Phenotype – Genotype Correlations in Leigh Syndrome: New Insights from a Multicenter Study of 96 Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NDUFAF1 Antibody
Efficient Professional Protein and Antibody Platforms NDUFAF1 Antibody Basic information: Catalog No.: UPA63763 Source: Rabbit Size: 50ul/100ul Clonality: monoclonal Concentration: 1mg/ml Isotype: Rabbit IgG Purification: Protein A purified. Useful Information: WB:1:1000 ICC:1:50-1:200 Applications: IHC:1:50-1:200 FC:1:50-1:100 Reactivity: Human Specificity: This antibody recognizes NDUFAF1 protein. Immunogen: Synthetic peptide within C terminal human NDUFAF1. This gene encodes a complex I assembly factor protein. Complex I (NADH-ubiquinone oxidoreductase) catalyzes the transfer of electrons from NADH to ubiquinone (coenzyme Q) in the first step of the mitochondrial respiratory chain, resulting in the translocation of protons across the inner mitochondrial membrane. The encoded protein is required for assembly of complex I, and mutations in this gene are a cause of mitochondrial complex I deficiency. Alternatively spliced transcript variants have been observed for Description: this gene, and a pseudogene of this gene is located on the long arm of chromosome 19. Part of the mitochondrial complex I assembly (MCIA) com- plex. The complex comprises at least TMEM126B, NDUFAF1, ECSIT, and ACAD9. Interacts with ECSIT. Interacts with ACAD9. At early stages of com- plex I assembly, it is found in intermediate subcomplexes that contain dif- ferent subunits including NDUFB6, NDUFA6, NDUFA9, NDUFS3, NDUFS7, ND1, ND2 and ND3 Uniprot: Q9Y375 Human BiowMW: 38 kDa Buffer: 1*TBS (pH7.4), 1%BSA, 50%Glycerol. Preservative: 0.05% Sodium Azide. Storage: Store at 4°C short term and -20°C long term. Avoid freeze-thaw cycles. Note: For research use only, not for use in diagnostic procedure. -

Molecular Mechanism of ACAD9 in Mitochondrial Respiratory Complex 1 Assembly
bioRxiv preprint doi: https://doi.org/10.1101/2021.01.07.425795; this version posted January 9, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Molecular mechanism of ACAD9 in mitochondrial respiratory complex 1 assembly Chuanwu Xia1, Baoying Lou1, Zhuji Fu1, Al-Walid Mohsen2, Jerry Vockley2, and Jung-Ja P. Kim1 1Department of Biochemistry, Medical College of Wisconsin, Milwaukee, Wisconsin, 53226, USA 2Department of Pediatrics, University of Pittsburgh School of Medicine, University of Pittsburgh, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA 15224, USA Abstract ACAD9 belongs to the acyl-CoA dehydrogenase family, which catalyzes the α-β dehydrogenation of fatty acyl-CoA thioesters. Thus, it is involved in fatty acid β-oxidation (FAO). However, it is now known that the primary function of ACAD9 is as an essential chaperone for mitochondrial respiratory complex 1 assembly. ACAD9 interacts with ECSIT and NDUFAF1, forming the mitochondrial complex 1 assembly (MCIA) complex. Although the role of MCIA in the complex 1 assembly pathway is well studied, little is known about the molecular mechanism of the interactions among these three assembly factors. Our current studies reveal that when ECSIT interacts with ACAD9, the flavoenzyme loses the FAD cofactor and consequently loses its FAO activity, demonstrating that the two roles of ACAD9 are not compatible. ACAD9 binds to the carboxy-terminal half (C-ECSIT), and NDUFAF1 binds to the amino-terminal half of ECSIT. Although the binary complex of ACAD9 with ECSIT or with C-ECSIT is unstable and aggregates easily, the ternary complex of ACAD9-ECSIT-NDUFAF1 (i.e., the MCIA complex) is soluble and extremely stable. -

Two Transgenic Mouse Models for Β-Subunit Components of Succinate-Coa Ligase Yielding Pleiotropic Metabolic Alterations
Two transgenic mouse models for -subunit components of succinate-CoA ligase yielding pleiotropic metabolic alterations Kacso, Gergely; Ravasz, Dora; Doczi, Judit; Németh, Beáta; Madgar, Ory; Saada, Ann; Ilin, Polina; Miller, Chaya; Ostergaard, Elsebet; Iordanov, Iordan; Adams, Daniel; Vargedo, Zsuzsanna; Araki, Masatake; Araki, Kimi; Nakahara, Mai; Ito, Haruka; Gál, Aniko; Molnár, Mária J; Nagy, Zsolt; Patocs, Attila; Adam-Vizi, Vera; Chinopoulos, Christos Published in: Biochemical Journal DOI: 10.1042/BCJ20160594 Publication date: 2016 Document version Publisher's PDF, also known as Version of record Document license: CC BY Citation for published version (APA): Kacso, G., Ravasz, D., Doczi, J., Németh, B., Madgar, O., Saada, A., Ilin, P., Miller, C., Ostergaard, E., Iordanov, I., Adams, D., Vargedo, Z., Araki, M., Araki, K., Nakahara, M., Ito, H., Gál, A., Molnár, M. J., Nagy, Z., ... Chinopoulos, C. (2016). Two transgenic mouse models for -subunit components of succinate-CoA ligase yielding pleiotropic metabolic alterations. Biochemical Journal, 473(20), 3463-3485. https://doi.org/10.1042/BCJ20160594 Download date: 02. okt.. 2021 Biochemical Journal (2016) 473 3463–3485 DOI: 10.1042/BCJ20160594 Research Article Two transgenic mouse models for β-subunit components of succinate-CoA ligase yielding pleiotropic metabolic alterations Gergely Kacso1,2, Dora Ravasz1,2, Judit Doczi1,2, Beáta Németh1,2, Ory Madgar1,2, Ann Saada3, Polina Ilin3, Chaya Miller3, Elsebet Ostergaard4, Iordan Iordanov1,5, Daniel Adams1,2, Zsuzsanna Vargedo1,2, Masatake -

High-Throughput, Pooled Sequencing Identifies Mutations in NUBPL And
ARTICLES High-throughput, pooled sequencing identifies mutations in NUBPL and FOXRED1 in human complex I deficiency Sarah E Calvo1–3,10, Elena J Tucker4,5,10, Alison G Compton4,10, Denise M Kirby4, Gabriel Crawford3, Noel P Burtt3, Manuel Rivas1,3, Candace Guiducci3, Damien L Bruno4, Olga A Goldberger1,2, Michelle C Redman3, Esko Wiltshire6,7, Callum J Wilson8, David Altshuler1,3,9, Stacey B Gabriel3, Mark J Daly1,3, David R Thorburn4,5 & Vamsi K Mootha1–3 Discovering the molecular basis of mitochondrial respiratory chain disease is challenging given the large number of both mitochondrial and nuclear genes that are involved. We report a strategy of focused candidate gene prediction, high-throughput sequencing and experimental validation to uncover the molecular basis of mitochondrial complex I disorders. We created seven pools of DNA from a cohort of 103 cases and 42 healthy controls and then performed deep sequencing of 103 candidate genes to identify 151 rare variants that were predicted to affect protein function. We established genetic diagnoses in 13 of 60 previously unsolved cases using confirmatory experiments, including cDNA complementation to show that mutations in NUBPL and FOXRED1 can cause complex I deficiency. Our study illustrates how large-scale sequencing, coupled with functional prediction and experimental validation, can be used to identify causal mutations in individual cases. Complex I of the mitochondrial respiratory chain is a large ~1-MDa assembly factors are probably required, as suggested by the 20 factors macromolecular machine composed of 45 protein subunits encoded necessary for assembly of the smaller complex IV9 and by cohort by both the nuclear and mitochondrial (mtDNA) genomes. -

Neurodevelopmental Signatures of Narcotic and Neuropsychiatric Risk Factors in 3D Human-Derived Forebrain Organoids
Molecular Psychiatry www.nature.com/mp ARTICLE OPEN Neurodevelopmental signatures of narcotic and neuropsychiatric risk factors in 3D human-derived forebrain organoids 1 1 1 1 2 2 3 Michael Notaras , Aiman Lodhi , Estibaliz✉ Barrio-Alonso , Careen Foord , Tori Rodrick , Drew Jones , Haoyun Fang , David Greening 3,4 and Dilek Colak 1,5 © The Author(s) 2021 It is widely accepted that narcotic use during pregnancy and specific environmental factors (e.g., maternal immune activation and chronic stress) may increase risk of neuropsychiatric illness in offspring. However, little progress has been made in defining human- specific in utero neurodevelopmental pathology due to ethical and technical challenges associated with accessing human prenatal brain tissue. Here we utilized human induced pluripotent stem cells (hiPSCs) to generate reproducible organoids that recapitulate dorsal forebrain development including early corticogenesis. We systemically exposed organoid samples to chemically defined “enviromimetic” compounds to examine the developmental effects of various narcotic and neuropsychiatric-related risk factors within tissue of human origin. In tandem experiments conducted in parallel, we modeled exposure to opiates (μ-opioid agonist endomorphin), cannabinoids (WIN 55,212-2), alcohol (ethanol), smoking (nicotine), chronic stress (human cortisol), and maternal immune activation (human Interleukin-17a; IL17a). Human-derived dorsal forebrain organoids were consequently analyzed via an array of unbiased and high-throughput analytical approaches, including state-of-the-art TMT-16plex liquid chromatography/mass- spectrometry (LC/MS) proteomics, hybrid MS metabolomics, and flow cytometry panels to determine cell-cycle dynamics and rates of cell death. This pipeline subsequently revealed both common and unique proteome, reactome, and metabolome alterations as a consequence of enviromimetic modeling of narcotic use and neuropsychiatric-related risk factors in tissue of human origin. -

A Minimum-Labeling Approach for Reconstructing Protein Networks Across Multiple Conditions
A Minimum-Labeling Approach for Reconstructing Protein Networks across Multiple Conditions Arnon Mazza1, Irit Gat-Viks2, Hesso Farhan3, and Roded Sharan1 1 Blavatnik School of Computer Science, Tel Aviv University, Tel Aviv 69978, Israel. Email: [email protected]. 2 Dept. of Cell Research and Immunology, Tel Aviv University, Tel Aviv 69978, Israel. 3 Biotechnology Institute Thurgau, University of Konstanz, Unterseestrasse 47, CH-8280 Kreuzlingen, Switzerland. Abstract. The sheer amounts of biological data that are generated in recent years have driven the development of network analysis tools to fa- cilitate the interpretation and representation of these data. A fundamen- tal challenge in this domain is the reconstruction of a protein-protein sub- network that underlies a process of interest from a genome-wide screen of associated genes. Despite intense work in this area, current algorith- mic approaches are largely limited to analyzing a single screen and are, thus, unable to account for information on condition-specific genes, or reveal the dynamics (over time or condition) of the process in question. Here we propose a novel formulation for network reconstruction from multiple-condition data and devise an efficient integer program solution for it. We apply our algorithm to analyze the response to influenza in- fection in humans over time as well as to analyze a pair of ER export related screens in humans. By comparing to an extant, single-condition tool we demonstrate the power of our new approach in integrating data from multiple conditions in a compact and coherent manner, capturing the dynamics of the underlying processes. 1 Introduction With the increasing availability of high-throughput data, network biol- arXiv:1307.7803v1 [q-bio.QM] 30 Jul 2013 ogy has become the method of choice for filtering, interpreting and rep- resenting these data. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Complex I Deficiency Due to Loss of Ndufs4 in the Brain Results
Complex I deficiency due to loss of Ndufs4 in the brain results in progressive encephalopathy resembling Leigh syndrome Albert Quintanaa,1, Shane E. Krusea,1, Raj P. Kapurb, Elisenda Sanzc, and Richard D. Palmitera,2 aHoward Hughes Medical Institute and Department of Biochemistry, University of Washington, Seattle, WA 98195; bDepartment of Laboratories, Seattle Children’s Hospital, Seattle, WA 98105; and cDepartment of Pharmacology, University of Washington, Seattle, WA 98195 Contributed by Richard D. Palmiter, May 5, 2010 (sent for review April 22, 2010) To explore the lethal, ataxic phenotype of complex I deficiency in least one intact Ndufs4 allele are indistinguishable from WT Ndufs4 knockout (KO) mice, we inactivated Ndufs4 selectively in mice, and they are sometimes used interchangeably with WT as neurons and glia (NesKO mice). NesKO mice manifested the same controls (CT). To examine the role of the CNS in pathology, we symptoms as KO mice including retarded growth, loss of motor restricted the inactivation of Ndufs4 gene to neurons and lox/lox ability, breathing abnormalities, and death by ∼7 wk. Progressive astroglial cells by crossing the Ndufs4 mice with mice neuronal deterioration and gliosis in specific brain areas corre- expressing Cre recombinase from the Nestin locus (19) to create sponded to behavioral changes as the disease advanced, with mice that we refer to as NesKO mice. We confirmed that Nestin- early involvement of the olfactory bulb, cerebellum, and vestibular Cre results in recombination primarily in the CNS by crossing the nuclei. Neurons, particularly in these brain regions, had aberrant mice with a Rosa26-reporter line and by PCR analysis of DNA mitochondrial morphology. -
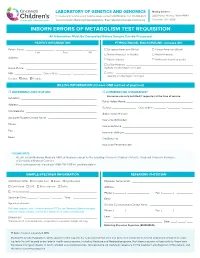
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

Genes Investigated
BabyNEXTTM EXTENDED Investigated genes and associated diseases Gene Disease OMIM OMIM Condition RUSP gene Disease ABCC8 Familial hyperinsulinism 600509 256450 Metabolic disorder - ABCC8-related Inborn error of amino acid metabolism ABCD1 Adrenoleukodystrophy 300371 300100 Miscellaneous RUSP multisystem (C) * diseases ABCD4 Methylmalonic aciduria and 603214 614857 Metabolic disorder - homocystinuria, cblJ type Inborn error of amino acid metabolism ACAD8 Isobutyryl-CoA 604773 611283 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of (S) ** organic acid metabolism ACAD9 acyl-CoA dehydrogenase-9 611103 611126 Metabolic Disorder - (ACAD9) deficiency Inborn error of fatty acid metabolism ACADM Acyl-CoA dehydrogenase, 607008 201450 Metabolic Disorder - RUSP medium chain, deficiency of Inborn error of fatty (C) acid metabolism ACADS Acyl-CoA dehydrogenase, 606885 201470 Metabolic Disorder - RUSP short-chain, deficiency of Inborn error of fatty (S) acid metabolism ACADSB 2-methylbutyrylglycinuria 600301 610006 Metabolic Disorder - RUSP Inborn error of (S) organic acid metabolism ACADVL very long-chain acyl-CoA 609575 201475 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of fatty (C) acid metabolism ACAT1 Alpha-methylacetoacetic 607809 203750 Metabolic Disorder - RUSP aciduria Inborn error of (C) organic acid metabolism ACSF3 Combined malonic and 614245 614265 Metabolic Disorder - methylmalonic aciduria Inborn error of organic acid metabolism 1 ADA Severe combined 608958 102700 Primary RUSP immunodeficiency due -

Proteomic and Metabolomic Analyses of Mitochondrial Complex I-Deficient
THE JOURNAL OF BIOLOGICAL CHEMISTRY VOL. 287, NO. 24, pp. 20652–20663, June 8, 2012 © 2012 by The American Society for Biochemistry and Molecular Biology, Inc. Published in the U.S.A. Proteomic and Metabolomic Analyses of Mitochondrial Complex I-deficient Mouse Model Generated by Spontaneous B2 Short Interspersed Nuclear Element (SINE) Insertion into NADH Dehydrogenase (Ubiquinone) Fe-S Protein 4 (Ndufs4) Gene*□S Received for publication, November 25, 2011, and in revised form, April 5, 2012 Published, JBC Papers in Press, April 25, 2012, DOI 10.1074/jbc.M111.327601 Dillon W. Leong,a1 Jasper C. Komen,b1 Chelsee A. Hewitt,a Estelle Arnaud,c Matthew McKenzie,d Belinda Phipson,e Melanie Bahlo,e,f Adrienne Laskowski,b Sarah A. Kinkel,a,g,h Gayle M. Davey,g William R. Heath,g Anne K. Voss,a,h René P. Zahedi,i James J. Pitt,j Roman Chrast,c Albert Sickmann,i,k Michael T. Ryan,l Gordon K. Smyth,e,f,h b2 a,h,m,n3 David R. Thorburn, and Hamish S. Scott Downloaded from From the aMolecular Medicine Division, gImmunology Division, and eBioinformatics Division, Walter and Eliza Hall Institute of Medical Research, Parkville, Victoria 3052, Australia, the bMurdoch Childrens Research Institute, Royal Children’s Hospital and Department of Paediatrics, University of Melbourne, Parkville, Victoria 3052, Australia, the cDépartement de Génétique Médicale, Université de Lausanne, 1005 Lausanne, Switzerland, the dCentre for Reproduction and Development, Monash Institute of Medical Research, Clayton, Victoria 3168, Australia, the hDepartment of Medical Biology -

Low Abundance of the Matrix Arm of Complex I in Mitochondria Predicts Longevity in Mice
ARTICLE Received 24 Jan 2014 | Accepted 9 Apr 2014 | Published 12 May 2014 DOI: 10.1038/ncomms4837 OPEN Low abundance of the matrix arm of complex I in mitochondria predicts longevity in mice Satomi Miwa1, Howsun Jow2, Karen Baty3, Amy Johnson1, Rafal Czapiewski1, Gabriele Saretzki1, Achim Treumann3 & Thomas von Zglinicki1 Mitochondrial function is an important determinant of the ageing process; however, the mitochondrial properties that enable longevity are not well understood. Here we show that optimal assembly of mitochondrial complex I predicts longevity in mice. Using an unbiased high-coverage high-confidence approach, we demonstrate that electron transport chain proteins, especially the matrix arm subunits of complex I, are decreased in young long-living mice, which is associated with improved complex I assembly, higher complex I-linked state 3 oxygen consumption rates and decreased superoxide production, whereas the opposite is seen in old mice. Disruption of complex I assembly reduces oxidative metabolism with concomitant increase in mitochondrial superoxide production. This is rescued by knockdown of the mitochondrial chaperone, prohibitin. Disrupted complex I assembly causes premature senescence in primary cells. We propose that lower abundance of free catalytic complex I components supports complex I assembly, efficacy of substrate utilization and minimal ROS production, enabling enhanced longevity. 1 Institute for Ageing and Health, Newcastle University, Newcastle upon Tyne NE4 5PL, UK. 2 Centre for Integrated Systems Biology of Ageing and Nutrition, Newcastle University, Newcastle upon Tyne NE4 5PL, UK. 3 Newcastle University Protein and Proteome Analysis, Devonshire Building, Devonshire Terrace, Newcastle upon Tyne NE1 7RU, UK. Correspondence and requests for materials should be addressed to T.v.Z.