A Novel Mutation (P.Met1?) of a Cuban Patient in the NAGLU Gene
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epidemiology of Mucopolysaccharidoses Update
diagnostics Review Epidemiology of Mucopolysaccharidoses Update Betul Celik 1,2 , Saori C. Tomatsu 2 , Shunji Tomatsu 1 and Shaukat A. Khan 1,* 1 Nemours/Alfred I. duPont Hospital for Children, Wilmington, DE 19803, USA; [email protected] (B.C.); [email protected] (S.T.) 2 Department of Biological Sciences, University of Delaware, Newark, DE 19716, USA; [email protected] * Correspondence: [email protected]; Tel.: +302-298-7335; Fax: +302-651-6888 Abstract: Mucopolysaccharidoses (MPS) are a group of lysosomal storage disorders caused by a lysosomal enzyme deficiency or malfunction, which leads to the accumulation of glycosaminoglycans in tissues and organs. If not treated at an early stage, patients have various health problems, affecting their quality of life and life-span. Two therapeutic options for MPS are widely used in practice: enzyme replacement therapy and hematopoietic stem cell transplantation. However, early diagnosis of MPS is crucial, as treatment may be too late to reverse or ameliorate the disease progress. It has been noted that the prevalence of MPS and each subtype varies based on geographic regions and/or ethnic background. Each type of MPS is caused by a wide range of the mutational spectrum, mainly missense mutations. Some mutations were derived from the common founder effect. In the previous study, Khan et al. 2018 have reported the epidemiology of MPS from 22 countries and 16 regions. In this study, we aimed to update the prevalence of MPS across the world. We have collected and investigated 189 publications related to the prevalence of MPS via PubMed as of December 2020. In total, data from 33 countries and 23 regions were compiled and analyzed. -

Pathophysiology of Mucopolysaccharidosis
Pathophysiology of Mucopolysaccharidosis Dr. Christina Lampe, MD The Center for Rare Diseases, Clinics for Pediatric and Adolescent Medicine Helios Dr. Horst Schmidt Kliniken, Wiesbaden, Germany Inborn Errors of Metabolism today - more than 500 diseases (~10 % of the known genetic diseases) 5000 genetic diseases - all areas of metabolism involved - vast majority are recessive conditions 500 metabolic disorders - individually rare or very rare - overall frequency around 1:800 50 LSD (similar to Down syndrome) LSDs: 1: 5.000 live births MPS: 1: 25.000 live births 7 MPS understanding of pathophysiology and early diagnosis leading to successful therapy for several conditions The Lysosomal Diseases (LSD) TAY SACHS DIS. 4% WOLMAN DIS. ASPARTYLGLUCOSAMINURIA SIALIC ACID DIS. SIALIDOSIS CYSTINOSIS 4% SANDHOFF DIS. 2% FABRY DIS. 7% POMPE 5% NIEMANN PICK C 4% GAUCHER DIS. 14% Mucopolysaccharidosis NIEMANN PICK A-B 3% MULTIPLE SULPH. DEF. Mucolipidosis MUCOLIPIDOSIS I-II 2% Sphingolipidosis MPSVII Oligosaccharidosis GM1 GANGLIOSIDOSIS 2% MPSVI Neuronale Ceroid Lipofuszinois KRABBE DIS. 5% MPSIVA others MPSIII D A-MANNOSIDOSIS MPSIII C MPSIIIB METACHROMATIC LEUKOD. 8% MPS 34% MPSIIIA MPSI MPSII Initial Description of MPS Charles Hunter, 1917: “A Rare Disease in Two Brothers” brothers: 10 and 8 years hearing loss dwarfism macrocephaly cardiomegaly umbilical hernia joint contractures skeletal dysplasia death at the age of 11 and 16 years Description of the MPS Types... M. Hunter - MPS II (1917) M. Hurler - MPS I (1919) M. Morquio - MPS IV (1929) M. Sanfilippo - MPS III (1963) M. Maroteaux-Lamy - MPS IV (1963) M. Sly - MPS VII (1969) M. Scheie - MPS I (MPS V) (1968) M. Natowicz - MPS IX (1996) The Lysosome Lysosomes are.. -

Mucopolysaccharidosis Type II: One Hundred Years of Research, Diagnosis, and Treatment
International Journal of Molecular Sciences Review Mucopolysaccharidosis Type II: One Hundred Years of Research, Diagnosis, and Treatment Francesca D’Avanzo 1,2 , Laura Rigon 2,3 , Alessandra Zanetti 1,2 and Rosella Tomanin 1,2,* 1 Laboratory of Diagnosis and Therapy of Lysosomal Disorders, Department of Women’s and Children ‘s Health, University of Padova, Via Giustiniani 3, 35128 Padova, Italy; [email protected] (F.D.); [email protected] (A.Z.) 2 Fondazione Istituto di Ricerca Pediatrica “Città della Speranza”, Corso Stati Uniti 4, 35127 Padova, Italy; [email protected] 3 Molecular Developmental Biology, Life & Medical Science Institute (LIMES), University of Bonn, 53115 Bonn, Germany * Correspondence: [email protected] Received: 17 January 2020; Accepted: 11 February 2020; Published: 13 February 2020 Abstract: Mucopolysaccharidosis type II (MPS II, Hunter syndrome) was first described by Dr. Charles Hunter in 1917. Since then, about one hundred years have passed and Hunter syndrome, although at first neglected for a few decades and afterwards mistaken for a long time for the similar disorder Hurler syndrome, has been clearly distinguished as a specific disease since 1978, when the distinct genetic causes of the two disorders were finally identified. MPS II is a rare genetic disorder, recently described as presenting an incidence rate ranging from 0.38 to 1.09 per 100,000 live male births, and it is the only X-linked-inherited mucopolysaccharidosis. The complex disease is due to a deficit of the lysosomal hydrolase iduronate 2-sulphatase, which is a crucial enzyme in the stepwise degradation of heparan and dermatan sulphate. -

Tepzz¥5Z5 8 a T
(19) TZZ¥Z___T (11) EP 3 505 181 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 03.07.2019 Bulletin 2019/27 A61K 38/46 (2006.01) C12N 9/16 (2006.01) (21) Application number: 18248241.4 (22) Date of filing: 28.12.2018 (84) Designated Contracting States: (72) Inventors: AL AT BE BG CH CY CZ DE DK EE ES FI FR GB • DICKSON, Patricia GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO Torrance, CA California 90502 (US) PL PT RO RS SE SI SK SM TR • CHOU, Tsui-Fen Designated Extension States: Torrance, CA California 90502 (US) BA ME • EKINS, Sean Designated Validation States: Brooklyn, NY New York 11215 (US) KH MA MD TN • KAN, Shih-Hsin Torrance, CA California 90502 (US) (30) Priority: 28.12.2017 US 201762611472 P • LE, Steven 05.04.2018 US 201815946505 Torrance, CA California 90502 (US) • MOEN, Derek R. (71) Applicants: Torrance, CA California 90502 (US) • Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center (74) Representative: J A Kemp Torrance, CA 90502 (US) 14 South Square • Phoenix Nest Inc. Gray’s Inn Brooklyn NY 11215 (US) London WC1R 5JJ (GB) (54) PREPARATION OF ENZYME REPLACEMENT THERAPY FOR MUCOPOLYSACCHARIDOSIS IIID (57) The present disclosure relates to compositions for use in a method of treating Sanfilippo syndrome (also known as Sanfilippo disease type D, Sanfilippo D, mu- copolysaccharidosis type IIID, MPS IIID). The method can entail injecting to the spinal fluid of a MPS IIID patient an effective amount of a composition comprising a re- combinant human acetylglucosamine-6-sulfatase (GNS) protein comprising the amino acid sequence of SEQ ID NO: 1 or an amino acid sequence having at least 90% sequence identity to SEQ ID NO: 1 and having the en- zymatic activity of the human GNS protein. -
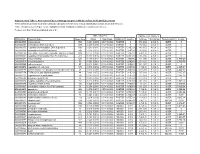
Association of Gene Ontology Categories with Decay Rate for Hepg2 Experiments These Tables Show Details for All Gene Ontology Categories
Supplementary Table 1: Association of Gene Ontology Categories with Decay Rate for HepG2 Experiments These tables show details for all Gene Ontology categories. Inferences for manual classification scheme shown at the bottom. Those categories used in Figure 1A are highlighted in bold. Standard Deviations are shown in parentheses. P-values less than 1E-20 are indicated with a "0". Rate r (hour^-1) Half-life < 2hr. Decay % GO Number Category Name Probe Sets Group Non-Group Distribution p-value In-Group Non-Group Representation p-value GO:0006350 transcription 1523 0.221 (0.009) 0.127 (0.002) FASTER 0 13.1 (0.4) 4.5 (0.1) OVER 0 GO:0006351 transcription, DNA-dependent 1498 0.220 (0.009) 0.127 (0.002) FASTER 0 13.0 (0.4) 4.5 (0.1) OVER 0 GO:0006355 regulation of transcription, DNA-dependent 1163 0.230 (0.011) 0.128 (0.002) FASTER 5.00E-21 14.2 (0.5) 4.6 (0.1) OVER 0 GO:0006366 transcription from Pol II promoter 845 0.225 (0.012) 0.130 (0.002) FASTER 1.88E-14 13.0 (0.5) 4.8 (0.1) OVER 0 GO:0006139 nucleobase, nucleoside, nucleotide and nucleic acid metabolism3004 0.173 (0.006) 0.127 (0.002) FASTER 1.28E-12 8.4 (0.2) 4.5 (0.1) OVER 0 GO:0006357 regulation of transcription from Pol II promoter 487 0.231 (0.016) 0.132 (0.002) FASTER 6.05E-10 13.5 (0.6) 4.9 (0.1) OVER 0 GO:0008283 cell proliferation 625 0.189 (0.014) 0.132 (0.002) FASTER 1.95E-05 10.1 (0.6) 5.0 (0.1) OVER 1.50E-20 GO:0006513 monoubiquitination 36 0.305 (0.049) 0.134 (0.002) FASTER 2.69E-04 25.4 (4.4) 5.1 (0.1) OVER 2.04E-06 GO:0007050 cell cycle arrest 57 0.311 (0.054) 0.133 (0.002) -

Bioinformatics Classification of Mutations in Patients with Mucopolysaccharidosis IIIA
Metabolic Brain Disease (2019) 34:1577–1594 https://doi.org/10.1007/s11011-019-00465-6 ORIGINAL ARTICLE Bioinformatics classification of mutations in patients with Mucopolysaccharidosis IIIA Himani Tanwar1 & D. Thirumal Kumar1 & C. George Priya Doss1 & Hatem Zayed2 Received: 30 April 2019 /Accepted: 8 July 2019 /Published online: 5 August 2019 # The Author(s) 2019 Abstract Mucopolysaccharidosis (MPS) IIIA, also known as Sanfilippo syndrome type A, is a severe, progressive disease that affects the central nervous system (CNS). MPS IIIA is inherited in an autosomal recessive manner and is caused by a deficiency in the lysosomal enzyme sulfamidase, which is required for the degradation of heparan sulfate. The sulfamidase is produced by the N- sulphoglucosamine sulphohydrolase (SGSH) gene. In MPS IIIA patients, the excess of lysosomal storage of heparan sulfate often leads to mental retardation, hyperactive behavior, and connective tissue impairments, which occur due to various known missense mutations in the SGSH, leading to protein dysfunction. In this study, we focused on three mutations (R74C, S66W, and R245H) based on in silico pathogenic, conservation, and stability prediction tool studies. The three mutations were further subjected to molecular dynamic simulation (MDS) analysis using GROMACS simulation software to observe the structural changes they induced, and all the mutants exhibited maximum deviation patterns compared with the native protein. Conformational changes were observed in the mutants based on various geometrical parameters, such as conformational stability, fluctuation, and compactness, followed by hydrogen bonding, physicochemical properties, principal component analysis (PCA), and salt bridge analyses, which further validated the underlying cause of the protein instability. Additionally, secondary structure and surrounding amino acid analyses further confirmed the above results indicating the loss of protein function in the mutants compared with the native protein. -

Assessment of Predicted Enzymatic Activity of Alpha-N- Acetylglucosaminidase (NAGLU) Variants of Unknown Significance for CAGI 2016
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Hum Mutat Manuscript Author . Author manuscript; Manuscript Author available in PMC 2020 April 14. Published in final edited form as: Hum Mutat. 2019 September ; 40(9): 1519–1529. doi:10.1002/humu.23875. Assessment of predicted enzymatic activity of alpha-N- acetylglucosaminidase (NAGLU) variants of unknown significance for CAGI 2016 Wyatt T. Clark1, Laura Kasak2,3, Constantina Bakolitsa2, Zhiqiang Hu2, Gaia Andreoletti2,*, Giulia Babbi4, Yana Bromberg5, Rita Casadio4, Roland Dunbrack6, Lukas Folkman7, Colby T. Ford8, David Jones9, Panagiotis Katsonis10,*, Kunal Kundu11, Olivier Lichtarge12, Pier Luigi Martelli4, Sean D. Mooney13,*, Conor Nodzak8, Lipika R. Pal11, Predrag Radivojac14,*, Castrense Savojardo4, Xinghua Shi8, Yaoqi Zhou15, Aneeta Uppal8, Qifang Xu6, Yizhou Yin11,*, Vikas Pejaver16, Meng Wang17, Liping Wei17, John Moult11, G. Karen Yu1, Steven E. Brenner2, Jonathan H. LeBowitz1 1BioMarin Pharmaceutical, San Rafael, California, USA 2Department of Plant and Microbial Biology, University of California, Berkeley, CA, USA 3Institute of Biomedicine and Translational Medicine, University of Tartu, Tartu, Estonia 4Biocomputing Group, Department of Pharmacy and Biotechnology, University of Bologna, Bologna, Italy 5Department of Biochemistry and Microbiology, Rutgers University, New Brunswick, NJ, USA 6Fox Chase Cancer Center, Philadelphia, PA, USA 7School of Information and Communication Technology, Griffith University, Southport, Australia 8Department of -

Sanfilippo Disease Type D: Deficiency of N-Acetylglucosamine-6- Sulfate Sulfatase Required for Heparan Sulfate Degradation
Proc. Nat!. Acad. Sci. USA Vol. 77, No. 11, pp. 6822-6826, November 1980 Medical Sciences Sanfilippo disease type D: Deficiency of N-acetylglucosamine-6- sulfate sulfatase required for heparan sulfate degradation (mucopolysaccharidosis/keratan sulfate/lysosomes) HANS KRESSE, EDUARD PASCHKE, KURT VON FIGURA, WALTER GILBERG, AND WALBURGA FUCHS Institute of Physiological Chemistry, Waldeyerstrasse 15, D-4400 Mfinster, Federal Republic of Germany Communicated by Elizabeth F. Neufeld, July 10, 1980 ABSTRACT Skin fibroblasts from two patients who had lippo syndromes and excreted excessive amounts of heparan symptoms of the Sanfilippo syndrome (mucopolysaccharidosis sulfate and keratan sulfate in the urine. His fibroblasts were III) accumulated excessive amounts of hean sulfate and were unable to desulfate N-acetylglucosamine-6-sulfate and the unable to release sulfate from N-acety lucosamine)--sulfate linkages in heparan sulfate-derived oligosaccharides. Keratan corresponding sugar alcohol (17, 18). It was therefore suggested sulfate-derived oligosaccharides bearing the same residue at that N-acetylglucosamine-6-sulfate sulfatase is involved in the the nonreducing end and p-nitrophenyl6sulfo-2-acetamido- catabolism of both types of macromolecules. 2-deoxy-D-ucopyranoside were degraded normally. Kinetic In this paper, we describe a new disease, tentatively desig- differences between the sulfatase activities of normal fibro- nated Sanfilippo disease type D, that is characterized by the blasts were found. These observations suggest that N-acetyl- excessive excretion glucosamine4-6sulfate sulfatase activities degrading heparan clinical features of the Sanfilippo syndrome, sulfate and keratan sulfate, respectively, can be distinguished. of heparan sulfate, and the inability to release inorganic sulfate It is the activity directed toward heparan sulfate that is deficient from N-acetylglucosamine-6-sulfate residues of heparan sul- in these patients; we propose that this deficiency causes Sanfi- fate-derived oligosaccharides. -

Journal of Inborn Errors of Metabolism & Screening
Original Article Journal of Inborn Errors Determination of Reference Values for of Metabolism & Screening 2021, Volume 9: e20200023 Alpha-N-Acetylglucosaminidase Activities DOI: https://doi.org/10.1590/2326–4594– JIEMS–2020–0023 in Patients with Sanfilippo Type B Disease and Control Population in Colombia Johana Ramírez Borda1 and Alfredo Uribe-Ardila1 Abstract Sanfilippo B is a lysosomal disorder characterized by the pathological accumulation of heparan sulfate. It is caused by mutations in the NAGLU gene that codes for the alpha-N-acetylglucosaminidase enzyme. The objective of this study was to determine the reference values and frequency of Sanfilippo B in Colombia through an enzyme analysis of leukocytes extracts. We aim to inform the community and the health system so that they can work in a preventive way, providing an early diagnosis of patients and thus providing an appropriate management of the symptoms. We carried out an endpoint assay that indirectly quantifies NAGLU activity through the cleavage of 4-methylumbelliferone from the 4-methylumbelliferyl-2-acetamido-2-deoxy-α-D-glucopyranoside substrate. The activity of 463 healthy volunteers (Range: 0.6 - 4 nmol/mg/h , Median: 1.69 +/- 0.73 ) as well as 462 patients referred for clinical suspicion, was calculated. From the last group, 7 cases turned out to be positive (Range: 0 - 0.24 nmol/mg/h , Median: 0.13 +/- 0.09 ). The cut-off point according to ROC analysis between affected patients and controls was 0.42 nmol/mg/h. To our knowledge, this study is the first in Colombia where an estimated frequency of Sanfilippo type B is calculated by providing enzyme activity ranges and a cut-off point. -

Prediction of the Effect of Naturally Occurring Missense Mutations On
bioRxiv preprint doi: https://doi.org/10.1101/598870; this version posted April 5, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. PREDICTION OF THE EFFECT OF NATURALLY OCCURRING MISSENSE MUTATIONS ON CELLULAR N-Acetyl-Glucosaminidase ENZYMATIC ACTIVITY Colby T. Ford∗ Conor M. Nodzak Department of Bioinformatics and Genomics Department of Bioinformatics and Genomics The University of North Carolina at Charlotte The University of North Carolina at Charlotte Charlotte, NC 28223 Charlotte, NC 28223 Aneeta Uppal Xinghua Shi Department of Bioinformatics and Genomics Department of Bioinformatics and Genomics The University of North Carolina at Charlotte The University of North Carolina at Charlotte Charlotte, NC 28223 Charlotte, NC 28223 April 4, 2019 ABSTRACT In 2015, the Critical Assessment of Genome Interpretation (CAGI) proposed a challenge to devise a computational method for predicting the phenotypic consequences of genetic variants of a lysosomal hydrolase enzyme known as α-N-acetylglucosaminidase (NAGLU). In 2014, the Human Gene Mutation Database released that 153 NAGLU mutations associated with MPS IIIB and 90 of them are missense mutations. The ExAC dataset catalogued 189 missense mutations NAGLU based on exome sequence data from about 60,000 individual and 24 of them are known to be disease associated. Biotechnology company, BioMarin, has quantified the relative functionality of NAGLU for the remaining subset of 165 missense mutations. For this particular challenge, we examined the subset missense mutations within the ExAC dataset and predicted the probability of a given mutation being deleterious and relating this measure to the capacity of enzymatic activity. -

Anesthetic Considerations and Clinical Manifestations 243
MUCOPOLYSACCHARIDOSES: ANESTHETIC CONSIDERATIONS AND CLINICAL MANIFESTATIONS 243 MUCOPOLYSACCHARIDOSES: ANESTHETIC CONSIDERATIONS AND CLINICAL MANIFESTATIONS * ** *** JERMALE A. SAM , AMIR R. BALUCH , RASHID S. NIAZ , *** **** LINDSEY LONADIER AND ALAN D. KAYE Abstract Mucopolysaccharidosis (MPS) is a group of genetic disorders that presents challenges during anesthetic care and in particular difficulty with airway management. Patients should be managed by experienced anesthesiologists at centers that are familiar with these types of conditions. Rarely encountered disease states have been identified as important topics in the continuing education of clinical anesthesiologists. This review will define MPS, describe the pathophysiology of MPS, describe how patients with this rare lysosomal storage disorders have dysfunction of tissues, cite the incidence of MPS, list the clinical manifestations and specific problems associated with the administration of anesthesia to patients with MPS, present treatment options for patients with MPS, define appropriate preoperative evaluation and perioperative management of these patients, including, to anticipate potential postoperative airway problems. Introduction Mucopolysaccharidoses (MPS) are a group of rare genetic lysosomal storage disorders characterized by the deficiency in or complete lack of necessary lysosomal enzymes required for the stepwise breakdown of glycosaminoglycans (GAGs, also known as mucopolysaccharidoses)1-5. Consequently, fragments of GAGs accumulate intracellularly in the lysosome resulting in cellular enlargement causing disruption/dysfunction of structure and function of tissues. This process leads to numerous clinical abnormalities. Incidence of all types of MPS is reported to be between 1in 10,000 to 1 in 30,000 live births and are transmitted autosomal recessive except for MPS II which is X-linked1,4,5. Pathophysiology Glycosaminoglycans are long-chain complex carbohydrates consisting of repeating sulfated acidic and amino sugar disaccharide units. -

Matching Whole Genomes to Rare Genetic Disorders: Identification of Potential
bioRxiv preprint doi: https://doi.org/10.1101/707687; this version posted July 18, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Matching whole genomes to rare genetic disorders: Identification of potential causative variants using phenotype-weighted knowledge in the CAGI SickKids5 clinical genomes challenge Lipika R. Pal 1*, Kunal Kundu 1, 2, Yizhou Yin 1, John Moult 1, 3* 1 Institute for Bioscience and Biotechnology Research, University of Maryland, 9600 Gudelsky Drive, Rockville, MD 20850, USA. 2 Computational Biology, Bioinformatics and Genomics, Biological Sciences Graduate Program, University of Maryland, College Park, MD 20742, USA. 3 Department of Cell Biology and Molecular Genetics, University of Maryland, College Park, MD 20742, USA. *Corresponding authors: [email protected] Phone: (240) 314-6146 [email protected] Phone: (240) 314-6241 FAX: (240) 314-6255 Funding Information: This work was partially supported by NIH R01GM120364 and R01GM104436 to JM. The CAGI experiment coordination is supported by NIH U41 HG007346 and the CAGI conference by NIH R13 HG006650. bioRxiv preprint doi: https://doi.org/10.1101/707687; this version posted July 18, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Keywords: Whole-genome sequencing data, Human Phenotype Ontology (HPO), Eye disorder, Connective-tissue disorder, Neurological diseases, Diagnostic variants, CAGI5.