Note: Every item shown in this album was an original, one-of-a-kind design. The design process from concept through crafting to the finished item is a source of incredible satisfaction to me, and a process that extends well beyond woodworking into music composition, and (with my brother) creation of innovative educational materials. A few years before I retired, Dave Campbell, a senior engineer and friend at Skydata where I worked, remarked that as a writer of technical communications documents for satellite communications equipment, I was an “information designer.” Those were kind works, and, I hope, accurate. This octogenarian loves designing. ii Toys for my great-grandson, Mason: The front-end loader and dump truck were my first major toy designs, built November 2017. Most solid wood is poplar, plywood parts are Baltic birch, dark wood is Indian rosewood, from a local tree destroyed in one of the 2004 hurricanes. Metal parts were aluminum (truck bed edge rails, front end loader bucket and crosspiece), brass (truck steering components) and stainless steel (all fasteners, operating levers). Lever and knob above truck cab controls steering. 1 Built March 2018: Toy box for Mason’s third birthday, May 6th: 2 November 2018: Toy flat-bed wrecker and grumpy wrecked race car for Mason’s Christmas. One of Mason’s parent’s close friends is Tim Daugherty, who races his #88 car (so far NOT wrecked) in figure-8 races at the Antelope Valley Fairgrounds in Southern California. I hope he didn’t mind my version. -
Immediate and Short-Term Effects of Kinesiotaping on Muscular Activity
Reynard et al. BMC Musculoskeletal Disorders (2018) 19:305 https://doi.org/10.1186/s12891-018-2169-5 RESEARCH ARTICLE Open Access Immediate and short-term effects of kinesiotaping on muscular activity, mobility, strength and pain after rotator cuff surgery: a crossover clinical trial Fabienne Reynard1* , Philippe Vuistiner2, Bertrand Léger2 and Michel Konzelmann3 Abstract Background: Kinesiotape (KT) is widely used in musculoskeletal rehabilitation as an adjuvant to treatment, but minimal evidence supports its use. The aim of this study is to determine the immediate and short-term effects of shoulder KT on muscular activity, mobility, strength and pain after rotator cuff surgery. Methods: Thirty-nine subjects who underwent shoulder rotator cuff surgery were tested 6 and 12 weeks post-surgery, without tape, with KT and with a sham tape (ST). KT and ST were applied in a randomized order. For each condition, the muscular activity of the upper trapezius, three parts of the deltoid and the infraspinatus were measured during shoulder flexion, and range of motion (ROM) and pain intensity were assessed. At 12 weeks, the isometric strength at 90° of shoulder flexion, related muscular activity and pain intensity were also measured. Subjects maintained the last tape that was applied for three days and recorded the pain intensity at waking up and during the day. Results: Modifications in muscle activity were observed with KT and with ST. Major changes in terms of decreased recruitment of the upper trapezius were observed with KT (P < 0.001). KT and ST also increased flexion ROM at 6 weeks (P = 0.004), but the differences with the no tape condition were insufficient to be clinically important. -

Musicians and MSI: Symptoms and Types of Injuries
Musicians and MSI: Symptoms and types of injuries Musculoskeletal injury (MSI) is any injury or disorder of There is also a predominant medical perspective that the muscles, bones, joints, tendons, ligaments, nerves, MSI is neither life-threatening nor medically serious. blood vessels, or related soft tissues. This includes a However, an MSI can be artistically and professionally strain, sprain, or inflammation that is caused or limiting, or even career-ending, with devastating effects aggravated by activity. on your physical, emotional, and financial well-being. If you experience pain that may indicate MSI, take steps to Musicians (including vocalists) are prone to MSI that is deal with the problem. caused or aggravated by practice, rehearsal, or performance. Playing a musical instrument may be Table 1 describes five levels of MSI signs and symptoms in second only to computer use in terms of population performers. If you are at Level I or II, modify your exposure to an MSI risk factor. Some studies have shown activities to prevent further progression of symptoms. If that approximately half of professional musicians and you are at Level III or higher, seek professional assistance. music students experience significant MSI symptoms. Table 1 Progression of MSI signs and symptoms To find out more about MSI, see the information sheet Level I “Musicians and MSI — Prevention and Treatment.” Pain occurs after class, practice, rehearsal, or performance, but you are able to perform normally. MSI symptoms Level II Pain occurs during class, practice, If you develop an MSI, you may experience symptoms rehearsal, or performance, but you are not restricted in performing. -

Trauma and Reiter's Syndrome: Development of 'Reactive Arthropathy' in Two Patients Following Musculoskeletal Injury
Ann Rheum Dis: first published as 10.1136/ard.43.6.829 on 1 December 1984. Downloaded from Annals of the Rheumatic Diseases, 1984, 43, 829-832 Trauma and Reiter's syndrome: development of 'reactive arthropathy' in two patients following musculoskeletal injury JEFFREY J. WISNIESKI From the Medical Service, Rheumatology Section, Cleveland Veterans Administration Medical Center, and Case Western Reserve University School of Medicine, Cleveland, Ohio, USA. SUMMARY Two patients are reported who developed arthropathies with some features of Reiter's syndrome shortly after physical injury. Both were HLA-B27 positive. No other precipitating factors were identified, and the possibility that trauma may have precipitated a reactive arth- ropathy is discussed. Key words: endogenous antigen (immunogen), genetic predisposition, collagen. copyright. Concepts of Reiter's syndrome (RS) have changed swelling, pain, and heat; internal mechanical dramatically in the past decade. Notable develop- derangement was suspected. Five months after the ments include: (1) recognition that clinical activity trauma arthroscopy revealed hyperaemic and thick- may be acute/self-limited, acute/recurrent, or ened synovium but no structural abnormality. Syno- chronic'-5; (2) recognition that disease mani- vial biopsy showed chronic synovitis with marked festations vary from 'incomplete' RS to multisystem lymphocyte and plasma cell infiltration. involvement'-3; (3) development of concepts of Seven months after the injury the knee continued genetic predisposition and linkage4 5; and (4) charac- to be warm and painful, with thickened synovium and http://ard.bmj.com/ terisation of RS as reactive arthritis developing in a large effusion. No other joints were involved. Con- genetically predisposed individuals.45 In most junctivitis of the left eye was noted. -
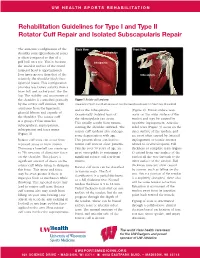
Rehabilitation Guidelines for Type I and Type II Rotator Cuff Repair and Isolated Subscapularis Repair
UW HEALTH SPORTS REHABILITATION Rehabilitation Guidelines for Type I and Type II Rotator Cuff Repair and Isolated Subscapularis Repair The anatomic configuration of the Back View Front View shoulder joint (glenohumeral joint) Supraspinatus is often compared to that of a golf ball on a tee. This is because Infraspinatus the articular surface of the round humeral head is approximately Teres four times greater than that of the Minor Subscapularis relatively flat shoulder blade face (glenoid fossa). This configuration provides less boney stability than a truer ball and socket joint, like the hip. The stability and movement of the shoulder is controlled primarily Figure 1 Rotator cuff anatomy by the rotator cuff muscles, with Image property of Primal Pictures, Ltd., primalpictures.com. Use of this image without authorization from Primal Pictures, Ltd. is prohibited. assistance from the ligaments, and/or the infraspinatus. (Figure 2). Bursal surface tears glenoid labrum and capsule of Occasionally isolated tears of occur on the outer surface of the the shoulder. The rotator cuff the subscapularis can occur. tendon and may be caused by is a group of four muscles: This usually results from trauma repetitive impingement. Articular subscapularis, supraspinatus, rotating the shoulder outward. The sided tears (Figure 3) occur on the infraspinatus and teres minor rotator cuff tendons also undergo inner surface of the tendon, and (Figure 1). some degeneration with age. are most often caused by internal Rotator cuff tears can occur from This process alone can lead to impingement or tensile stresses repeated stress or from trauma. rotator cuff tears in older patients. related to overhead sports. -

Modern Repair Techniques for Rotator Cuff Tears
Current Reviews in Musculoskeletal Medicine (2018) 11:113–121 https://doi.org/10.1007/s12178-018-9465-4 ROTATOR CUFF REPAIR (M TAO AND M TEUSINK, SECTION EDITORS) Partial and Full-Thickness RCT: Modern Repair Techniques Amit Nathani1 & Kevin Smith1 & Tim Wang1 Published online: 22 January 2018 # Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Purpose of Review The purpose of this article is to review the recent literature concerning modern repair techniques related to partial- and full-thickness rotator cuff tears. Recent Findings The understanding of rotator cuff pathology and healing continues to evolve, beginning with emerging descrip- tions of the anatomic footprint and natural history of rotator cuff tears. Significant controversy remains in treatment indications for partial-thickness rotator cuff lesions as well as optimal surgical repair techniques for both partial- and full-thickness tears. Techniques such as margin convergence and reduction of the so-called “comma” tissue have improved the ability to anatomically reduce large and retracted tears. Repair strength and contact pressures are improved with double-row repairs and transosseus- equivalent techniques compared to traditional single-row repairs. Future work is directed towards obtaining reliable radiographic healing and demonstrating clinical superiority and cost-effectiveness of a single technique. Summary Much recent work regarding rotator cuff anatomy and pathology has been reported. Newer techniques improve repair strength. Despite these advances, significant questions remain concerning surgical indications and clinical outcomes. Keywords Rotator cuff . Repair . Anatomy . Technique . Review . Outcomes Introduction muscle degeneration and atrophy, which may preclude suc- cessful surgical repair [4•, 5, 6]. Rotator cuff tears are a very common musculoskeletal injury Much of the work the past two decades regarding rotator and source of disability in the shoulder. -
SHAKERWORKBENCH Design, Construction Notes and Techniques
BENCHCRAFTED · SHAKER BENCH PLANS SHAKERWORKBENCH Design, Construction Notes and Techniques “Don't make something unless it is both necessary and useful; but if it is both neces- sary and useful, don't hesitate to make it beautiful." –Shaker Dictum Introduction and Design: Ron Brese Construction Notes and Techniques: Jameel Abraham Measured Drawings: Louis Bois Copyright Benchcrafted 2011·2014 No unauthorized reproduction or distribution. You may print copies for your own personal use only. 1 BENCHCRAFTED · SHAKER BENCH PLANS · INTRODUCTION & DESIGN · “Whatever perfections you may have, be assured people will find them out, but whether they do or not, nobody will take them on your word” Canterbury, New Hampshire, 1844 When I first laid eyes on the workbench at the Hancock Shaker Museum in Pittsfield, Massachusetts I had a pretty good idea of the configuration of my next workbench. I think it would be safe to say that I was inspired. However, designing a workbench that is inspired by a Shaker icon can be intimidating as well. I had to do justice to the original and keep in mind what might be considered acceptable. Luckily, most are aware that the Shakers were quite accepting of new technologies that could be practically applied, so this did allow a fair amount of leeway in regards to using more recent workholding devices on this bench. In the end, I did want the look to be very representative of the Shaker Ideal. “‘Tis a Gift to Be Simple” is an over used Shaker pronouncement, however I often think it’s meaning is misinterpreted. I believe it means having freedom from making things unnecessarily complicated. -

An Ultrasonographic Analysis of the Structures of the Subacromial Space, As They Relate to the Postures of Upper String Musicians Elliot V
Marshall University Marshall Digital Scholar Theses, Dissertations and Capstones 2016 An Ultrasonographic Analysis of the Structures of the Subacromial Space, as They Relate to the Postures of Upper String Musicians Elliot V. Smithson [email protected] Follow this and additional works at: http://mds.marshall.edu/etd Part of the Musculoskeletal Diseases Commons, Musculoskeletal, Neural, and Ocular Physiology Commons, and the Sports Sciences Commons Recommended Citation Smithson, Elliot V., "An Ultrasonographic Analysis of the Structures of the Subacromial Space, as They Relate to the Postures of Upper String Musicians" (2016). Theses, Dissertations and Capstones. Paper 994. This Thesis is brought to you for free and open access by Marshall Digital Scholar. It has been accepted for inclusion in Theses, Dissertations and Capstones by an authorized administrator of Marshall Digital Scholar. For more information, please contact [email protected], [email protected]. AN ULTRASONOGRAPHIC ANALYSIS OF THE STRUCTURES OF THE SUBACROMIAL SPACE, AS THEY RELATE TO THE POSTURES OF UPPER STRING MUSICIANS A thesis submitted to the Graduate College of Marshall University In partial fulfillment of the requirements for the degree of Master of Science in Athletic Training by Elliot V. Smithson Approved by Dr. Mark K. Timmons, Committee Chairperson Dr. Gary McIlvain Dr. Elizabeth Reed Smith Marshall University May 2016 i APPROVAL OF THESIS/DISSERTATION We, the faculty supervising the work of Elliot V. Smithson, affirm that the thesis, An Ultrasonographic Analysis of the Structures of the Subacromial Space, As They Relate to the Postures of Upper string Musicians, meets the high academic standards for original scholarship and creative work established by the Master’s of Athletic Training Program and the Marshall University School of Kinesiology. -

Arterial Supply to the Rotator Cuff Muscles
Int. J. Morphol., 32(1):136-140, 2014. Arterial Supply to the Rotator Cuff Muscles Suministro Arterial de los Músculos del Manguito Rotador N. Naidoo*; L. Lazarus*; B. Z. De Gama*; N. O. Ajayi* & K. S. Satyapal* NAIDOO, N.; LAZARUS, L.; DE GAMA, B. Z.; AJAYI, N. O. & SATYAPAL, K. S. Arterial supply to the rotator cuff muscles.Int. J. Morphol., 32(1):136-140, 2014. SUMMARY: The arterial supply to the rotator cuff muscles is generally provided by the subscapular, circumflex scapular, posterior circumflex humeral and suprascapular arteries. This study involved the bilateral dissection of the scapulohumeral region of 31 adult and 19 fetal cadaveric specimens. The subscapularis muscle was supplied by the subscapular, suprascapular and circumflex scapular arteries. The supraspinatus and infraspinatus muscles were supplied by the suprascapular artery. The infraspinatus and teres minor muscles were found to be supplied by the circumflex scapular artery. In addition to the branches of these parent arteries, the rotator cuff muscles were found to be supplied by the dorsal scapular, lateral thoracic, thoracodorsal and posterior circumflex humeral arteries. The variations in the arterial supply to the rotator cuff muscles recorded in this study are unique and were not described in the literature reviewed. Due to the increased frequency of operative procedures in the scapulohumeral region, the knowledge of variations in the arterial supply to the rotator cuff muscles may be of practical importance to surgeons and radiologists. KEY WORDS: Arterial supply; Variations; Rotator cuff muscles; Parent arteries. INTRODUCTION (Abrassart et al.). In addition, the muscular parts of infraspinatus and teres minor muscles were supplied by the circumflex scapular artery while the tendinous parts of these The rotator cuff is a musculotendionous cuff formed muscles received branches from the posterior circumflex by the fusion of the tendons of four muscles – viz. -

Better Tenons
BETTER TENONS © 2017 Cruz Bay Publishing, Inc. tips & techniques for Better Tenons Mortise and tenon joinery is a hallmark of the key details. The drawing and pho- The other detail that I key in on is a of solid, long-lasting construction. To tos below highlight what you’re after. tight, even seam around the shoulders. improve your skills, it’s helpful to take For me, there are two main points of This looks good, but it also resists the some time to zero in on one part of the attention: First, the connection between forces that try to lever the pieces apart. process. Here, let’s take a look at how to the wide cheeks of the tenon and the As for the fit of the tenon at the ends of raise your tenon-making game. long-grain walls of the mortise. This gives the mortise, I’m not concerned about that. YOUR TARGET. Before you get to the the joint its strength. The other surfaces In fact, a little gap here gives you some nitty-gritty of making and fine- have at least one end-grain component wiggle room to align parts at assembly. tuning the fit of a tenon, I find and contribute very little to the overall Another aspect you don’t need to it helpful to have an idea strength of the joint. worry about is making the length of the Chamfered edges allow the tenon to slide in easier Gap on short shoulders allows you to align parts better Wide cheeks provide strongest glue surface Tenon cut short Stile cut away so it to show doesn't mortise and bottom tenon joint out in mortise { A properly sized tenon should fit into { Another test for a tenon is to dry fit the joint the mating mortise with moderate hand and raise the mortised piece.