Safety and Feasibility of Antiretroviral Preexposure Prophylaxis For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Fluoxymesterone-Dea Schedule Iii Androfluorene
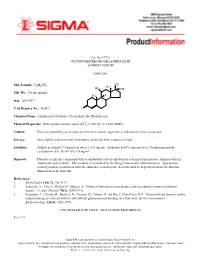
Cat. No. F7751 FLUOXYMESTERONE--DEA SCHEDULE III ANDROFLUORENE Androgen. OH Mol. Formula: C20H29FO3 HO H3C CH3 Mol. Wt.: 336.45 (anhyd.) F H3C m.p.: 288-290°C CAS Registry No.: 76-43-7 O Chemical Name: 4-Androsten-9a-fluoro-17a-methyl-11b,17b-diol-3-one 22 Physical Properties: White photosensitive solid. [a] D = +102.34° (c = 0.47, EtOH). Caution: Due care should be exercised to prevent skin contact, ingestion or inhalation of this compound. Storage: Store tightly sealed at room temperature, protected from exposure to light. Solubility: Soluble in ethanol (7.3 mg/ml) or water (< 0.5 mg/ml). Solubility in 45% aqueous (w/v) 2-hydroxypropyl-b- cyclodextrin (Cat. No. H-107): 6.4 mg/ml. Disposal: Dissolve or mix the compound with a combustible solvent and burn in a chemical incinerator equipped with an afterburner and scrubber. This product is controlled by the Drug Enforcement Administration. Appropriate security must be maintained until the substance is destroyed. Records must be kept which detail the ultimate disposition of the material. References: 1. Merck Index 11th Ed., No. 4113. 2. Saborido, A., Vila, J., Molano, F., Megias, A. “Effect of steroids on mitochondria and sarcotubular system of skeletal muscle.” J. Appl. Physiol. 70(3), 1038 (1991). 3. Fernandez, L., Chirino, R., Boada, L.D., Navarro, D., Cabrera, N., del Rio, I., Diaz-Chico, B.N. “Stanozolol and danazol, unlike natural androgens, interact with the low affinity glucocorticoid-binding sites from male rat liver microsomes.” Endocrinology 134(3), 1401 (1994). CONTROLLED SUBSTANCE - DEA LICENSE REQUIRED (III) Rev. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Determination of 17 Hormone Residues in Milk by Ultra-High-Performance Liquid Chromatography and Triple Quadrupole Mass Spectrom
No. LCMSMS-065E Liquid Chromatography Mass Spectrometry Determination of 17 Hormone Residues in Milk by Ultra-High-Performance Liquid Chromatography and Triple Quadrupole No. LCMSMS-65E Mass Spectrometry This application news presents a method for the determination of 17 hormone residues in milk using Shimadzu Ultra-High-Performance Liquid Chromatograph (UHPLC) LC-30A and Triple Quadrupole Mass Spectrometer LCMS- 8040. After sample pretreatment, the compounds in the milk matrix were separated using UPLC LC-30A and analyzed via Triple Quadrupole Mass Spectrometer LCMS-8040. All 17 hormones displayed good linearity within their respective concentration range, with correlation coefficient in the range of 0.9974 and 0.9999. The RSD% of retention time and peak area of 17 hormones at the low-, mid- and high- concentrations were in the range of 0.0102-0.161% and 0.563-6.55% respectively, indicating good instrument precision. Method validation was conducted and the matrix spike recovery of milk ranged between 61.00-110.9%. The limit of quantitation was 0.14-0.975 g/kg, and it meets the requirement for detection of hormones in milk. Keywords: Hormones; Milk; Solid phase extraction; Ultra performance liquid chromatograph; Triple quadrupole mass spectrometry ■ Introduction Since 2008’s melamine-tainted milk scandal, the With reference to China’s national standard GB/T adulteration of milk powder has become a major 21981-2008 "Hormone Multi-Residue Detection food safety concern. In recent years, another case of Method for Animal-derived Food - LC-MS Method", dairy product safety is suspected to cause "infant a method utilizing solid phase extraction, ultra- sexual precocity" (also known as precocious puberty) performance liquid chromatography and triple and has become another major issue challenging the quadrupole mass spectrometry was developed for dairy industry in China. -

Part I Biopharmaceuticals
1 Part I Biopharmaceuticals Translational Medicine: Molecular Pharmacology and Drug Discovery First Edition. Edited by Robert A. Meyers. © 2018 Wiley-VCH Verlag GmbH & Co. KGaA. Published 2018 by Wiley-VCH Verlag GmbH & Co. KGaA. 3 1 Analogs and Antagonists of Male Sex Hormones Robert W. Brueggemeier The Ohio State University, Division of Medicinal Chemistry and Pharmacognosy, College of Pharmacy, Columbus, Ohio 43210, USA 1Introduction6 2 Historical 6 3 Endogenous Male Sex Hormones 7 3.1 Occurrence and Physiological Roles 7 3.2 Biosynthesis 8 3.3 Absorption and Distribution 12 3.4 Metabolism 13 3.4.1 Reductive Metabolism 14 3.4.2 Oxidative Metabolism 17 3.5 Mechanism of Action 19 4 Synthetic Androgens 24 4.1 Current Drugs on the Market 24 4.2 Therapeutic Uses and Bioassays 25 4.3 Structure–Activity Relationships for Steroidal Androgens 26 4.3.1 Early Modifications 26 4.3.2 Methylated Derivatives 26 4.3.3 Ester Derivatives 27 4.3.4 Halo Derivatives 27 4.3.5 Other Androgen Derivatives 28 4.3.6 Summary of Structure–Activity Relationships of Steroidal Androgens 28 4.4 Nonsteroidal Androgens, Selective Androgen Receptor Modulators (SARMs) 30 4.5 Absorption, Distribution, and Metabolism 31 4.6 Toxicities 32 Translational Medicine: Molecular Pharmacology and Drug Discovery First Edition. Edited by Robert A. Meyers. © 2018 Wiley-VCH Verlag GmbH & Co. KGaA. Published 2018 by Wiley-VCH Verlag GmbH & Co. KGaA. 4 Analogs and Antagonists of Male Sex Hormones 5 Anabolic Agents 32 5.1 Current Drugs on the Market 32 5.2 Therapeutic Uses and Bioassays -

INTEGRIS Formulary July 2017
INTEGRIS Formulary July 2017 Foreword FORMULARY EXCLUDED THERAPEUTIC DRUG This document represents the efforts of the MedImpact Healthcare Systems THERAPEUTIC DRUGS CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide ALTERNATIVES physicians and pharmacists with a method to evaluate the safety, efficacy and cost- clindamycin/tretinoin, ACNE AGENTS, effectiveness of commercially available drug products. A structured approach to the VELTIN drug selection process is essential in ensuring continuing patient access to rational ZIANA TOPICAL drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ANALGESICS, KADIAN prescribing decisions that reflect the most current clinical consensus associated ER, NUCYNTA, NARCOTICS with drug therapy decisions. NUCYNTA ER ANALGESICS, This is accomplished through the auspices of the MedImpact P & T and Formulary BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, fentanyl citrate ANALGESICS, LAZANDA, lozenge NARCOTICS As you use this Formulary, you are encouraged to review the information and ONSOLIS, provide your input and comments to the MedImpact P & T and Formulary SUBSYS Committees. immediate-release GRALISE ANTICONVULSANTS The MedImpact P & T -

Anabolic Steroids/Androgens Pa Summary
ANABOLIC STEROIDS/ANDROGENS PA SUMMARY PREFERRED Anadrol-50, Danazol, Fluoxymesterone, Methitest, Oxandrolone, Testosterone Cypionate Injection, Testosterone Enanthate Injection NON-PREFERRED Android, Testred LENGTH OF AUTHORIZATION: Varies NOTE: All preferred and non-preferred agents require prior authorization. See PA criteria labeled “Topical Testosterone” for Androderm, Androgel, Striant, and Testim. The criteria details below are for the outpatient pharmacy program. If an injectable medication is being administered in a physician’s office then the criteria information below does not apply. Instead, the physician’s office must bill this drug through the DCH physician’s injectable program and not the outpatient pharmacy program. Information regarding the physician’s injectable program can be located at www.mmis.georgia.gov. PA CRITERIA: For Anadrol-50 Approvable for the following diagnoses: anemia caused by deficient red blood cell production, acquired or congenital aplastic anemia, myelofibrosis, hypoplastic anemia due to administration of myelotoxic drugs Also approvable for HIV or AIDS wasting when significant weight loss is documented in members currently receiving nutritional support For Danazol Approvable for the following diagnoses: endometriosis, fibrocystic breast disease, hereditary angioedema For Fluoxymesterone, Methyltestosterone (Android, Methitest, Testred), Testosterone Cypionate or Enanthate Injection Approvable in male members 12 years of age or older for the following diagnoses: primary hypogonadism, secondary -

Printed Formulary Catalog Basic
Scripps Health Formulary July 2016 Foreword Pharmacy and Therapeutics Committee. MedImpact approves such multi- This document represents the efforts of the MedImpact Healthcare Systems source drugs for addition to the MAC list based on the following criteria: Pharmacy and Therapeutics (P & T) and Formulary Committees to provide physicians A multi-source drug product manufactured by at least one (1) nationally and pharmacists with a method to evaluate the safety, efficacy and cost-effectiveness marketed company. of commercially available drug products. A structured approach to the drug selection At least one (1) of the generic manufacturer’s products must have an “A” process is essential in ensuring continuing patient access to rational drug therapies. rating or the generic product has been determined to be unassociated with The ultimate goal of the Portfolio Formulary is to provide a process and framework to efficacy, safety or bioequivalency concerns by the MedImpact P & T support the dynamic evolution of this document to guide prescribing decisions that Committee. reflect the most current clinical consensus associated with drug therapy decisions. Drug product will be approved for generic substitution by the MedImpact P & T Committee. This is accomplished through the auspices of the MedImpact P & T and Formulary Committees. These committees meet quarterly and more often as warranted to ensure This list is reviewed and updated periodically based on the clinical literature and clinical relevancy of the Formulary. To accommodate changes to this document, pharmacokinetic characteristics of currently available versions of these drug updates are made accessible as necessary. products. As you use this Formulary, you are encouraged to review the information and provide If a member or physician requests a brand name product in lieu of an approved your input and comments to the MedImpact P & T and Formulary Committees. -

Role of Androgens on MCF-7 Breast Cancer Cell Growth and on the Inhibitory Effect of Letrozole
Research Article Role of Androgens on MCF-7 Breast Cancer Cell Growth and on the Inhibitory Effect of Letrozole Luciana F. Macedo, Zhiyong Guo, Syreeta L. Tilghman, Gauri J. Sabnis, Yun Qiu, and Angela Brodie Department of Pharmacology and Experimental Therapeutics, University of Maryland, Baltimore, Maryland Abstract hormone therapy and longer patient survival (14). However, the Previous work has shown that androgens inhibit breast cancer physiologic role of endogenous androgens and events following AR cells and tumor growth. On the other hand, androgens can be activation leading to inhibition of cell growth are not clearly identified in breast cancer cells. Some studies have shown that converted to mitogenic estrogens by aromatase in breast cancer cells. Here, we report that androgens, such as the androgens modulate the expression of the Bcl-2protein family in aromatizable androstenedione and the non-aromatizable breast cancer cells, and that their effect is contrary to that of 5A-dihydrotestosterone, inhibit MCF-7 cell proliferation. This estrogens (15, 16). The Bcl-2family proteins both inhibit and effect is observed only in the absence or at a low concentra- promote cell death (16, 17), and the Bcl-2protein has been tion of estrogens and is evident in cells with low aromatase extensively characterized as an inhibitor of apoptosis. activity. Growth of a new aromatase stably transfected MCF-7 Due to their adverse side effects, exogenous androgens were later cell line (Ac1) was stimulated by conversion of androstene- replaced by other better tolerated breast cancer treatment dione into estrogens and was sensitive to aromatase inhib- strategies, such as ER antagonism and aromatase inhibition. -

Steroids and Other Appearance and Performance Enhancing Drugs (Apeds) Research Report
Research Report Revised Febrero 2018 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Table of Contents Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Introduction What are the different types of APEDs? What is the history of anabolic steroid use? Who uses anabolic steroids? Why are anabolic steroids misused? How are anabolic steroids used? What are the side effects of anabolic steroid misuse? How does anabolic steroid misuse affect behavior? What are the risks of anabolic steroid use in teens? How do anabolic steroids work in the brain? Are anabolic steroids addictive? How are anabolic steroids tested in athletes? What can be done to prevent steroid misuse? What treatments are effective for anabolic steroid misuse? Where can I get further information about steroids? References Page 1 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Esta publicación está disponible para su uso y puede ser reproducida, en su totalidad, sin pedir autorización al NIDA. Se agradece la citación de la fuente, de la siguiente manera: Fuente: Instituto Nacional sobre el Abuso de Drogas; Institutos Nacionales de la Salud; Departamento de Salud y Servicios Humanos de los Estados Unidos. Introduction Appearance and performance enhancing drugs (APEDs) are most often used by males to improve appearance by building muscle mass or to enhance athletic performance. Although they may directly and indirectly have effects on a user’s mood, they do not produce a euphoric high, which makes APEDs distinct from other drugs such as cocaine, heroin, and marijuana. However, users may develop a substance use disorder, defined as continued use despite adverse consequences. -

Control Be Implemented. the First Large-Scale Systematic Olympic Games
Br J Sports Med: first published as 10.1136/bjsm.11.4.162 on 1 December 1977. Downloaded from 162 Brit. J. Sports Med. - Vol. 1 1, No. 4, December 1977, pp. 162-169 RADIOIMMUNOASSAY OF ANABOLIC STEROIDS: AN EVALUATION OF THREE ANTISERA FOR THE DETECTION OF ANABOLIC STEROIDS IN BIOLOGICAL FLUIDS Robert DUGAL, Ph.D., Claire DUPUIS, Ph.D. and Michel J. BERTRAND, Ph.D. Centre de Recherches en Sciences de la Sante, Institut National de la Recherche Scientifique, Centre Hospitalier Louis-H. Lafontaine, Montrdal, Quebec, Canada ABSTRACT Recently developped radioimmunoassays (RIA) for the analysis of anabolic steroids and their metabolites in biological fluids were tested for cross-reactivity with other types of steroids. Results show that the degree of desirable cross-reactivity within the two classes of orally active anabolic steroids vary widely and that the antiserum for 19-Nortestosterone (the active principle of intramuscular, preparations) has a very high degree of undesirable cross- reactivity with components of oral contraceptives. Single and multiple dose studies in human volunteers demonstrate that the detection level and degree of retrospectivity are likewise variable but that the test easily detects most anabolic steroids during treatment. At the present time, the combination of the three antisera for the assay of a sample appears to be a relatively rapid and economic method for screening large numbers of samples in situations where doping control of anabolic steroids is required. The importance of utilizing physico-chemical means for identification of RIA potential positives is emphasized. INTRODUCTION (Sumner, 1974: Brooks et al, 1975) and identification procedures for a limited number of them have also been copyright. -

The Combined Cardiac Effect of the Anabolic Steroid, Nandrolone And
ù1. v -¿. rlc) 77.- *n*hi.rnool oowol,ù*o ffi"/fu -lo *rn*(o fii'o fio¿o¿¿, /v&"ùún lonno **al cooaiæe';¿vfl"- oã. Benjamin D. Phillis, B.Sc. (Hons) Phatmacology Depattment of Clinical & Experimental Pharmacology Ftome Rd. , Medical School Noth Adelaide Univetsity ADEIAIDE SA 5OOO û.)r.'-*hr/7enveltîù Foremost, I would like to thank my two supervisors for the direction that they have given this ptojecr. To Rod, for his unfailing troubleshooting abiJity and to Jenny fot her advice and ability to add scientific rigour' Many thanks to Michael Adams for his technical assistance and especially fot performing the surgery for the ischaemia-reperfusion projects and for his willingness to work late nights and public holidays. Lastly I would like to thank my v¡ife for her extreme patience during the tumult of the last 5 years. Her love, suppoït, patience and undetstanding have been invaluable in this endeavout. Beniamin D. Phillis Octobet,2005 ADE,I-AIDE ii T*(¿t of Ao,t",tù DECI.ARATION I ACKNOWLEDGEMENTS il TABLE OF CONTENTS UI ABBREVIATIONS x ABSTRACT )ilr CÉIAPTER t-l Inttoduction 1-1 1.1 Background 1,-1, 1.2What ate anabolic stetoids? 7-1 1,3 General pharmacology of Anabolic steroids t-2 '1,-2 1.3.1 Genomic effects of anabolic steroids 1.3.2 Non-genomic effects of anabolic steroids 1-3 1.4 Clinical use of AS 1.-4 1.5 Patterns of AS abuse 1.-4 1.5.1 Steroid abuse by athletes 1.-+ 1.5.2 Stetoid abuse by sedentary teenagers r-6 1.5.3 Prevalence of abuse 1-6 1.5.4 Abuse ptevalence in Australia 1.-9 1.6 Cardiotoxicity of anabolic steroids r-9 1.6.1 Reduced cotonary flow 1.-1.1, 1,.6.2 Dtect myocatdial eff ects 1-1 5 1.6.3 Hypertension 1-21 1.7 Difficulties associated with anabolic steroid research 1.-24 1-25 1.8 The polydrug abuse Phenomenon 1.9 The pharmacology of cocaine 1-26 1.10 Pteparations 1-28 1-29 1.11 Metabolism lll 1-30 1. -
Controlled Substances Listed in This Section from Schedule VI
Page 1 of 15 ARTICLE II Schedule I (a) Schedule I shall consist of the drugs and other substances, by whatever official name, common or usual name, chemical name, or brand name designated, listed in this section. Each drug or substance has been assigned the DEA Controlled Substances Code Number set forth opposite it. (b) Opiates: (Narcotic Drugs) Unless specifically excepted or unless listed in another schedule, any of the following opiates, including their isomers, esters, ethers, salts, and salts of isomers, esters, and ethers, whenever the existence of such isomers, esters, ethers, salts is possible within the specific chemical designation (for purposes of paragraph (b)(34) only, the term isomer includes the optical and geometric isomers): (1) Acetyl-alpha-methylfentanyl(N-[1-[1-methyl-2- phenethyl)-4-piperidinyl]-N-phenylacetamide) ----- 9815-(2-86) (2) Acetylmethadol ----------------------------------- 9601* (3) Allylprodine ------------------------------------- 9602* (4) Alphacetylmethadol (except Levo-alphacetylmethadol (LAAM)------------------------------- 9603* (5) Alphameprodine ----------------------------------- 9604* (6) Alphamethadol ------------------------------------ 9605* (7) Alpha-methylfentanyl (N-[1-(alpha-methyl-beta-phenyl) ethyl-4-piperidyl]propronanilide; 1-(1-methyl- 2-phenylethyl)-4(N-propanilido)piperidine) ------- 9814-(6-82) (8) Alpha-methylthiofentanyl(N-[1-methyl-2-(2thienyl) ethyl-4-piperidinyl]-N-phenylpropanamide) -------- 9832-(2-86) (9) Benzethidine ------------------------------------- 9606* (10)