Update on Liposuction: Clinical Pearls
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Weight Management Guideline: Children and Adolescents
Weight Management in Children and Adolescents Screening and Intervention Guideline Prevention ........................................................................................................................................ 2 Nutrition ........................................................................................................................................ 2 Healthy eating behaviors .............................................................................................................. 2 Physical activity ............................................................................................................................ 3 Screening ......................................................................................................................................... 3 Diagnosis.......................................................................................................................................... 3 Interventions ..................................................................................................................................... 4 Goals ............................................................................................................................................ 4 Strategies to help with weight loss ............................................................................................... 5 Behavior change counseling using the 5A approach ................................................................... 5 Lifestyle modifications ................................................................................................................. -

Role of Body Fat and Body Shape on Judgment of Female Health and Attractiveness: an Evolutionary Perspective
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Psychological Topics 15 (2006), 2, 331-350 Original Scientific Article – UDC 159.9.015.7.072 572.51-055.2 Role of Body Fat and Body Shape on Judgment of Female Health and Attractiveness: An Evolutionary Perspective Devendra Singh University of Texas at Austin Department of Psychology Dorian Singh Oxford University Department of Social Policy and Social Work Abstract The main aim of this paper is to present an evolutionary perspective for why women’s attractiveness is assigned a great importance in practically all human societies. We present the data that the woman’s body shape, or hourglass figure as defined by the size of waist-to-hip-ratio (WHR), reliably conveys information about a woman’s age, fertility, and health and that systematic variation in women’s WHR invokes systematic changes in attractiveness judgment by participants both in Western and non-Western societies. We also present evidence that attractiveness judgments based on the size of WHR are not artifact of body weight reduction. Then we present cross-cultural and historical data which attest to the universal appeal of WHR. We conclude that the current trend of describing attractiveness solely on the basis of body weight presents an incomplete, and perhaps inaccurate, picture of women’s attractiveness. “... the buttocks are full but her waist is narrow ... the one for who[m] the sun shines ...” (From the tomb of Nefertari, the favorite wife of Ramses II, second millennium B.C.E.) “... By her magic powers she assumed the form of a beautiful woman .. -
Understanding 7 Understanding Body Composition
PowerPoint ® Lecture Outlines 7 Understanding Body Composition Copyright © 2009 Pearson Education, Inc. Objectives • Define body composition . • Explain why the assessment of body size, shape, and composition is useful. • Explain how to perform assessments of body size, shape, and composition. • Evaluate your personal body weight, size, shape, and composition. • Set goals for a healthy body fat percentage. • Plan for regular monitoring of your body weight, size, shape, and composition. Copyright © 2009 Pearson Education, Inc. Body Composition Concepts • Body Composition The relative amounts of lean tissue and fat tissue in your body. • Lean Body Mass Your body’s total amount of lean/fat-free tissue (muscles, bones, skin, organs, body fluids). • Fat Mass Body mass made up of fat tissue. Copyright © 2009 Pearson Education, Inc. Body Composition Concepts • Percent Body Fat The percentage of your total weight that is fat tissue (weight of fat divided by total body weight). • Essential Fat Fat necessary for normal body functioning (including in the brain, muscles, nerves, lungs, heart, and digestive and reproductive systems). • Storage Fat Nonessential fat stored in tissue near the body’s surface. Copyright © 2009 Pearson Education, Inc. Why Body Size, Shape, and Composition Matter Knowing body composition can help assess health risks. • More people are now overweight or obese. • Estimates of body composition provide useful information for determining disease risks. Evaluating body size and shape can motivate healthy behavior change. • Changes in body size and shape can be more useful measures of progress than body weight. Copyright © 2009 Pearson Education, Inc. Body Composition for Men and Women Copyright © 2009 Pearson Education, Inc. -

Underweight and Difficulty Gaining Weight
Nutrition Fact sheet Underweight and Difficulty Gaining Weight Maintaining a healthy body weight is important for good health, but every person’s energy needs are different, depending on their activity levels. Ultimately, the “energy in” from food each day must be balanced with the “energy out” expended through exercise and activity. For people with physical Challenges Gaining and disabilities, energy needs are Maintaining Weight often related to ability. For Some children with disabilities example, people who use a have difficulty gaining weight wheelchair tend to have less and may be underweight for energy needs than those who Reasons for not getting their height and age. This walk. People with spasticity the right amount of food can continue into adulthood, type cerebral palsy tend to include: with some people struggling have less energy needs than to gain weight and maintain • Difficulties with eating and those with athetosis. a healthy body weight their drinking Dietitian reviews are entire lives. • Inability to express hunger recommended for any person Low body weight can lead to: or thirst at risk of being either over – • Requiring assistance with or underweight. Reviews will • Growth failure in children eating and drinking assist you to determine the • Decreased muscle strength most suitable foods to meet • Reflux, vomiting or • Reduced ability to cough your needs. aspiration (food and drink • Increased risk of infection going into the lungs) • Constipation • Requiring food textures to • Osteoporosis be changed before eating • Pressure injury or drinking • Irritability • Lack of appetite • Depression • Taking a long time to eat and drink There are two general causes • Constipation of low body weight: a lack of correct nutrition to gain and maintain weight; and more energy being expended than is being taken in. -

Relationship Between Body Image and Body Weight Control in Overweight ≥55-Year-Old Adults: a Systematic Review
International Journal of Environmental Research and Public Health Review Relationship between Body Image and Body Weight Control in Overweight ≥55-Year-Old Adults: A Systematic Review Cristina Bouzas , Maria del Mar Bibiloni and Josep A. Tur * Research Group on Community Nutrition and Oxidative Stress, University of the Balearic Islands & CIBEROBN (Physiopathology of Obesity and Nutrition CB12/03/30038), E-07122 Palma de Mallorca, Spain; [email protected] (C.B.); [email protected] (M.d.M.B.) * Correspondence: [email protected]; Tel.: +34-971-1731; Fax: +34-971-173184 Received: 21 March 2019; Accepted: 7 May 2019; Published: 9 May 2019 Abstract: Objective: To assess the scientific evidence on the relationship between body image and body weight control in overweight 55-year-old adults. Methods: The literature search was conducted ≥ on MEDLINE database via PubMed, using terms related to body image, weight control and body composition. Inclusion criteria were scientific papers, written in English or Spanish, made on older adults. Exclusion criteria were eating and psychological disorders, low sample size, cancer, severe diseases, physiological disorders other than metabolic syndrome, and bariatric surgery. Results: Fifty-seven studies were included. Only thirteen were conducted exclusively among 55-year-old ≥ adults or performed analysis adjusted by age. Overweight perception was related to spontaneous weight management, which usually concerned dieting and exercising. More men than women showed over-perception of body image. Ethnics showed different satisfaction level with body weight. As age increases, conformism with body shape, as well as expectations concerning body weight decrease. Misperception and dissatisfaction with body weight are risk factors for participating in an unhealthy lifestyle and make it harder to follow a healthier lifestyle. -

Chapter 10. the Interplay of Genes, Lifestyle, and Obesity
CHAPTER 10. The interplay of genes, lifestyle, and obesity Paul W. Franks CHAPTER 10 CHAPTER This chapter reviews the evi- long term [1]. Success in pharmaco- marketed for treatment of diabetes: dence supporting a joint effect of therapeutics for weight loss has also (i) metformin, which reduces hepatic genes and lifestyle factors in obesi- been meagre, and in some instances gluconeogenesis (the production of ty, focusing mainly on evidence from disastrous. A handful of anti-obesity glucose in the liver); (ii) sodium-glu- epidemiological studies and clinical medications have been approved cose linked transporter 2 (SGLT2) trials research. by the European Medicines Agency inhibitors, such as empagliflozin, Obesity is the scourge of most (EMA) and the United States Food which reduce re-uptake of glucose contemporary societies; about 40% and Drug Administration (FDA). One in the kidneys and are diuretic; and of adults worldwide are overweight of the most successful of these is (iii) glucagon-like peptide-1 (GLP-1) and 13% are obese (http://www.who. the lipase inhibitor orlistat. Howev- agonists, such as exenatide, which int/mediacentre/factsheets/fs311/ er, because orlistat diminishes in- diminish appetite by delaying gastric en/). Much of the burden that obesity testinal fat absorption, a frequent emptying. However, because all of conveys arises from the life-threat- side-effect of the drug is fatty stool, these drugs can cause side-effects ening diseases it causes, although which many patients cannot toler- and they are not all reimbursable by there are also direct consequences, ate. Other weight-loss drugs, such health insurance providers for treat- because quality of life is often dimin- as rimonabant, are approved for use ment of obesity, they are rarely used ished in people with morbid obesity in the European Union but are not primarily for weight reduction. -

Physical Activity Reduces Compensatory Weight Gain After Liposuction 13 June 2012
Physical activity reduces compensatory weight gain after liposuction 13 June 2012 Abdominal liposuction triggers a compensatory possible compensatory visceral fat growth and the increase in visceral fat, which is correlated with potential health risks associated with a liposuction cardiovascular disease, but this effect can be procedure," said Benatti. "Additionally, health counteracted by physical activity, according to a professionals are encouraged to recommend recent study in the Journal of Clinical exercise training as an intervention following Endocrinology and Metabolism, a publication of liposuction surgery." The Endocrine Society. More information: The original article, Liposuction is one of the most popular aesthetic "Liposuction Induces a Compensatory Increase of surgery procedures performed worldwide, but its Visceral Fat which Is Effectively Counteracted by long-term impact on health remains unclear. Physical Activity: A Randomized Trial" appears in Previous studies have shown that the immediate the July 2012 issue of JCEM. decrease in body fat following liposuction may affect body composition and metabolic profile by triggering feedback mechanisms of body fat regain. The current study investigated the effects of Provided by The Endocrine Society liposuction on body fat distribution and whether physical activity could prevent fat regain. "We found that removing adipose tissue from the body, as liposuction does, may result in a decrease in total energy expenditure and compensatory growth of visceral fat which is associated with heart disease," said Fabiana Braga Benatti, PhD, of the University of Sao Paulo in Brazil and lead author of the study. "The good news is that exercise training was effective in counteracting this compensatory growth. If someone chooses to undergo liposuction, it is very important, if not essential, that this person exercises after the surgery." In this study 36 healthy women underwent a small- volume liposuction of the abdomen. -

Promoting Healthy Weight
Promoting Healthy Weight Maintaining a healthy weight during childhood Definitions and Terminology and adolescence is critically important for chil- dren’s and adolescents’ overall health and well- Body mass index (BMI) is defined as weight (kilo- being, as well as for good health in adulthood. A grams) divided by the square of height (meters): 2 child’s or adolescent’s weight status is the result weight (kg)/[height (m)] . Although BMI does not of multiple factors working together—heredity, directly measure body fat, it is a useful screening metabolism, height, behavior, and environment.1 tool because it correlates with body fat and health 2 HEAL PROMOTING Two of the most important behavioral determi- risks. Additionally, measuring BMI is clinically nants are nutrition and physical activity. How feasible. In children and adolescents, BMI distribu- much and what a child or adolescent eats and tion, like weight and height distributions, changes the types and intensity of physical activity she with age. As a result, while BMI is appropriate to categorize body weight in adults, BMI percentiles participates in can affect weight and therefore T overall health. A balanced, nutritious diet and specific for age and sex from reference populations WE HY define underweight, healthy weight, overweight, regular physical activity are keys to preventing IG overweight and obesity. and obesity in children and adolescents. H T Underweight is an issue for some children and Body mass index is recommended as one of sev- adolescents, including some children and youth eral screening tools for assessing weight status. For with special health care needs and some adolescents individual children and adolescents, health care with eating disorders, but the overriding concern professionals need to review growth patterns, fam- with weight status in the United States today is over- ily histories, and medical conditions to assess risk weight and obesity. -

Refining the Abdominoplasty for Better Patient Outcomes
Refining the Abdominoplasty for Better Patient Outcomes Karol A Gutowski, MD, FACS Private Practice University of Illinois & University of Chicago Refinements • 360o assessment & treatment • Expanded BMI inclusion • Lipo-abdominoplasty • Low scar • Long scar • Monsplasty • No “dog ears” • No drains • Repurpose the fat • Rapid recovery protocols (ERAS) What I Do and Don’t Do • “Standard” Abdominoplasty is (almost) dead – Does not treat the entire trunk – Fat not properly addressed – Problems with lateral trunk contouring – Do it 1% of cases • Solution: 360o Lipo-Abdominoplasty – Addresses entire trunk and flanks – No Drains & Rapid Recovery Techniques Patient Happy, I’m Not The Problem: Too Many Dog Ears! Thanks RealSelf! Take the Dog (Ear) Out! Patients Are Telling Us What To Do Not enough fat removed Not enough skin removed Patient Concerns • “Ideal candidate” by BMI • Pain • Downtime • Scar – Too high – Too visible – Too long • Unnatural result – Dog ears – Mons aesthetics Solutions • “Ideal candidate” by BMI Extend BMI range • Pain ERAS protocols + NDTT • Downtime ERAS protocols + NDTT • Scar Scar planning – Too high Incision markings – Too visible Scar care – Too long Explain the need • Unnatural result Technique modifications – Dog ears Lipo-abdominoplasty – Mons aesthetics Mons lift Frequent Cause for Reoperation • Lateral trunk fullness – Skin (dog ear), fat, or both • Not addressed with anterior flank liposuction alone – need posterior approach • Need a 360o approach with extended skin excision (Extended Abdominoplasty) • Patient -
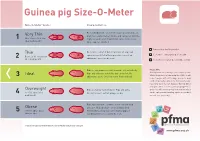
Guinea Pig Size-O-Meter Will 3 Abdominal Curve
Guinea pig Size-O- Meter Size-O-Meter Score: Characteristics: Each individual rib can be felt easily, hips and spine are Very Thin prominent and extremely visible and can be felt with the 1 More than 20% below slightest touch. Under abdominal curve can be seen. ideal body weight Spine appears hunched. Your pet is a healthy weight Thin Each rib is easily felt but not prominent. Hips and spine are easily felt with no pressure. Less of an Seek advice about your pet’s weight Between 10-20% below 2 abdominal curve can be seen. ideal body weight Seek advice as your pet could be at risk Ribs are not prominent and cannot be felt individually. Please note Hips and spine are not visible but can be felt. No Getting hands on is the key to this simple system. Ideal Whilst the pictures in Guinea pig Size-O-Meter will 3 abdominal curve. Chest narrower then hind end. help, it may be difficult to judge your pet’s body condition purely by sight alone. Some guinea pigs have long coats that can disguise ribs, hip bones and spine, while a short coat may highlight these Overweight Ribs are harder to distinguish. Hips and spine areas. You will need to gently feel your pet which 4 10 -15% above ideal difficult to feel. Feet not always visible. can be a pleasurable bonding experience for both body weight you and your guinea pig. Ribs, hips and spine cannot be felt or can with mild Obese pressure. No body shape can be distinguished. -

Treatment of Childhood Overweight and Obesity
June 2020 Michigan Quality Improvement Consortium Guideline Treatment of Childhood Overweight and Obesity The following guideline recommends specific treatment interventions for childhood overweight and obesity. Eligible Population Key Components Recommendation and Level of Evidence Frequency Children 2 years or Identify presence Reinforce Prevention Recommendations (See MQIC Prevention and Identification of Childhood Overweight Each periodic older with a BMI ≥ of weight-related and Obesity guideline) health exam, 85th percentile risk factors and History and physical exam [D]: more complications Pulse and blood pressure (≥ 3 years), using appropriate technique and cuff size for age. frequently as Family history, social determinants/influencers (healthy food access, safe neighborhood for physical activity), case requires patient or parental concern about weight, dietary patterns (e.g. frequency of eating outside the home, consumption of breakfast, adequate fruits and vegetables, excessive portion sizes, etc.), physical activity level, sleep patterns, and history of medication use. Consider Symptoms of diabetes, hypothyroidism, digestive disorders, gallbladder disease, obstructive sleep disorders, management weight-related orthopedic problems, depression and anxiety, or other mental health concerns, etc. of childhood Be alert to secondary causes of obesity and consider genetic, endogenous, or syndrome-associated causes obesity as a long- of obesity. term intervention Reinforce lifestyle and behavior modifications [D]: Focus on slowing the child's rate of weight gain and maintaining or lowering their BMI percentile. Family must recognize the problem and be actively engaged in the treatment. Small, gradual lifestyle changes are recommended. Promote a healthy diet and lifestyle with focus on 5-2-1-0: ≥ 5 fruits and vegetables, ≤ 2 hours recreational screen time, ≥ 1 hour physical activity, 0 sugar-containing drinks, daily. -

5.2 Recommendations for Preventing Excess Weight Gain and Obesity
5.2 Recommendations for preventing excess weight gain and obesity 5.2.1 Background Almost all countries (high-income and low-income alike) are experien- cing an obesity epidemic, although with great variation between and within countries. In low-income countries, obesity is more common in middle-aged women, people of higher socioeconomic status and those living in urban communities. In more affluent countries, obesity is not only common in the middle-aged, but is becoming increasingly prevalent among younger adults and children. Furthermore, it tends to be associated with lower socioeconomic status, especially in women, and the urban--rural differences are diminished or even reversed. It has been estimated that the direct costs of obesity accounted for 6.8% (or US$ 70 billion) of total health care costs, and physical inactivity for a further US$ 24 billion, in the United States in 1995. Although direct costs in other industrialized countries are slightly lower, they still consume a sizeable proportion of national health budgets (1). Indirect costs, which are far greater than direct costs, include workdays lost, physician visits, disability pensions and premature mortality. Intangible costs such as impaired quality of life are also enormous. Because the risks of diabetes, cardiovascular disease and hypertension rise continuously with increas- ing weight, there is much overlap between the prevention of obesity and the prevention of a variety of chronic diseases, especially type 2 diabetes. Population education strategies will need a solid base of policy and environment-based changes to be effective in eventually reversing these trends. 5.2.2 Trends The increasing industrialization, urbanization and mechanization occurring in most countries around the world is associated with changes in diet and behaviour, in particular, diets are becoming richer in high-fat, high energy foods and lifestyles more sedentary.