Recognition and Management of Pesticide Poisonings Is an Up- Date and Expansion of the 1989 Fourth Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Is the Difference Between Pesticides, Insecticides and Herbicides? Pesticide Effects on Food Production
What is the Difference Between Pesticides, Insecticides and Herbicides? Pesticides are chemicals that may be used to kill fungus, bacteria, insects, plant diseases, snails, slugs, or weeds among others. These chemicals can work by ingestion or by touch and death may occur immediately or over a long period of time. Insecticides are a type of pesticide that is used to specifically target and kill insects. Some insecticides include snail bait, ant killer, and wasp killer. Herbicides are used to kill undesirable plants or “weeds”. Some herbicides will kill all the plants they touch, while others are designed to target one species. Pesticide Effects on Food Production As the human population continues to grow, more and more crops are needed to meet this growing demand. This has increased the use of pesticides to increase crop yield per acre. For example, many farmers will plant a field with Soybeans and apply two doses of Roundup throughout the growing year to remove all other plants and prepare the field for next year’s crop. The Roundup is applied twice through the growing season to kill everything except the soybeans, which are modified to be pesticide resistant. After the soybeans are harvested, there is little vegetative cover on the field creating potential erosion issues for the reason that another crop can easily be planted. With this method, hundreds of gallons of chemicals are introduced into the environment every year. All these chemicals affect wildlife, insects, water quality and air quality. One greatly affected “good” insect are bees. Bees play a significant role in the pollination of the foods that we eat. -

Novel Approach to Fast Determination of 64 Pesticides Using of Ultra-Performance Liquid Chromatography-Tandem Mass Spectrometry
Novel approach to fast determination of 64 pesticides using of ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) Tomas Kovalczuk, Ondrej Lacina, Martin Jech, Jan Poustka, Jana Hajslova To cite this version: Tomas Kovalczuk, Ondrej Lacina, Martin Jech, Jan Poustka, Jana Hajslova. Novel approach to fast determination of 64 pesticides using of ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS). Food Additives and Contaminants, 2008, 25 (04), pp.444-457. 10.1080/02652030701570156. hal-00577414 HAL Id: hal-00577414 https://hal.archives-ouvertes.fr/hal-00577414 Submitted on 17 Mar 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Food Additives and Contaminants For Peer Review Only Novel approach to fast determination of 64 pesticides using of ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) Journal: Food Additives and Contaminants Manuscript ID: TFAC-2007-065.R1 Manuscript Type: Original Research Paper Date Submitted by the 07-Jul-2007 Author: Complete List of Authors: -
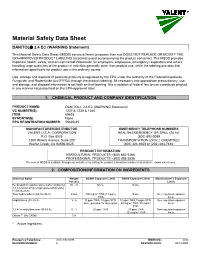
Material Safety Data Sheet
Material Safety Data Sheet DANITOL 2.4 EC (WARNING Statement) This Material Safety Data Sheet (MSDS) serves different purposes than and DOES NOT REPLACE OR MODIFY THE EPA-APPROVED PRODUCT LABELING (attached to and accompanying the product container). This MSDS provides important health, safety, and environmental information for employers, employees, emergency responders and others handling large quantities of the product in activities generally other than product use, while the labeling provides that information specifically for product use in the ordinary course. Use, storage and disposal of pesticide products is regulated by the EPA under the authority of the Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA) through the product labeling. All necessary and appropriate precautionary, use, and storage, and disposal information is set forth on that labeling. It is a violation of federal law to use a pesticide product in any manner not prescribed on the EPA-approved label. 1. CHEMICAL PRODUCT AND COMPANY IDENTIFICATION PRODUCT NAME: DANITOL 2.4 EC (WARNING Statement) VC NUMBER(S): 1237 & 1238 & 1340 ITEM: 69625 SYNONYM(S): None EPA REGISTRATION NUMBER: 59639-35 MANUFACTURER/DISTRIBUTOR EMERGENCY TELEPHONE NUMBERS VALENT U.S.A. CORPORATION HEALTH EMERGENCY OR SPILL (24 hr): P.O. Box 8025 (800) 892-0099 1600 Riviera Avenue, Suite 200 TRANSPORTATION (24 hr.): CHEMTREC Walnut Creek, CA 94596-8025. (800) 424-9300 or (202) 483-7616. PRODUCT INFORMATION AGRICULTURAL PRODUCTS: (800) 682-5368 PROFESSIONAL PRODUCTS: (800) 898-2536 The current MSDS is available through our website or by calling the product information numbers listed above. (www.valent.com) 2. COMPOSITION/INFORMATION ON INGREDIENTS Chemical Name Weight/ ACGIH Exposure Limits OSHA Exposure Limits Manufacturer's Exposure Percent Limits Fenpropathrin (alpha-cyano-3-phenoxybenzyl 30 - 32 None. -

Historical Perspectives on Apple Production: Fruit Tree Pest Management, Regulation and New Insecticidal Chemistries
Historical Perspectives on Apple Production: Fruit Tree Pest Management, Regulation and New Insecticidal Chemistries. Peter Jentsch Extension Associate Department of Entomology Cornell University's Hudson Valley Lab 3357 Rt. 9W; PO box 727 Highland, NY 12528 email: [email protected] Phone 845-691-7151 Mobile: 845-417-7465 http://www.nysaes.cornell.edu/ent/faculty/jentsch/ 2 Historical Perspectives on Fruit Production: Fruit Tree Pest Management, Regulation and New Chemistries. by Peter Jentsch I. Historical Use of Pesticides in Apple Production Overview of Apple Production and Pest Management Prior to 1940 Synthetic Pesticide Development and Use II. Influences Changing the Pest Management Profile in Apple Production Chemical Residues in Early Insect Management Historical Chemical Regulation Recent Regulation Developments Changing Pest Management Food Quality Protection Act of 1996 The Science Behind The Methodology Pesticide Revisions – Requirements For New Registrations III. Resistance of Insect Pests to Insecticides Resistance Pest Management Strategies IV. Reduced Risk Chemistries: New Modes of Action and the Insecticide Treadmill Fermentation Microbial Products Bt’s, Abamectins, Spinosads Juvenile Hormone Analogs Formamidines, Juvenile Hormone Analogs And Mimics Insect Growth Regulators Azadirachtin, Thiadiazine Neonicotinyls Major Reduced Risk Materials: Carboxamides, Carboxylic Acid Esters, Granulosis Viruses, Diphenyloxazolines, Insecticidal Soaps, Benzoyl Urea Growth Regulators, Tetronic Acids, Oxadiazenes , Particle Films, Phenoxypyrazoles, Pyridazinones, Spinosads, Tetrazines , Organotins, Quinolines. 3 I Historical Use of Pesticides in Apple Production Overview of Apple Production and Pest Management Prior to 1940 The apple has a rather ominous origin. Its inception is framed in the biblical text regarding the genesis of mankind. The backdrop appears to be the turbulent setting of what many scholars believe to be present day Iraq. -
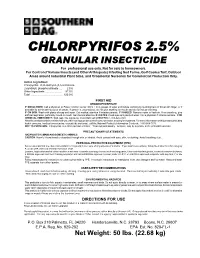
CHLORPYRIFOS 2.5% GRANULAR INSECTICIDE for Professional Use Only
CHLORPYRIFOS 2.5% GRANULAR INSECTICIDE For professional use only. Not for sale to homeowners. For Control of Various Insects (and Other Arthropods) Infesting Sod Farms, Golf Course Turf, Outdoor Areas around Industrial Plant Sites, and Ornamental Nurseries for Commercial Production Only. Active Ingredient: Chlorpyrifos: O,O-diethyl-0-(3,5,6-trichloro- 2-pyridinyl) phosphorothioate .... 2.5% Other Ingredients ....................... 97.5% Total ............................................ 100.0% FIRST AID ORGANOPHOSPHATE IF SWALLOWED: Call a physician or Poison Control Center. Drink 1 or 2 glasses of water and induce vomiting by touching back of throat with finger, or if available by administering syrup of ipecac. If person is unconscious, do not give anything by mouth and do not induce vomiting. IF ON SKIN: Wash with plenty of soap and water. Get medical attention if irritation persists. IF INHALED: Remove victim to fresh air. If not breathing, give artificial respiration, preferably mouth-to-mouth. Get medical attention. IF IN EYES: Flush eyes with plenty of water. Call a physician if irritation persists. FOR CHEMICAL EMERGENCY: Spill, leak, fire, exposure, or accident call CHEMTREC 1-800-424-9300. Have the product container or label with you when calling a poison control center or doctor, or going for treatment. For more information on this product (including health concerns, medical emergencies, or pesticide incidents), call the National Pesticide Information Center at: 1-800-858-7378. NOT TO PHYSICIAN: Chlorpyrifos is a cholinesterase inhibitor. Treat symptomatically. Atropine, only by injection, is the preferable antidote. PRECAUTIONARY STATEMENTS HAZARDS TO HUMANS AND DOMESTIC ANIMALS CAUTION: Harmful if swallowed or absorbed through skin or inhaled. -

WO 2010/128115 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 11 November 2010 (11.11.2010) WO 2010/128115 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C12N 9/16 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (21) International Application Number: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, PCT/EP20 10/056204 DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 6 May 2010 (06.05.2010) KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (25) Filing Language: English NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (26) Publication Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 09159520.7 6 May 2009 (06.05.2009) EP (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant (for all designated States except US): GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, NOVOZYMES A/S [DK/DK]; Krogshoejvej 36, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, DK-2880 Bagsvaerd (DK). -

Activated Carbon, Biochar and Charcoal: Linkages and Synergies Across Pyrogenic Carbon’S Abcs
water Review Activated Carbon, Biochar and Charcoal: Linkages and Synergies across Pyrogenic Carbon’s ABCs Nikolas Hagemann 1,* ID , Kurt Spokas 2 ID , Hans-Peter Schmidt 3 ID , Ralf Kägi 4, Marc Anton Böhler 5 and Thomas D. Bucheli 1 1 Agroscope, Environmental Analytics, Reckenholzstrasse 191, CH-8046 Zurich, Switzerland; [email protected] 2 United States Department of Agriculture, Agricultural Research Service, Soil and Water Management Unit, St. Paul, MN 55108, USA; [email protected] 3 Ithaka Institute, Ancienne Eglise 9, CH-1974 Arbaz, Switzerland; [email protected] 4 Eawag, Swiss Federal Institute of Aquatic Science and Technology, Department Process Engineering, Überlandstrasse 133, CH-8600 Dübendorf, Switzerland; [email protected] 5 Eawag, Swiss Federal Institute of Aquatic Science and Technology, Application and Development, Department Process Engineering, Überlandstrasse 133, CH-8600 Dübendorf, Switzerland; [email protected] * Correspondence: [email protected]; Tel.: +41-58-462-1074 Received: 11 January 2018; Accepted: 1 February 2018; Published: 9 February 2018 Abstract: Biochar and activated carbon, both carbonaceous pyrogenic materials, are important products for environmental technology and intensively studied for a multitude of purposes. A strict distinction between these materials is not always possible, and also a generally accepted terminology is lacking. However, research on both materials is increasingly overlapping: sorption and remediation are the domain of activated carbon, which nowadays is also addressed by studies on biochar. Thus, awareness of both fields of research and knowledge about the distinction of biochar and activated carbon is necessary for designing novel research on pyrogenic carbonaceous materials. Here, we describe the dividing ranges and common grounds of biochar, activated carbon and other pyrogenic carbonaceous materials such as charcoal based on their history, definition and production technologies. -

Pesticide Resistance Management an Insect Perspective
PesticidePesticide ResistanceResistance ManagementManagement AnAn InsectInsect PerspectivePerspective FrankFrank Zalom,Zalom, Dept.Dept. ofof Entomology,Entomology, UCUC DavisDavis NickNick Toscano,Toscano, DeptDept ofof Entomology,Entomology, UCUC RiversideRiverside FrankFrank Byrne,Byrne, DeptDept ofof Entomology,Entomology, UCUC RiversideRiverside InsecticideInsecticide resistanceresistance isis duedue toto aa geneticgenetic traittrait aa pestpest inheritsinherits thatthat allowsallows itit toto survivesurvive anan applicationapplication thatthat mostmost otherother individualsindividuals inin thethe populationpopulation cannotcannot survive.survive. TheThe survivorsurvivor thenthen passespasses thethe genesgenes forfor resistanceresistance onon toto thethe nextnext generation.generation. X TheThe moremore thethe insecticideinsecticide isis used,used, thethe moremore quicklyquickly susceptiblesusceptible individualsindividuals areare eliminatedeliminated andand thethe fasterfaster thethe proportionproportion ofof resistantresistant individualsindividuals increasesincreases inin thethe population.population. X X X X X X IncreasingIncreasing pesticidepesticide ratesrates ResistanceResistance MechanismsMechanisms InsecticideInsecticide avoidanceavoidance behaviorsbehaviors -- • InsectsInsects maymay changechange theirtheir behaviorbehavior inin orderorder toto avoidavoid thethe pesticide.pesticide. BiochemicalBiochemical mechanismsmechanisms -- • ResistantResistant insectsinsects possesposses enzymesenzymes thatthat breakbreak downdown -

Toxicity Reduction Evaluation Guidance for Municipal Wastewater Treatment Plants EPA/833B-99/002 August 1999
United States Office of Wastewater EPA/833B-99/002 Environmental Protection Management August 1999 Agency Washington DC 20460 Toxicity Reduction Evaluation Guidance for Municipal Wastewater Treatment Plants EPA/833B-99/002 August 1999 Toxicity Reduction Evaluation Guidance for Municipal Wastewater Treatment Plants Office of Wastewater Management U.S. Environmental Protection Agency Washington, D.C. 20460 Notice and Disclaimer The U.S. Environmental Protection Agency, through its Office of Water, has funded, managed, and collaborated in the development of this guidance, which was prepared under order 7W-1235-NASX to Aquatic Sciences Consulting; order 5W-2260-NASA to EA Engineering, Science and Technology, Inc.; and contracts 68-03-3431, 68-C8-002, and 68-C2-0102 to Parsons Engineering Science, Inc. It has been subjected to the Agency's peer and administrative review and has been approved for publication. The statements in this document are intended solely as guidance. This document is not intended, nor can it be relied on, to create any rights enforceable by any party in litigation with the United States. EPA and State officials may decide to follow the guidance provided in this document, or to act at variance with the guidance, based on an analysis of site-specific circumstances. This guidance may be revised without public notice to reflect changes in EPA policy. ii Foreword This document is intended to provide guidance to permittees, permit writers, and consultants on the general approach and procedures for conducting toxicity reduction evaluations (TREs) at municipal wastewater treatment plants. TREs are important tools for Publicly Owned Treatment Works (POTWs) to use to identify and reduce or eliminate toxicity in a wastewater discharge. -

Development of a CEN Standardised Method for Liquid Chromatography Coupled to Accurate Mass Spectrometry
Development of a CEN standardised method for liquid chromatography coupled to accurate mass spectrometry CONTENTS 1. Aim and scope ................................................................................................................. 2 2. Short description ................................................................................................................ 2 3. Apparatus and consumables ......................................................................................... 2 4. Chemicals ........................................................................................................................... 2 5. Procedure ........................................................................................................................... 3 5.1. Sample preparation ................................................................................................... 3 5.2. Recovery experiments for method validation ...................................................... 3 5.3. Extraction method ...................................................................................................... 3 5.4. Measurement .............................................................................................................. 3 5.5. Instrumentation and analytical conditions ............................................................ 4 5.5.1. Dionex Ultimate 3000 .......................................................................................... 4 5.5.2. QExactive Focus HESI source parameters ..................................................... -

Fipronil Poisoning Presenting As Sinus Bradycardia - a Rare Case Report
Jemds.com Case Report Fipronil Poisoning Presenting as Sinus Bradycardia - A Rare Case Report Abhijit Wadekar1, Sreekarthik Pratapa2, Maharshi Patel3, Shilpa Gaidhane4, Nazli Khatib5, 1, 2, 3, 4 Department of Medicine, Acharya Vinoba Bhave Rural Hospital, Sawangi, Wardha, Maharashtra, India. 5 Department of Physiology, Acharya Vinoba Bhave Rural Hospital, Sawangi, Wardha, Maharashtra, India. INTRODUCTION Fipronil is an N-phenylpyrazole insecticide, a second-generation insecticide which is Corresponding Author: relatively new and now commonly used in cotton growing community of rural Central Dr. Shilpa Gaidhane, India. Farmer suicide and deliberate self-poisoning is menace to the Vidarbha region Department of Medicine, of rural Central India. There is paucity of research published on fipronil poisoning, Acharya Vinoba Bhave Rural Hospital, Sawangi, Wardha, Maharashtra, India. clinical features, complications and treatment data. It is scarcely documented E-mail: [email protected] worldwide. Agricultural insecticides are common household items in rural areas of DOI: 10.14260/jemds/2021/247 developing countries. Because of their easy availability, insecticides became a major source of deliberate self-poisoning. As per World Health Organization (WHO), around How to Cite This Article: 3 million poisoning cases with around 0.2 million deaths are noted annually in the Wadekar A, Pratapa S, Patel M, et al. world.1 About 99 % of these deaths occur in developing countries. Insecticide Fipronil poisoning presenting as sinus poisoning is an important public issue in India. Around 168,000 deaths occurred from bradycardia - a rare case report. J Evolution Med Dent Sci 2021;10(16):1166-1168, DOI: pesticide self-poisoning which totals to almost 19.7 % of the global suicides.2 The 10.14260/jemds/2021/247 most common cause of self-poisoning in Central India is ingestion of organophosphorus compounds (OPC). -

Historical Use of Lead Arsenate and Survey of Soil Residues in Former Apple Orchards in Virginia
HISTORICAL USE OF LEAD ARSENATE AND SURVEY OF SOIL RESIDUES IN FORMER APPLE ORCHARDS IN VIRGINIA by Therese Nowak Schooley Thesis submitted to the faculty of the Virginia Polytechnic Institute and State University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE IN LIFE SCIENCES in Entomology Michael J. Weaver, Chair Donald E. Mullins, Co-Chair Matthew J. Eick May 4, 2006 Blacksburg, Virginia Keywords: arsenic, lead, lead arsenate, orchards, soil residues, historical pesticides HISTORICAL USE OF LEAD ARSENATE AND SURVEY OF SOIL RESIDUES IN FORMER APPLE ORCHARDS IN VIRGINIA Therese Nowak Schooley Abstract Inorganic pesticides including natural chemicals such as arsenic, copper, lead, and sulfur have been used extensively to control pests in agriculture. Lead arsenate (PbHAsO4) was first used in apple orchards in the late 1890’s to combat the codling moth, Cydia pomonella (Linnaeus). The affordable and persistent pesticide was applied in ever increasing amounts for the next half century. The persistence in the environment in addition to the heavy applications during the early 1900’s may have led to many of the current and former orchards in this country being contaminated. In this study, soil samples were taken from several apple orchards across the state, ranging from Southwest to Northern Virginia and were analyzed for arsenic and lead. Based on naturally occurring background levels and standards set by other states, two orchards sampled in this study were found to have very high levels of arsenic and lead in the soil, Snead Farm and Mint Spring Recreational Park. Average arsenic levels at Mint Spring Recreational Park and Snead Farm were found to be 65.2 ppm and 107.6 ppm, respectively.