This Is Your Products Liability Restatement on Drugs Lars Noah
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
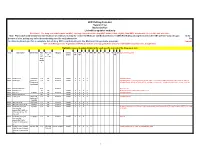
Drug Code List
HCPCS/Drug Code List Version 13.2 Revised 6/1/21 List will be updated routinely Disclaimer: For drug codes that require an NDC, coverage depends on the drug NDC status (rebate eligible, Non-DESI, non-termed, etc) on the date of service. Note: Physician/Facility-administered medications are reimbursed using the Centers for Medicare and Medicaid Services (CMS) Part B Drug pricing file found on the CMS website--www.cms.gov. In the absence of a fee, pricing may reflect the methodolgy used for retail pharmacies. Go to data.medicaid.gov for a complete list of drug NDCs participating in the Medicaid drug rebate program. Consult with each Managed Care Organization (MCO) about their coverage guidelines and prior authroization requirements, if applicable. Highlights represent updated material for each specific revision of the Drug Code List. Code Description Brand Name NDC NDC unit Category Service AC CAH P NP MW MH HS PO OPH HI ID DC Special Instructions req. of Limits OP OP TF for measure drug rebate ? 90281 human ig, im Gamastan Yes ML Antisera NONE X X X X Closed 3/31/13. 90283 human ig, iv Gamimune, Yes ML Antisera NONE X X X X Closed 3/31/13. Cost invoice required with claim. Restricted to ICD-9 diagnoses codes 204.10 - 204.12, Flebogamma, 279.02, 279.04, 279.06, 279.12, 287.31, and 446.1, and must be included on claim form, effective 10/1/09. Gammagard 90287 botulinum antitoxin N/A Antisera Not Covered 90288 botulism ig, iv No ML NONE X X X X Requires documentation and medical review 90291 cmv ig, iv Cytogam Yes ML Antisera NONE X X X X Closed 3/31/13. -

Pharmaceutical Patient Safety Policy (PM509)
Original Department: Pharmacy 09/12/2007 Approval: Policy #: PM509 Last Approval: 12/10/2020 Title: Pharmaceutical Patient Safety Approved By: Medical Management Leadership Team Dependencies: None Line(s) of Business WAH-IMC (HCA) BHSO Medicare Advantage (CMS) Medicare SNP (CMS) Cascade Select Purpose Community Health Plan of Washington (CHPW) is committed to ensuring pharmaceutical patient safety. For this reason, in conjunction with its pharmacy benefit manager (PBM), CHPW has established the following programs for all lines of business: • Concurrent Drug Utilization Review (DUR) • Retrospective Drug Utilization Review (DUR) • Drug Recall Safety Alerts Policy CHPW, in conjunction with its PBM, maintains a Concurrent Drug Utilization Review (DUR) at the point- of-dispensing. The goal of the Concurrent DUR is to serve as a secondary source of pharmaceutical information designed to enhance patient safety and to identify the most relevant drug interactions that could impact patient care and potentially result in an adverse drug reaction. In addition, CHPW alerts physicians and members about significant patient-safety related issues including, but not limited to, market withdrawals1, black box warnings2, and class I recalls3. CONCURRENT DUR The Concurrent DUR system is a clinically-based real-time process. The Concurrent DUR system that CHPW and its PBM use follows criteria standards found in 42 C.F.R 456.703(f)(1). It takes place during the claims adjudication process and is designed to identify important patient- specific pharmaceutical care concerns through the use of the following 13 modules: 1 Market withdrawal occurs when a product has a minor violation that would not be subject to FDA legal action. -

Drug Recall: an Incubus for Pharmaceutical Companies and Most Serious Drug Recall of History
Review Article Drug recall: An incubus for pharmaceutical companies and most serious drug recall of history Upendra Nagaich, Divya Sadhna1 Departments of Pharmaceutics and 1Drug Regulatory Affairs, Amity Institute of Pharmacy, Amity University, Noida, Uttar Pradesh, India Abstract There has been an increasing trend in the number of prescribed and over-the-counter drug recall over the last few years. The recall is usually due to company’s discovery, customer’s complaint or Food and Drug Administration (FDA) observation. The process of recall involves a planned specific course of action, which addresses the depth of recall, need for public warning, and the extent of effectiveness checks for the recall. The FDA review and/or recommend changes to the firm’s recall strategy, as appropriate. The critical recall information list includes the identity of the product; summary of the failure; amount of product produced in the distribution chain and direct account. Product recalls clashes thousands of companies every year affecting: sales, testing customer relationships and disrupting supply chains. Drug recall is incubus for pharmaceutical companies. It effects the reputation of the company. The reason for the recall can be divided into two categories: manufacturing affined and safety/efficacy affined. It is essential to follow all the guidelines related to drug development and manufacturing procedure so as to minimize drug recall. Key words: Drug product recall, guidelines, process, recall information INTRODUCTION Regardless a company’s best exists that dangerously defective drug product may reach the customers. These products may cause A drug recall is an instance to return to the maker a batch or disasters, leading to adverse verdicts in drug product liability an entire production run of a drug product, usually due to the litigations. -

Annual Report 2020
2020 ANNUAL REPORT WAAX at Valley Fiesta. Photo by Dave Kan. OUR VISION To support and promote a thriving contemporary live and recorded music industry that transforms lives and delivers artistic, cultural, social and economic value to Queensland. QMUSIC 3/374 Brunswick Street PO Box 878 Fortitude Valley Qld 4006 Australia T (07) 3257 0013 E [email protected] W www.qmusic.com.au Queensland Music Network Incorporated ABN 14 083 014 720 CONTENTS PRESIDENT’S REPORT ...............................................................................................................................4 CEO’S REPORT ....................................................................................................................................................6 FIRST NATIONS PROGRAMMER AND PRODUCER REPORT .......8 PROGRAMMING .......................................................................................................................................10 PROGRAM OF ACTIVITIES ..........................................................................................................11 INDUSTRY ADVOCACY ....................................................................................................................27 PARTNERSHIPS ...............................................................................................................................................29 QMUSIC FEATURES ...............................................................................................................................30 QMUSIC’S REACH ....................................................................................................................................36 -

Triple J Hottest 100 of the Decade Voting List: AZ Artists
triple j Hottest 100 of the Decade voting list: A-Z artists ARTIST SONG 360 Just Got Started {Ft. Pez} 360 Boys Like You {Ft. Gossling} 360 Killer 360 Throw It Away {Ft. Josh Pyke} 360 Child 360 Run Alone 360 Live It Up {Ft. Pez} 360 Price Of Fame {Ft. Gossling} #1 Dads So Soldier {Ft. Ainslie Wills} #1 Dads Two Weeks {triple j Like A Version 2015} 6LACK That Far A Day To Remember Right Back At It Again A Day To Remember Paranoia A Day To Remember Degenerates A$AP Ferg Shabba {Ft. A$AP Rocky} (2013) A$AP Rocky F**kin' Problems {Ft. Drake, 2 Chainz & Kendrick Lamar} A$AP Rocky L$D A$AP Rocky Everyday {Ft. Rod Stewart, Miguel & Mark Ronson} A$AP Rocky A$AP Forever {Ft. Moby/T.I./Kid Cudi} A$AP Rocky Babushka Boi A.B. Original January 26 {Ft. Dan Sultan} Dumb Things {Ft. Paul Kelly & Dan Sultan} {triple j Like A Version A.B. Original 2016} A.B. Original 2 Black 2 Strong Abbe May Karmageddon Abbe May Pony {triple j Like A Version 2013} Action Bronson Baby Blue {Ft. Chance The Rapper} Action Bronson, Mark Ronson & Dan Auerbach Standing In The Rain Active Child Hanging On Adele Rolling In The Deep (2010) Adrian Eagle A.O.K. Adrian Lux Teenage Crime Afrojack & Steve Aoki No Beef {Ft. Miss Palmer} Airling Wasted Pilots Alabama Shakes Hold On Alabama Shakes Hang Loose Alabama Shakes Don't Wanna Fight Alex Lahey You Don't Think You Like People Like Me Alex Lahey I Haven't Been Taking Care Of Myself Alex Lahey Every Day's The Weekend Alex Lahey Welcome To The Black Parade {triple j Like A Version 2019} Alex Lahey Don't Be So Hard On Yourself Alex The Astronaut Not Worth Hiding Alex The Astronaut Rockstar City triple j Hottest 100 of the Decade voting list: A-Z artists Alex the Astronaut Waste Of Time Alex the Astronaut Happy Song (Shed Mix) Alex Turner Feels Like We Only Go Backwards {triple j Like A Version 2014} Alexander Ebert Truth Ali Barter Girlie Bits Ali Barter Cigarette Alice Ivy Chasing Stars {Ft. -

Remixing Music Copyright to Better Protect Mashup Artists Kerri Eble
EBLE.DOCX (DO NOT DELETE) 3/29/2013 2:34 PM THIS IS A REMIX: REMIXING MUSIC COPYRIGHT TO BETTER PROTECT MASHUP ARTISTS KERRI EBLE Modern copyright law has strayed from its original purpose as set out in the Constitution and is ill-equipped to protect and foster new forms of artistic expression. Since the last major amendment to the Copyright Act, new art forms have arisen, particularly “mashup music.” This type of music combines elements of other artists’ songs with other sounds to create a new artistic work. Under modern copy- right law, various courts treat this type of music inconsistently, creat- ing uncertainty among mashup artists and stifling this new artistic ex- pression. In addition, copyright law, as applied to music, unduly favors primary artists, sacrificing the Copyright Clause’s focus on preserving the public domain. This Note discusses the history of mashup music and its increas- ing popularity in the United States, as well as the relevant history of copyright law. This Note then discusses current safe harbors that ex- ist under copyright law for secondary artists and analyzes why mashups do not fit within these safe harbors. This Note concludes by recommending that the fair use exception be expanded to protect mashup artists by adding a safe harbor for “recontextualized” or “re- designed” artworks. I. INTRODUCTION Everything is breaking down in a good way. Once upon a time . there was a line. You know, the edge of the stage was there. The performers are on one side. The audience is on the oth- er side, and never the twain shall meet. -

Lawyer Leads Fight Against Modern Slavery Ode To
EDITION 2 2014 LAWYER LEADS WHERE DO BIG FISH ODE TO RESILIENT, FIGHT AGAINST GO IN THE CONTRADICTORY MODERN SLAVERY WET SEASON? DARWIN EDITION 2 2014 ORIGINS FEATURES REGULARS Lawyer leads fight 3 8 against modern slavery From the Vice-Chancellor 4 Social ills grow as goals Snapshot 10 move out of sight 26 Q and A 12 Partners in slime 28 CDU publishing achievements Where do big fish go in 14 the wet season? 30 CDU art collection Picture emerges of 31 16 northern dolphins Art exhibition Neridah Stockley: a retrospective Welcome to the first Charles Darwin Scholar 19 32 Limited edition Refreshing research 20 targets heat stress Finding hope for the 22 future in the past Ode to resilient, 24 contradictory Darwin Young musician 29 reaches for the sky ORIGINS Origins magazine is produced by Charles Darwin University’s Office of Media, Advancement and Community Engagement (MACE). MACE is grateful to the following people for their contributions and assistance in compiling this edition: Lucy Barnard, Penelope Bergen, Matt Brearley, Janet Browne, Bobby Bunungurr, David Crook, Carla Eisemberg, John Firth-Smith, CONTRIBUTORS Felicity Gerry, Dan Hartney, Amy Kimber, Michael Lawrence-Taylor, Tess Lea, Michael Lindsey, KATIE WEISS Robyn Marsh, Hana Morrissey, Simon Moss, Elspeth Opperman, Carol Palmer, Heidi Smith- One of the newest writers to join Origins is Charles Vaughan, Neridah Stockley and Ruth Thornton. Darwin University’s Media Officer Katie Weiss. Katie recently moved to Darwin and was formerly a Opinions and views expressed in this edition do journalist with the mainstream media. Her writing not necessarily reflect those of Charles Darwin has featured in a range of publications nationally University. -

Code of Alabama 1975
CODE OF ALABAMA 1975 CUMULATIVE SUPPLEMENT INCLUDING ACT OF 2009 LEGISLATURE TITLE 34 CHAPTER 23 PRACTICE OF PHARMACY ACT 205 LEGISLATURE 1966 ALABAMA STATE BOARD OF PHARMACY December 7, 2009 1 PHARMACISTS AND PHARMACIES Article 1. Sec. General Provisions 34-23-1. Definitions. 34-23-2. Objects and purposes of chapter. 34-23-3. State drug inspectors. 34-23-4. Recognition of schools and colleges of pharmacy. 34-23-5. Pharmacists exempt from jury duty. 34-23-6. Bankruptcy sales, auction sales, etc., of drugs and medicines. 34-23-7. Illegal possession of prescription drugs. 34-23-8. Substitution of drugs or brands of drugs. 34-23-9. Purity of drugs dispensed. 34-23-10. Notification by pharmacists of change of employment. 34-23-11. Physicians, dentists, registered nurses, etc., exempt from chapter. 34-23-12. Injunctions against violations of chapter. 34-23-13. Penalty for practicing pharmacy without a license; compounding or dispensing prescriptions by unauthorized persons; violations of chapter or rules and regulations of board. Article 2. Licenses and Permits. Division 1. General Provisions. 34-23-30. Pharmacy permits generally. 34-23-31. Permits for mail-order houses. 34-23-32. Manufacturer, bottler, packer, repackager, or wholesale distributor of drugs. 34-23-32.1 FDA requirements to be adhered to by affected parties. 34-23-33. Revocation or suspension of licensed pharmacist, holder of pharmacy intern or extern certificate, permit to operate - Grounds. 34-23-34. Revocation or suspension of licenses to practice pharmacy and pharmacy permits – Statement of charges and notice of hearing. Division 2. Pharmacists' Licenses. -

Reproductive Health & Wellness Program RHWP Title X Clinical
Reproductive Health & Wellness Program RHWP Title X Clinical Services & Protocols 2021 Ohio Department of Health Reviewed by: Cynthia Shellhas MD, MPH March 2021 1 TABLE OF CONTENTS SECTION 1 – Providing Quality Family Planning Services Introduction Introduction……………………………………………………………………………………... 6 Service Plans and Protocols…………………………………………………………………….. 7 Procedural Outline……………………………………………………………………………… 8 Client Encounters……………………………………………………………………………….. 10 Checklist of FP and Related Preventative Health Services for Women………………………... 11 Checklist of FP and Related Preventative Health Services for Men…………………………… 12 Family Planning Services Contraceptive Services…………………………………………………………………………. 13 Broad Range of Contraceptives………………………………………………………………. 13 The Clinic Visit……………………………………………………………………………….. 14 Physical and Laboratory Assessment………………………………………………………… 15 Client Education and Counseling…………………………………………………………….. 16 Contraceptive Counseling to Adolescent Clients…………………………………………….. 17 Counseling Returning Clients………………………………………………………………… 18 Preventative Health Promotion and Referral…………………………………………………. 18 Preconception Health Services Medical History for Female Clients………………………………………………………….. 18 Medical History for Male Clients……………………………………………………………. 19 Physical Examination for all Clients…………………………………………………………. 19 Client Plan and Education……………………………………………………………………. 19 Referral……………………………………………………………………………………….. 20 Achieving Pregnancy Services Client Assessment…………………………………………………………………………….. 20 Client Education and Counseling……………………………………………………………. -

Ed 064 811 Author Title Institution Pub Date Note
DOCUMENT RESUME ED 064 811 EC 042 255 AUTHOR Segal, Julius, Ed. TITLE Mental Health Program Reports - 5. INSTITUTION Health Services and Mental Health Administration (DREW), Bethesda, Md. PUB DATE Dec 71 NOTE 397p. AVAILABLE FROMSuperintendent of Documents, U. S. Government Printing Office, Washington, D. C. 20402 ($1.75) EDRS PRICE MF-$0.65 HC-$13.16 DESCRIPTORS Child Abuse; Disadvantaged Youth; Drug Abuse; *Emotionally Disturbed; *Exceptional Child Education; Feedback; *Mental Health; Mental Health Clinics; Physiology; Program Descriptions; *Research Projects; *Services ABSTRACT The volume is reported to reflect the broad range of National Institute of Mental Health activities in areas of research, development of mental health manpower, and delivery of mental health services. Twenty papers examine, respectively, relationship of life histories and biochemistry of siblings and twins to schizophrenia, training of Navaho medicine men, development of intelligence in babies, studies of child abuse and infant accidents, community mental health center in Appalachia, educating new leaders via Operation Hope, manner in which social organization of animal communities can lead to a population crisis destroying them, community mental health center in the San Francisco westside, nonprofessionals serving aged public housing tenants, nursery schools in service of mental health, followup survey of long term effects of lysergic acid diethylamide, preschool program for disadvantaged children, infant stimulation as part of well baby care in a disadvantaged area, mental illness and competency to stand trial, studying consciousness with physiological feedback technique, voluntary control of internal states, asymmetry of huran brain and implications for training, controlling brain functions, controlling autonomic functions, and drug abuse. (CB) 111IIIII SCOPE OF INTEREST NOTICE The ERIC Facility has assigned this docum ocessing to: .1 .. -

Triple J's 2017 Hottest 100 Songs No. Song Artist 1 HUMBLE. Kendrick
FOR IMMEDIATE RELEASE: Saturday 27 January 2018 triple j's 2017 Hottest 100 songs No. Song Artist 1 HUMBLE. Kendrick Lamar 2 Let Me Down Easy Gang Of Youths 3 Chateau Angus & Julia Stone 4 Ubu Methyl Ethel 5 The Deepest Sighs, The Frankest Shadows Gang Of Youths 6 Green Light Lorde 7 Go Bang PNAU 8 Sally {Ft. Mataya} Thundamentals 9 Lay It On Me Vance Joy 10 What Can I Do If The Fire Goes Out? Gang Of Youths 11 SWEET BROCKHAMPTON 12 Fake Magic Peking Duk & AlunaGeorge 13 Young Dumb & Broke Khalid 14 Homemade Dynamite Lorde 15 Regular Touch Vera Blue 16 Feel The Way I Do The Jungle Giants 17 Marryuna {Ft. Yirrmal} Baker Boy 18 Exactly How You Are Ball Park Music 19 The Man The Killers 20 Let You Down {Ft. Icona Pop} Peking Duk 21 Birthdays The Smith Street Band 22 Lemon To A Knife Fight The Wombats 23 Not Worth Hiding Alex The Astronaut 24 rockstar {Ft. 21 Savage} Post Malone 25 Weekends Amy Shark 26 Feel It Still Portugal. The Man 27 Be About You Winston Surfshirt 28 Mystik Tash Sultana 29 Mended Vera Blue 30 Low Blows Meg Mac 31 Lay Down Touch Sensitive 32 NUMB {Ft. GRAACE} Hayden James 33 Slow Mover Angie McMahon For more info, images and interviews contact: Gerry Bull, triple j Publicist 02 8333 1641 | [email protected] | triplej.net.au 34 DNA. Kendrick Lamar 35 Passionfruit Drake 36 I Haven't Been Taking Care Of Myself Alex Lahey 37 Slide {Ft. Frank Ocean/Migos} Calvin Harris 38 bellyache Billie Eilish 39 Got On My Skateboard Skegss 40 True Lovers Holy Holy 41 Blood {triple j Like A Version 2017} Gang Of Youths 42 Cola CamelPhat & Elderbrook 43 Murder To The Mind Tash Sultana 44 In Motion {Ft. -

China Regulatory and Market Access Pharmaceutical Report 2014
CHINA REGULATORY AND MARKET ACCESS PHARMACEUTICAL REPORT 2014 Pacific Bridge Medical 7315 Wisconsin Avenue, Suite 609E Bethesda, MD 20814 Tel: (301) 469-3400 Fax: (301) 469-3409 Email: [email protected] Copyright © 2014 Pacific Bridge Medical. All rights reserved. This content is protected by US and International copyright laws and may not be copied, reprinted, published, translated, resold, hosted, or otherwise distributed by any means without explicit permission. Disclaimer: the information contained in this report is the opinion of Pacific Bridge Medical, a subsidiary of Pacific Bridge, Inc. It is provided for general information purposes only, and does not constitute professional advice. We believe the contents to be true and accurate at the date of writing but can give no assurances or warranties regarding the accuracy, currency, or applicability of any of the contents in relation to specific situations and particular circumstances. CHINA REGULATORY AND MARKET ACCESS PHARMACEUTICAL REPORT (2013) TABLE OF CONTENTS I. China Pharmaceutical Industry Overview .......................................................5 A. Overview B. China Pharmaceutical Market Trends C. China’s Pharmaceutical Distribution System D. Brief Overview of China’s Pharmaceutical Regulations E. China Food and Drug Administration (CFDA) II. The China Healthcare System .........................................................................13 A. History of China’s Healthcare System B. Struggling Healthcare Services Sector C. 2009 Healthcare Reform D. Hospitals and Medical Resources 1. Hospitals in China 2. Current Problems in the Hospital Sector 3. Private Investment in the Hospital Sector 4. Hospital Reform E. Health Insurance in China III. Drug Registration Regulations ........................................................................21 A. Drug Registration Policy B. Classification of Drugs C. Drug Registration Applications D. Application Documents for New Drug Registration E.