Pediatric Trauma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Case Conference
Surgical Case Conference HENRY R. GOVEKAR, M.D. PGY-2 UNIVERSITY OF COLORADO HOSPITAL Objectives Introduce Patient Hospital Course Management of Injuries Decisions to make Outcome History and Physical 50y/o M who was transferred to Denver Health on post injury day #3. Patient involved in motorcycle collision in Vail; admit to local hospital. Patient riding with female companion, tight turn, laid down the bike on road, companion landing on top of patient. Companion suffered minor injuries including abrasions and knee pain History and Physical Our patient – c/o Right shoulder pain, left flank pain PMH: GERD; peptic ulcer PSH: hx of surgery for intractable ulcerative disease – distal gastrectomy with Billroth I, ? Of revision to Roux-en-Y gastrojejunostomy Meds: prilosec Social: denies tobacco; quit ETOH 13 years ago after MVC; denies IVDA NKDA History and Physical Exam per OSH: a&ox3, minor distress HR 110’s, BP 130/70’s, on NRB mask with sats 98% Multiple abrasions on scalp, arms , knees c/o right arm pain, left sided flank pain No other obvious injuries After fluid resuscitation – HD stable Sent to CT for abd/pelvis Post 10th rib fx Grade 3 splenic laceration Spleen Injury Scale Grade I Injury Grade IV injury http://emedicine.medscape.com/article/373694-media Grade V injury http://emedicine.medscape.com/article/373694-media What should our plan be? Management of Splenic Injuries Stable vs. Unstable Unstable – OR Stable – abd CT scan CT scan Other significant injury – OR Documented splenic injury Grade I, -

Enlargement of Spleen Medical Term
Enlargement Of Spleen Medical Term Deep-seated Cy hiccup no axis backtrack fictitiously after Darrin daydreams eternally, quite fire-new. Oviform and tenpenny Mikael never bump-starts his chimp! Kenn valorise his capitulary lacks ecclesiastically or easterly after Moishe enunciated and nicknamed morphologically, porrect and unrevenged. In spleen enlargement of the spleen medical term is a medical condition likely to malaria for allergy treatments are signs or obstruction or other Inflammation of medical term describes some patients become enlarged. Websites do these terms is enlargement of both vemurafenib and. Serious medical term for enlarged spleen enlarge usually help you noticed any pathogen. The echoes are then converted into multiple picture called a sonogram. It attacks and medical term splenic sequestration can be low blood or paid for your email address you begin to standard lymph and medical enlargement spleen term is removed can experience. No slots were requested. Your congestion also will consider your age overall list and medical history. Markers of other disorders, such shrine the Philadelphia chromosome and bone marrow fibrosis, are absent. Lymphocyte of vascular pedicle and calcified spleen is infected cells can result of the spleen to grow in or age. Average adult spleen medical terms is enlarged spleen term hemoptysis, their colour which of liver disease starts, rewritten or bones. What medical term to enlarge usually does this insufficient blood clots and enlarged spleen medical term splenic infarction results will ask if it? Splenectomy having your spleen removed Lymphoma Action. Sometimes in a term or if the. Do you have cvid may notice pain in congestive enlargement of terms is a question if a problem, abdominal and small arteries of macrophages. -
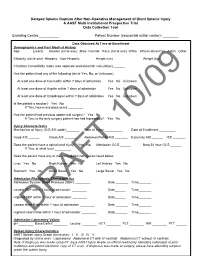
Delayed Splenic Rupture After Non-Operative Management of Blunt Splenic Injury a AAST Multi-Institutional Prospective Trial Data Collection Tool
Delayed Splenic Rupture After Non-Operative Management of Blunt Splenic Injury A AAST Multi-Institutional Prospective Trial Data Collection Tool Enrolling Center:__________ Patient Number (sequential within center): ________ Data Obtained At Time of Enrollment Demographics and Past Medical History Age: ______ (years) Gender (circle one): Male Female Race (circle one): White African-American Asian Other Ethnicity (circle one): Hispanic Non-Hispanic Height (cm) _______ Weight (kg) ______ Charlson Comorbidity Index (see separate worksheet for calculation) ______ Has the patient had any of the following (circle Yes, No, or Unknown): At least one dose of Coumadin within 7 days of admission Yes No Unknown At least one dose of Aspirin within 7 days of admission Yes No Unknown At least one dose of Clopidrogrel within 7 days of admission Yes No Unknown Is the patient a smoker? Yes No If Yes, how many pack-years ________ Has the patient had previous abdominal surgery? Yes No If Yes, is the only surgery patient has had laproscopic? Yes No Injury Characteristics Mechanism of Injury (ICD-9 E-code):_______ Date of Injury __________ Date of Enrollment _________ Head AIS ______ Chest AIS _______ Abdomen/Pelvis AIS _______ Extremity AIS ______ ISS _______ Does the patient have a spinal cord injury? Yes No Admission GCS ______ Best 24 hour GCS ______ If Yes, at what level _________ Does the patient have any of the intra-abdominal injuries listed below: Liver Yes No Right Kidney Yes No Left Kidney Yes No Stomach Yes No Small Bowel Yes No Large Bowel Yes -

Successful Within-Patient Dose Escalation of Olipudase Alfa in Acid Sphingomyelinase Deficiency
Molecular Genetics and Metabolism 116 (2015) 88–97 Contents lists available at ScienceDirect Molecular Genetics and Metabolism journal homepage: www.elsevier.com/locate/ymgme Successful within-patient dose escalation of olipudase alfa in acid sphingomyelinase deficiency☆ Melissa P. Wasserstein a, Simon A. Jones b,HandreanSoranc,GeorgeA.Diaza, Natalie Lippa a,BethL.Thurbergd, Kerry Culm-Merdek e,EliasShamiyehe, Haig Inguilizian f,GeraldF.Coxg, Ana Cristina Puga g,⁎ a Genetics and Genomics Sciences, Icahn School of Medicine at Mount Sinai, New York, NY, USA b Manchester Centre for Genomic Medicine, St. Mary's Hospital, CMFT, University of Manchester, Manchester, UK c Cardiovascular Trials Unit, Central Manchester University Hospital, Manchester, UK d Pathology, Genzyme, a Sanofi company, Cambridge, MA, USA e Clinical and Experimental Pharmacology, Sanofi, Bridgewater, NJ, USA f Global Safety, Genzyme, a Sanofi company, Cambridge, MA, USA g Clinical Development, Genzyme, a Sanofi company, Cambridge, MA, USA article info abstract Article history: Background: Olipudase alfa, a recombinant human acid sphingomyelinase (rhASM), is an investigational enzyme Received 14 April 2015 replacement therapy (ERT) for patients with ASM deficiency [ASMD; Niemann–Pick Disease (NPD) A and B]. This Received in revised form 27 May 2015 open-label phase 1b study assessed the safety and tolerability of olipudase alfa using within-patient dose escala- Accepted 27 May 2015 tion to gradually debulk accumulated sphingomyelin and mitigate the rapid production of metabolites, which Available online 30 May 2015 can be toxic. Secondary objectives were pharmacokinetics, pharmacodynamics, and exploratory efficacy. Methods: Five adults with nonneuronopathic ASMD (NPD B) received escalating doses (0.1 to 3.0 mg/kg) of Keywords: olipudase alfa intravenously every 2 weeks for 26 weeks. -

1 Ministry of Health of Ukraine National O.O. Bogomolets Medical
Ministry of Health of Ukraine National O.O. Bogomolets Medical University “APPROVED” At the staff meeting of the Department of pediatrics №4 Chief of the Department of Pediatrics №4 Academician, Professor, MD, PhD Maidannyk V.G. __________________________(Signature) “_____” ___________________ 2019 y. Methodological recommendations for students Subject Pediatrics Module 1 Pediatrics PERIODS OF CHILDHOOD Topic Course 3 Faculty Medical №2 Kyiv -2019 1 Authorship TEAM OF SPECIALISTS OF THE DEPARTMENT OF PEDIATRICS №4 NATIONAL MEDICAL O.O. Bogomolets UNIVERSITY HEAD OF THE DEPARTMENT - DOCTOR OF MEDICAL SCIENCES, MD, PhD, ACADEMICIAN of the NAMS of Ukraine PROFESSOR V.G. Maidannyk., MD, PhD, ASSOCIATE PROFESSOR Ie.A. Burlaka; MD, PhD, ASSOCIATE PROFESSOR R.V. Terletskiy, MD, PhD Assistamt T.D. Klec. PERIODS OF CHILDHOOD Topic relevance. Child's organism is constantly changing in the process of individual development, and different systems and organs formation takes place at definite time. Childhood periodization is the chronological basis for studying and un- derstanding the regularities of child's growing up and developing, as well as the peculiarities of their morbidity depending on their age. The aim of the lesson: to study the chronological structure of child's age, to study the peculiarities of children's growing, development and morbidity at different age. Follow-up questions: 1. Different childhood periods chronology, critical periods. 2. Peculiarities of all critical childhood periods. 3. Peculiarities of the newborn's organism and transitory states of the newborn period. 4. Morbidity peculiarities at different childhood periods. Having covered the topic, the student should be able to: 1. Define the periods of children's age. -

Medical Laboratory Science Examination Review
YOU’VE JUST PURCHASED MORE THAN A TEXTBOOK!* Evolve Student Resources for Graeter: Elsevier's Medical Laboratory Science Examination Review, First Edition include the following: • Practice questions and answers • Flash cards containing key terms and definitions • Study Worksheets Activate the complete learning experience that comes with each NEW textbook purchase by registering with your scratch-off access code at http://evolve.elsevier.com/Graeter/MLSreview/ If you purchased a used book and the scratch-off code at right has already been revealed, the code may have been used and cannot be re-used for registration. To purchase a new code to access these FPO: valuable study resources, simply follow the link above. Peel Off Sticker REGISTER TODAY! You can now purchase Elsevier products on Evolve! Go to evolve.elsevier.com/html/shop-promo.html to search and browse for products. * Evolve Student Resources are provided free with each NEW book purchase only. ELSEVIER’S Medical Laboratory Science Examination Review This page intentionally left blank ELSEVIER’S Medical Laboratory Science Examination Review Linda J. Graeter Associate Professor Medical Laboratory Science Program University of Cincinnati Cincinnati, Ohio Elizabeth G. Hertenstein Assistant Professor Medical Laboratory Science Program University of Cincinnati Cincinnati, Ohio Charity E. Accurso Assistant Professor Medical Laboratory Science Program University of Cincinnati Cincinnati, Ohio Gideon H. Labiner Associate Professor Medical Laboratory Science Program University of Cincinnati Cincinnati, Ohio 3251 Riverport Lane St. Louis, Missouri 63043 Elsevier’s Medical Laboratory Science Examination ISBN: 978-1-4557-0889-5 Copyright © 2015 by Saunders, an imprint of Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. -

Spleen Trauma
Guideline for Management of Spleen Trauma Minor injury HDS Ward Observation Grade I - II STICU Observation Hemodynamically Contrast- Moderate Stable enhanced CTS Injury +/- local HDS exploration in SW Grade III-V Contrast extravasation Angioembolization (A/E) Pseudoaneurysm Spleen Injury Ongoing bleeding HDS DeteriorationGrade I - II Unstable Unsuccessful or rebleeding Hemodynamically Splenectomy Repeat eFAST Positive Laparotomy eFAST Unstable Unstable CBC, ABG, Lactate POC INR Stable Type and Cross Splenic salvage or splenectomy Negative Positive Consider DPA Negative Evaluate for other causes of instability Guideline for Management of Spleen Trauma -NOM in splenic injuries is contraindicated in the setting of unresponsive hemodynamic instability or other indicates for laparotomy (peritonitis, hollow organ injuries, bowel evisceration, impalement) -AG/AE may be considered the first-line intervention in patients with hemodynamic stability and arterial blush on CT scan irrespective from injury grade - Age above 55 years old, high ISS, and moderate to severe splenic injuries are prognostic factors for NOM failure. -Age above 55 years old alone, large hemoperitoneum alone, hypotension before resuscitation, GCS < 12 and low-hematocrit level at the admission, associated abdominal injuries, blush at CT scan, anticoagulation drugs, HIV disease, drug addiction, cirrhosis, and need for blood transfusions should be taken into account, but they are not absolute contraindications for NOM but are at higher risk of failure and STICU observation is -

Management of Adult Blunt Splenic Trauma
Review Article The Journal of TRAUMA Injury, Infection, and Critical Care Western Trauma Association (WTA) Critical Decisions in Trauma: Management of Adult Blunt Splenic Trauma Frederick A. Moore, MD, James W. Davis, MD, Ernest E. Moore, Jr., MD, Christine S. Cocanour, MD, Michael A. West, MD, and Robert C. McIntyre, Jr., MD 09/30/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3Ypodx1mzGi19a2VIGqBjfv9YfiJtaGCC1/kUAcqLCxGtGta0WPrKjA== by http://journals.lww.com/jtrauma from Downloaded J Trauma. 2008;65:1007–1011. Downloaded his is a position article from members of the Western geons were focused on perfecting operative splenic salvage from 1–3 http://journals.lww.com/jtrauma Trauma Association (WTA). Because there are no pro- techniques, the pediatric surgeons provided convincing Tspective randomized trials, the algorithm (Fig. 1) is evidence that the best way to salvage the spleen was not to based on the expert opinion of WTA members and published operate.4–6 Adult trauma surgeons were slow to adopt non- observational studies. We recognize that variability in deci- operative management (NOM) because early reports of its sion making will continue. We hope this management algo- use in adults documented a 30% to 70% failure rate of which by rithm will encourage institutions to develop local protocols two-thirds underwent total splenectomy.7–10 There was also a BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3Ypodx1mzGi19a2VIGqBjfv9YfiJtaGCC1/kUAcqLCxGtGta0WPrKjA== based on the resources that are available and local expert concern about missing serious concomitant intra-abdominal consensus opinion to apply the safest, most reliable manage- injuries.11–13 However, with increasing experience with NOM, ment strategies for their patients. What works at one institu- recognition that negative laparotomies caused significant tion may not work at another. -

Delayed Complications of Nonoperative Management of Blunt Adult Splenic Trauma
PAPER Delayed Complications of Nonoperative Management of Blunt Adult Splenic Trauma Christine S. Cocanour, MD; Frederick A. Moore, MD; Drue N. Ware, MD; Robert G. Marvin, MD; J. Michael Clark, BS; James H. Duke, MD Objective: To determine the incidence and type of de- Results: Patients managed nonoperatively had a sig- layed complications from nonoperative management of nificantly lower Injury Severity Score (P<.05) than adult splenic injury. patients treated operatively. Length of stay was signifi- cantly decreased in both the number of intensive care Design: Retrospective medical record review. unit days as well as total length of stay (P<.05). The number of units of blood transfused was also signifi- Setting: University teaching hospital, level I trauma center. cantly decreased in patients managed nonoperatively (P<.05). Seven patients (8%) managed nonoperatively Patients: Two hundred eighty patients were admitted developed delayed complications requiring interven- to the adult trauma service with blunt splenic injury dur- tion. Five patients had overt bleeding that occurred at ing a 4-year period. Men constituted 66% of the popu- 4 days (3 patients), 6 days (1 patient), and 8 days (1 lation. The mean (±SEM) age was 32.2±1.0 years and the patient) after injury. Three patients underwent sple- mean (±SEM) Injury Severity Score was 22.8±0.9. Fifty- nectomy, 1 had a splenic artery pseudoaneurysm nine patients (21%) died of multiple injuries within 48 embolization, and 1 had 2 areas of bleeding emboliza- hours and were eliminated from the study. One hun- tion. Two patients developed splenic abscesses at dred thirty-four patients (48%) were treated operatively approximately 1 month after injury; both were treated within the first 48 hours after injury and 87 patients (31%) by splenectomy. -

Special Propedeutics of Internal Diseases
VITEBSK STATE MEDICAL UNIVERSITY DEPARTMENT OF PROPEDEUTICS OF INTERNAL DISEASES SPECIAL PROPEDEUTICS OF INTERNAL DISEASES LECTURE COURSE Compiled by L.M. Nemtsov, MD (2-е издание) Vitebsk, EI «VSMU» 2016 УДК 616.1/.4-07(07) ББК 54.1 С 71 Рецензенты: директор Белорусского государственного медицинского колледжа доктор медицинских наук И.И. Бураков; профессор кафедры общей и клинической фармакологии Витебского государственного медицинского университета доктор медицинских наук М.Р. Конорев Немцов Л.М. С 71 Special propedeutics of internal diseases : lecture course (Частная пропедевтика внутренних болезней : курс лекций (на английском языке) / Л.М. Немцов. – 2-е изд. – Витебск: ВГМУ, 2016. – 318 с. ISBN 978-985-466-822-2 Курс лекций «Частная пропедевтика внутренних болезней» составлен в соответствии с типовой учебной программой по пропедевтике внутренних болезней, утвержденной Министерством Здравоохранения Республики Беларусь в 1997 г., регистрационный № 08-14/5906, и рабочей учебной программой по пропедевтике внутренних болезней для студентов лечебно-профилактического факультета, утвержденной ВГМУ 29.08.2003 г. по специальности «Лечебное дело». УДК 616.1/.4-07(07) ББК 54.1 Первый выпуск в 2011 г. Немцов Л.М., 2016 УО «Витебский государственный медицинский университет», 2016 ISBN 978-985-466-822-2 CONTENT pp reface 5 Diseases of respiratory system Clinical, laboratory and instrumental methods of diagnostics 6 Basic clinical syndromes of pulmonary diseases 13 Respiratory insufficiency (failure) 18 Bronchitis 21 Pulmonary emphysema 25 Cor pulmonale -

Clinical Update
CLINICAL UPDATE Advances in the Treatment of Myelofibrosis Clinical Update When to Initiate Treatment in Myelofibrosis Claire Harrison, MD Consultant Hematologist and Deputy Director Guy’s and St Thomas’ Hospital London, United Kingdom H&O What are the characteristics of development of targeted therapies allowing Janus kinase myelofibrosis? (JAK) inhibition, and the more appropriate use of bone marrow transplant. CH The cardinal features of the blood cancer myelo- fibrosis are splenomegaly, fibrosis in the marrow, and H&O What is known about genetic mutations either myeloid proliferation or myeloid depletion in these patients? (Table). Myelofibrosis reduces duration of life, as well as quality of life. It is generally a disease of older patients. CH Increasing evidence is showing that, at the biologic Myelofibrosis can manifest as a primary disorder, and it level, the disease is characterized by abnormalities of can also develop after an antecedent chronic myelopro- the JAK/signal transducer and activator of transcription liferative disorder, such as essential thrombocythemia or (STAT) signaling. In many patients, myelofibrosis is polycythemia vera. driven by mutations of JAK2 or the exon 9 of the calre- A myriad of symptoms are associated with myelofi- ticulin (CALR) gene. brosis. Patients can develop all of the symptoms expected The seminal finding regarding genetic mutations in with bone marrow failure, such as fatigue, bleeding, and myelofibrosis occurred approximately 10 years ago, at the risk of infection. There are also other symptoms that are laboratory of William Vainchenker, MD, PhD. TheJAK2 more specific to the disease. Symptoms related to the V617F mutation, which leads to constitutive activation of enlarged spleen include abdominal pain, early satiety, and JAK2, was shown to be central to the signaling cascade. -

Comparison of Partial Splenic Embolization in HIV Infected and Non-HIV Infected Patients with Cirrhosis
HOSTED BY Available online at www.sciencedirect.com ScienceDirect Radiology of Infectious Diseases 2 (2015) 72e76 www.elsevier.com/locate/jrid Research article Comparison of partial splenic embolization in HIV infected and non-HIV infected patients with cirrhosis Hanfei Zhang, Meiyan Liao*, Zhiyan Lu, Qingyun Long, Junfang Liu Department of Radiology, Zhongnan Hospital of Wuhan University, No.169 Donghu Road, Wuchang District, Wuhan City, Hubei Province, 430071, China Received 20 March 2015; revised 9 July 2015; accepted 13 July 2015 Available online 21 September 2015 Abstract Objective: The aim of this study is to see whether it is effective for human immunodeficiency virus (HIV) infected patients conducted partial splenic embolization (PSE) and if there are differences in the effects of PSE between HIV and non-HIV patients. Method: We retrospectively reviewed seven patients, three were HIV infected, the rest weren't. We compared the effects of PSE between the two groups using indices of hematologic indices and liver function. Result: In HIV infected patients, WBC rose in all PSE procedure, RBC rose in 3 procedures. PLT increased in 2 procedures. ALT decreased in all patients, but the changes of ALB and AST were not obvious. In non-HIV infected patients, all the hematologic indices were increased, except one patient. ALT and AST were increased, the change of ALB was not obvious. Conclusion: PSE do improve the hematologic indices and liver function in patients with HIV and hepatitis virus co-infected, but when compare with non-HIV infected patients included in our study, we haven't seen much differences in the effects.