Standards of Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protocol V8, Dated 21 Aug 2017 Page 1 Regenerative Endodontic Therapy
Regenerative Endodontic Therapy (RET) using Antibiotic pastes or Calcium Hydroxide disinfection for the management of immature non-vital permanent teeth in children: A Randomized Controlled Clinical Trial Principal investigator: Dr Tong Huei Jinn Discipline of Orthodontics and Paediatric Dentistry Faculty of Dentistry, National University of Singapore Site Principal Investigator: Dr Lim Wan Yi School Dental Service Health Promotion Board Co-Investigators: Dr Victoria Yu Discipline of Operative Dentistry, Endodontics & Prosthodontics Faculty of Dentistry, National University of Singapore Dr Tang Kok Siew Discipline of Orthodontics and Paediatric Dentistry Faculty of Dentistry, National University of Singapore Dr Ode Wataru Discipline of Operative Dentistry, Endodontics & Prosthodontics Faculty of Dentistry, National University of Singapore Dr Ivan Koh Chee Keong Discipline of Operative Dentistry, Endodontics & Prosthodontics Faculty of Dentistry, National University of Singapore Protocol V8, Dated 21 Aug 2017 Page 1 Dr Eu Oy Chu, BDS, MSc School Dental Service Health Promotion Board Dr Melissa Tan Hui Xian, School Dental Service Health Promotion Board Protocol V8, Dated 21 Aug 2017 Page 2 1.0 Background The management of immature non-vital teeth following trauma or pulpal infection secondary to caries or dental anomalies e.g. fractured dens evaginatus tubercles is a challenge for dentists. Traditionally, the treatment prescribed for immature non-vital teeth is to thoroughly disinfect the root canal system and perform apexification procedures using materials such as Ca(OH)2 or Mineral Trioxide Aggregate (MTA), followed by filling the root canal with gutta-percha. This technique however does not produce increased thickness of dentine or gain in root length to the immature tooth. -

Different Approaches to the Regeneration of Dental Tissues in Regenerative Endodontics
applied sciences Review Different Approaches to the Regeneration of Dental Tissues in Regenerative Endodontics Anna M. Krupi ´nska 1 , Katarzyna Sko´skiewicz-Malinowska 2 and Tomasz Staniowski 2,* 1 Department of Prosthetic Dentistry, Wroclaw Medical University, 50-367 Wrocław, Poland; [email protected] 2 Department of Conservative Dentistry and Pedodontics, Wroclaw Medical University, 50-367 Wrocław, Poland; [email protected] * Correspondence: [email protected] Abstract: (1) Background: The regenerative procedure has established a new approach to root canal therapy, to preserve the vital pulp of the tooth. This present review aimed to describe and sum up the different approaches to regenerative endodontic treatment conducted in the last 10 years; (2) Methods: A literature search was performed in the PubMed and Cochrane Library electronic databases, supplemented by a manual search. The search strategy included the following terms: “regenerative endodontic protocol”, “regenerative endodontic treatment”, and “regenerative en- dodontics” combined with “pulp revascularization”. Only studies on humans, published in the last 10 years and written in English were included; (3) Results: Three hundred and eighty-six potentially significant articles were identified. After exclusion of duplicates, and meticulous analysis, 36 case reports were selected; (4) Conclusions: The pulp revascularization procedure may bring a favorable outcome, however, the prognosis of regenerative endodontics (RET) is unpredictable. Permanent immature teeth showed greater potential for positive outcomes after the regenerative procedure. Citation: Krupi´nska,A.M.; Further controlled clinical studies are required to fully understand the process of the dentin–pulp Sko´skiewicz-Malinowska,K.; complex regeneration, and the predictability of the procedure. -

Summarizing the Applications and Limitations of Cone Beam Computed Tomography – a Review
European Journal of Molecular & Clinical Medicine ISSN 2515-8260 Volume 07, Issue 5, 2020 SUMMARIZING THE APPLICATIONS AND LIMITATIONS OF CONE BEAM COMPUTED TOMOGRAPHY – A REVIEW Running Title: Cone Beam Computed Tomography-a review Arunajatesan Subbiya 1 , G S V Nivashini 2 , Ramachandran Tamilselvi 3 , Dhakshinamoorthy Malarvizhi 4 M.D.S., Professor & Head1, B.D.S., First yr Postgraduate student2, M.D.S, Reader3, M.D.S, Professor 4 , Department of Conservative Dentistry and Endodontics,, Sree Balaji Dental College and Hospital, Bharath Institute of Higher Education and Research,, Narayanapuram , Pallikaranai,Chennai -600100. Tamilnadu, India. Corresponding Author: G S V Nivashini., M.D.S., Postgraduate student Address: Department of Conservative dentistry and endodontics, Sree Balaji dental college and hospital, Bharath institute of higher education and research, Narayanapuram, Pallikaranai, Chennai – 600 100 Tamil nadu, India. ABSTRACT Cone Beam Computed Tomography (CBCT) has progressed over 15-20 years from being a technique with great potential to one that has become primary diagnostic investigation. 3D imaging has made complex root canal anatomies more accessible and helps in accurate treatment planning for many endodontic problems. A modification of original cone beam algorithm was developed by Feldkamp et al in 1984[1]. Since then there were significant progress in imaging technique starting from linear to hypocycloidal tomographic movements wherein the centre of rotation remains the same and movement of the equipment becomes more complicated for better resolution. The goal of this article is to summarize theapplications and limitations of CBCT in various clinical scenarios in day to day endodontic practice. Keywords : Radiation, imaging modalities, periapical pathosis, vertical root fractures, regenerative endodontics. -

Restorative Dentistry & Endodontics
pISSN 2234-7658 Vol. 44 · Supplement · November 2019 eISSN 2234-7666 November 8–10, 2019 · Coex, Seoul, Korea Restorative DentistryRestorative & Endodontics Restorative Dentistry & Endodontics Vol. 44 Vol. · Supplement Supplement · November 2019 November The Korean Academy of Conservative Dentistry Academy The Korean The Korean Academy of Conservative Dentistry www.rde.ac Vol. 44 · Supplement · November 2019 Restorative Dentistry & Endodontics November 8–10, 2019 · Coex, Seoul, Korea pISSN: 2234-7658 eISSN: 2234-7666 Aims and Scope Distribution Restorative Dentistry and Endodontics (Restor Dent Endod) is a Restor Dent Endod is not for sale, but is distributed to members peer reviewed and open-access electronic journal providing up- of Korean Academy of Conservative Dentistry and relevant to-date information regarding the research and developments researchers and institutions world-widely on the last day of on new knowledge and innovations pertinent to the field of February, May, August, and November of each year. Full text PDF contemporary clinical operative dentistry, restorative dentistry, files are also available at the official website (https://www.rde. and endodontics. In the field of operative and restorative ac; http://www.kacd.or.kr), KoreaMed Synapse (https://synapse. dentistry, the journal deals with diagnosis, treatment planning, koreamed.org), and PubMed Central. To report a change of treatment concepts and techniques, adhesive dentistry, esthetic mailing address or for further information contact the academy dentistry, tooth whitening, dental materials and implant office through the editorial office listed below. restoration. In the field of endodontics, the journal deals with a variety of topics such as etiology of periapical lesions, outcome Open Access of endodontic treatment, surgical endodontics including Article published in this journal is available free in both print replantation, transplantation and implantation, dental trauma, and electronic form at https://www.rde.ac, https://synapse. -

ABGD Board Review Questions 2013 Endodontics
ABGD Board Review Questions 2013 Endodontics 1. EDTA or ethylenediaminetetraacetic acid is a chelating agent. What else does it help to do in canal preparation? A. Removes potassium ions to make tooth less sensitive post op B. Removes the inorganic portion of the smear layer C. Removes the organic portion of the smear layer D. Kills bacteria and digests organic debris Answer - B With its ability to chelate inorganic material, it removes minerals from the smear layer while NaOCl digests organic material from the smear layer, kills bacteria, and digests organic debris. EDTA is available in liquid or paste form and is used in concentrations from 15-17%. It is usually combined with a detergent to decrease the surface tension and increase the cleaning ability as well as wetability of the dentin surface. To remove the smear layer the EDTA needs to be left in place for 1-5 minutes and then rinsed out of the tooth with water or NaOCl. Nygaard-Ostby in 1957 introduced chelating agents to endodontics for the treatment of narrow calcified canal systems. It allows for an easier cutting of the calcified dentin and its removal to aide in treatment. Source: Johnson WT, Gutmann JL; Ch. 10 Obturation of the Cleaned and Shaped Root Canal System; Pathways of the Pulp; Mosby Publishing, St. Louis, MO, 2006; pp. 366-367. 2. When using EDTA, one must factor in which variables to evaluate its effectiveness: A. Time of application B. pH C. Concentration D. Location of EDTA – coronal/middle/apical third of root canal E. All the above Answer – E The effectiveness of EDTA is related to time of application, the pH, and the concentration. -

Regenerative Pulpotomy As a Novel
Mobarak et al. DOI: 10.21608/ADJALEXU.2020.23924.1046 REGENERATIVE PULPOTOMY AS A NOVEL TECHNIQUE FOR TREATMENT OF PERMANENT MATURE MOLARS DIAGNOSED WITH IRREVERSIBLE PULPITIS USING PLATELET-RICH FIBRIN: A CASE SERIES STUDY 1* BDs MSc, 2 BDs MSc PhD, 3,4 BDs MSc PhD, Ahmed M. Mobarak Salma MH. Genena Ashraf M. Zaazou 5 4 Nayera A. Mokhless BDs MSc PhD, Sybel M. Moussa BDs MSc PhD. ABSTRACT INTRODUCTION: Management of teeth with clinical signs/symptoms suggestive of irreversible pulpitis was conventionally invasive, but the emerging evidence suggested successful treatment outcome using the less invasive vital pulp procedures such as coronal pulpotomy, leading to preservation of the remaining pulp in a vital and functioning state. OBJECTIVES: Evaluation of the clinical/radiographic success of novel regenerative coronal pulpotomy technique using Platelet-Rich Fibrin (PRF) and Biodentine. MATERIALS AND METHODS: Three irreversibly inflamed permanent molars with mature roots in three patients were treated by regenerative pulpotomy technique. Access openings were done, and coronal pulps were removed to the level of root canal orifices. Hemostasis in all teeth were done by the compression with cotton pellets moistened with 2.5 % sodium hypochlorite (NaOCl). PRF membranes were prepared by drawing 10 ml of patients’ own blood, then they were immediately centrifuged using a table top centrifuge at 400 gforce for 12mins. The PRF membranes were placed over the remaining radicular pulps followed by Biodentine preparation and placement over the PRF. The cavities were then immediately restored. Patients were scheduled for clinical/radiographic evaluations after three-, six- and 12-months. RESULTS: Throughout the follow-up periods, the three teeth demonstrated clinical/radiographic success with complete resolution of clinical signs/symptoms. -

Non-Surgical Endodontics
UnitedHealthcare® Dental Coverage Guideline Non-Surgical Endodontics Guideline Number: DCG009.07 Effective Date: February 1, 2021 Instructions for Use Table of Contents Page Related Dental Policy Coverage Rationale ....................................................................... 1 • Surgical Endodontics Definitions ...................................................................................... 3 Applicable Codes .......................................................................... 4 Description of Services ................................................................. 5 References ..................................................................................... 5 Guideline History/Revision Information ....................................... 5 Instructions for Use ....................................................................... 6 Coverage Rationale Vital Pulp Therapy Direct Pulp Cap Direct Pulp Capping is indicated for permanent teeth for the following: Tooth has a vital pulp or been diagnosed with reversible pulpitis All caries has been removed Mechanical exposure of a clinically vital and asymptomatic pulp occurs If bleeding can be controlled at the site of exposure Indirect Pulp Cap Indirect Pulp Capping is indicated for primary teeth or permanent teeth with immature apices for the following: Tooth has a vital pulp or been diagnosed with reversible pulpitis Tooth has a deep carious lesion that is considered likely to result in pulp exposure during excavation Therapeutic Pulpotomy Therapeutic Pulpotomy -

Pulp Revascularization: an Alternative Treatment to the Apexification of Immature Teeth
http://dx.doi.org/10.1590/1981-8637201400040000082673 REVISÃO | REVIEW Pulp revascularization: an alternative treatment to the apexification of immature teeth Revascularização pulpar: tratamento alternativo à apicificação de dentes jovens com rizogênese incompleta Maria Tereza Pedrosa ALBUQUERQUE1 Juliana Yuri NAGATA2 Adriana de Jesus SOARES2 Alexandre Augusto ZAIA2 ABSTRACT Pulp revascularization can be considered as a current alternative treatment to apexification, recommended for immature teeth cases, requiring endodontic treatment. Apexification involves long-term periodic exchanges of a calcium hydroxide paste into the root canal to induce the formation of a calcified barrier. Despite being the most classically therapy employed for these cases, the permanence of calcium hydroxide for long periods of time and also the successive changes may lead to a weakening of the root due to its hygroscopic properties and the proteolytic activities of calcium hydroxide, increasing the risk of fractures and contamination of the pulp space. Thus, a constant search for new treatment alternatives that provide the end of root development have been done to avoid the risk of future root fractures. So, revascularization has emerged as a new treatment option for cases of undeveloped teeth, that provides not only apical closure, as apexification, but also increase the dentin walls thickness. In the literature, there is an assortment of treatment protocols employing pulp revascularization procedure in attempt to attain the best way to achieve success. Assuming the diversity of protocols for revascularization treatment, it is important to go deep in the literature to collect, describe and discuss these protocols guiding new researches in this field and also conducting the clinicians. -

Regenerative Endodontics for Upper Permanent Central Incisors After Traumatic Injury: Case Report with a 3-Year Follow-Up Loai Alsofi
CASE REPORT Regenerative Endodontics for Upper Permanent Central Incisors after Traumatic Injury: Case Report with a 3-year Follow-up Loai Alsofi ABSTRACT Aim: The aim of this article is to describe a one-visit approach to attempt revascularization in the upper right and left central incisors after traumatic injury. Background: A single-visit conservative revascularization approach can be used to promote root growth and maturation following traumatic dental injury and loss of pulpal tissues. Case description: An eight-year-old female patient presented in Dentalia Clinics, Jeddah, Kingdom of Saudi Arabia, in 2016 with traumatic dental injury. Upon clinical and radiographic examination, it was found that the trauma resulted in loss of pulp vitality in two upper central incisors. Local anesthesia was administered, and a rubber dam was placed. Access cavity was done for each tooth separately. 2% chlorhexidine followed by sterile saline was used for irrigation with no instrumentation. Mineral trioxide aggregate (MTA) was used as the sealing material after blood clot formation. Follow-up showed continuous root maturation in the right central incisor, at 6 months, one year, two years, and three years. Root canal treatment was done in 2019 due to the development of periapical lesion. The 6-month follow-up radiograph also showed loss of the crown of the left central incisor due to a second trauma with retained apical root fragment. The fragment was embedded inside the bone and showed continuous maturation during the three years. Conclusion: A single-visit regenerative endodontic approach showed successful results in revascularizing the upper permanent central incisor after loss of pulpal tissue. -

Pulp Therapy for Primary and Immature Permanent Teeth
BEST PRACTICES: PULP THERAPY Pulp Therapy for Primary and Immature Permanent Teeth Latest Revision How to Cite: American Academy of Pediatric Dentistry. Pulp therapy 2020 for primary and immature permanent teeth. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry; 2020:384-92. Purpose as: normal pulp (symptom free and normally responsive to The American Academy of Pediatric Dentistry AAPD( ) intends vitality testing), reversible pulpitis (pulp is capable of healing), these recommendations to aid in the diagnosis of pulp health symptomatic or asymptomatic irreversible pulpitis (vital versus pathosis and to set forth the indications, objectives, inflamed pulp is incapable of healing), or necrotic pulp.3 The and therapeutic interventions for pulp therapy in primary and clinical diagnosis derived from:4-7 immature permanent teeth. 1. a comprehensive medical history. 2. a review of past and present dental history and Methods treatment, including current symptoms and chief Recommendations on pulp therapy for primary and immature complaint. permanent teeth were developed by the Clinical Affairs 3. a subjective evaluation of the area associated with the Committee – Pulp Therapy Subcommittee and adopted in current symptoms/chief complaint by questioning 1991.1 This document by the Council of Clinical Affairs is the patient/parent on the location, intensity, a revision of the previous version, last revised in 2014.2 This duration, stimulus, relief, and spontaneity. revision included a new search of the PubMed / 4. an objective extraoral examination as well as examina- MEDLINE database using the terms: pulpotomy, pulpectomy,® tion of the intraoral soft and hard tissues. pulpectomy primary teeth, indirect pulp treatment (IPT), 5. -

Vital Primary Molars
tistr Den y Rawi, Dentistry 2018, 8:1 Dentistry DOI: 10.4172/2161-1122.1000468 ISSN: 2161-1122 Research Article Open Access A New Era in Treatment of Non – Vital Primary Molars: One Year Follow-up Study Baydaa Rawi* Pediatric Dentistry, Dean of College of Dentistry, Ibn Sina University of Medical and Pharmaceutical Sciences, Iraq *Corresponding author: Baydaa Rawi, PhD, Assistant Professor, Pediatric Dentistry, Dean of College of Dentistry, Ibn Sina University of Medical and Pharmaceutical Sciences, Iraq, Tel: 009647730233399; E-mail: [email protected] Received date: December 01, 2017; Accepted date: December 29, 2017; Published date: January 05, 2018 Copyright: © 2018 Rawi B. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background: Pulpectomy is a root canal procedure for pulp tissue that is irreversibly infected or necrotic due to caries or trauma. Aims: The aim of this study is to apply blood clot technique for non-vital deciduous molars. Clinical and radiographical evaluations were carried out after 6 and 12 months. Materials and Methods: Forty non vital primary molars from twenty children were involved in this study. The root canals are disinfected using triple antibiotic paste. Resembling to blood clot techniques carried out for non vital immature permanent tooth, blood clot created in root canal by by over instrumentation, and put sterile cotton pellet at the canal orifice wait 5 min for blood to clot. MTA barrier placed over blood clot about over the root orifices. -
Stem Cell-Based Regenerative Endodontics
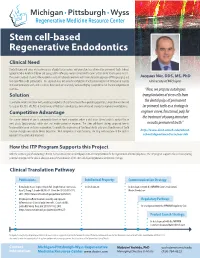
Stem cell-based Regenerative Endodontics Clinical Need .......................................................................................................................................................................................................................................... Dental trauma and caries are leading causes of pulp tissue necrosis and premature loss of immature permanent teeth. Indeed, approximately 5.4 million children and young adults suffer pulp necrosis associated to caries and/or dental trauma yearly in USA. The current standard of care for these patients is calcium hydroxide treatment with mineral trioxide aggregate (MTA) apical plug and Jacques Nör, DDS, MS, PhD root canal filling with gutta-percha. This approach does not allow for completion of vertical and lateral root formation in necrotic University of Michigan immature permanent teeth, and as a result, these teeth are structurally weak and highly susceptible to root fracture and premature tooth loss. “Here, we propose autologous Solution transplantation of stem cells from .......................................................................................................................................................................................................................................... To revitalize necrotic immature teeth, enabling completion of root formation in these pediatric population, a team of researchers led the dental pulps of permanent by Jacques Nör, DDS, MS, PhD, at the University of Michigan is developing a stem cell-based